Endovenous Ablation
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about endovenous ablation:
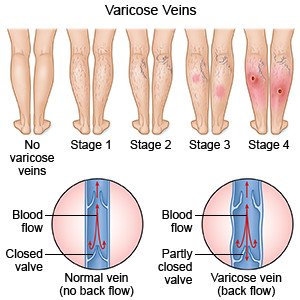
Endovenous ablation is a procedure that uses radiofrequency or laser energy to treat varicose veins. Varicose veins are large, twisted veins in your legs that bulge out under your skin. Endovenous ablation may help treat pain, discolored skin, or ulcers in your leg that are caused by varicose veins.
 |
How to prepare for endovenous ablation:
- Your healthcare provider will talk to you about how to prepare for your procedure. He or she may tell you not to eat or drink anything several hours before your procedure. He or she will tell you which medicines to take or not take on the day of your procedure. You may need to stop taking blood thinners several days before your procedure to prevent bleeding.
- You may need an ultrasound to help your healthcare provider plan your procedure. An ultrasound may be done to show the shape and location of your varicose veins. You will need to plan for someone to drive you home from your procedure.
What will happen during endovenous ablation:
- You may be given local anesthesia to numb the surgery area. With local anesthesia, you may still feel pressure or pushing during the procedure, but you should not feel any pain. You may also be given IV sedation to help you relax during the procedure.
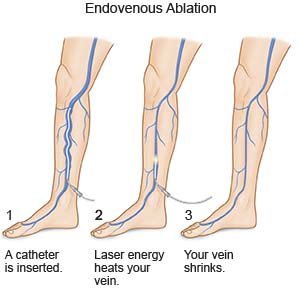
- Your healthcare provider may make a small cut in your skin. He or she will insert a small catheter through your skin and into your vein. Your healthcare provider will send laser or radiofrequency energy through the catheter and heat your vein. The heat will close your vein to stop blood flow. Your varicose veins will shrink and stop bulging under your skin. Your healthcare provider will remove the catheter. He or she will place a small bandage over your incision.
 |
What to expect after endovenous ablation:
- You may spend a night in the hospital so the circulation in your leg can be monitored. You may need to wear compression stockings. The stockings are tight and put pressure on your legs. This improves blood flow and helps prevent clots. You may need an ultrasound within 72 hours to look at your veins and check for blood clots. Your healthcare provider may tell you to start your normal activities immediately after endovenous ablation. He or she may also tell you to avoid air travel or sitting for long periods of time.
- You may have mild to moderate pain. You may have mild to severe bruising. Your healthcare provider will tell you how to treat pain and bruising.
Risks of endovenous ablation:
You may bleed more than usual or develop an infection. You may develop a pocket of blood under your skin that may need to be removed. You may get a blood clot in your leg. This may become life-threatening. Nerves and blood vessels may become damaged during your procedure. Your vein may become swollen, red, and painful. Your skin may be burned.
Call your local emergency number (911 in the US) for any of the following:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
- You have trouble breathing.
Related medications
Seek care immediately if:
- Blood soaks through your bandage.
- Your leg feels warm, tender and painful.
- Any part of your leg is numb or pale to the touch.
Call your doctor if:
- You have a fever or chills.
- Your wound is red, swollen, or draining pus.
- You have nausea or vomiting.
- Your skin is itchy, swollen, or you have a rash.
- You have questions or concerns about your condition or care.
Care for yourself at home:
- Stay active. Do not spend too much time sitting or standing. If you need to stand, shift your weight from leg to leg often. Take short walks throughout the day. Walking will improve blood flow and prevent blood clots in your leg. Ask your healthcare provider how much activity you need to do every day.
- Do not cross your legs when you sit. This decreases blood flow to your feet and can make your symptoms worse.
- Wear compression stockings or bandages as directed. The stockings and bandages are snug and put pressure on your legs. This improves blood flow and helps prevent clots.

- Apply a warm compress as directed. A warm compress can be a small towel or washcloth. Moisten it in warm (not hot) water. Apply the warm compress to your leg. A warm compress may help with discomfort from injury to your vein during the procedure.
- Elevate your leg. Keep your leg above the level of your heart as often as possible. This will help decrease swelling and pain. Prop your leg on pillows or blankets to keep it elevated comfortably.

- Do not wear tight clothing or shoes. Do not wear high-heeled shoes. Do not wear clothes that are tight around the waist or knees.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for the procedure area:
Carefully wash the area with soap and water. Dry the area and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. Check for signs of infection such as redness, swelling, or pus.
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
