Embolectomy
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
AMBULATORY CARE:
What you need to know about an embolectomy:
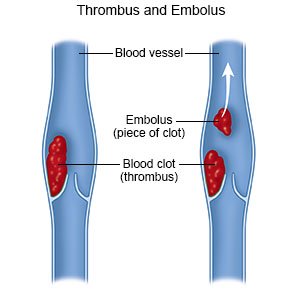
An embolectomy is surgery to remove an embolus from an artery or vein. An embolus is part of a blood clot that broke free. It can travel through your bloodstream and become stuck in another area. This is called an embolism. An embolism can block blood flow to the area. An embolus in your vein can reach your lungs. This is called a pulmonary embolism, or PE. An embolus in your artery can reach your brain. This can cause a stroke. An embolus in a femoral artery in your leg can cause tissue death in the leg. An embolus in an artery in your abdomen can cause pain and vomiting. An embolectomy is used when medicines or procedures cannot be used, or are not successful.
 |
How to prepare for an embolectomy:
An embolectomy may need to be done as immediate emergency surgery. The following is general information if you are able to plan for surgery.
- Your surgeon will tell you how to prepare. Your surgeon may tell you not to eat or drink anything after midnight on the day of surgery. Arrange to have someone drive you home after you are discharged.
- Tell your surgeon about any allergies you have, including to anesthesia, contrast liquid, or medicines. Contrast liquid may be used during surgery to help your surgeon see the blood vessel and embolus better.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for surgery, and when to stop. Your surgeon will tell you which medicines to take or not to take on the day of surgery.
What will happen during an embolectomy:
- You may be given local anesthesia to numb the area so you do not feel pain. You may instead be given general anesthesia to keep you asleep and free from pain.
- The following are ways the embolus may be removed:
- A catheter embolectomy is a minimally invasive surgery. A catheter (thin tube) is guided into the vein or artery that has the embolus. Suction is used to remove the embolus through the catheter.
- A balloon embolectomy is also minimally invasive. A catheter with a balloon on the end is guided into the vein, past the clot. The balloon is inflated (filled) and pulled back out of the vein. The embolus comes back through the vein with the catheter. The balloon helps move the embolus and keep it from continuing into the vein.
- An open embolectomy is usually only done for a large embolus, most often to treat a PE. Your surgeon will make an incision in the skin over the embolus. Your surgeon will open the vein or artery and remove the embolus.
- A filter may be placed to prevent another embolus from being able to travel through your body. Your surgeon will check that all of the embolus was removed. Your surgeon may place a filter in the blood vessel. The filter helps prevent pieces of the embolus from continuing to travel. When blood flows freely, your surgeon will close the vein or artery. The incision area will be covered with a pressure bandage.
What to expect after an embolectomy:
- You may have swelling or pain in the surgery area. You may be given medicines to reduce pain or swelling. You may need to stay in the hospital for up to 1 week, depending on where you had the embolectomy. You may need to lie still for several hours right after your surgery.
- Healthcare providers will help you walk around the same day of your surgery, or the day after. Movement will help prevent blood clots. You may also be given exercises to do in bed. Do not get out of bed on your own until your healthcare provider says you can. Ask before you get up the first time. You may need help to stand up safely.
- Healthcare providers will change the bandage over the embolectomy site as needed.
Risks of an embolectomy:
You may bleed more than expected or develop an infection. The blood vessel or tissues near the area may be damaged. Your surgeon may not be able to remove the embolus. Pieces of the embolus may break free and continue through the blood vessel.
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
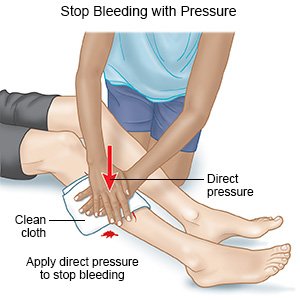
- The surgery area does not stop bleeding even after you apply firm pressure for 10 minutes.
- The leg or arm used for your surgery is numb, painful, or changes color.
- The bruise at your catheter site gets bigger or becomes swollen.
- You have purple spots or blisters on your skin.
Call your surgeon or hematologist if:
- You have a fever.
- You have a new skin rash and itching.
- You feel weak, lightheaded, or faint.
- You have new swelling around your eyes.
- You see blood in your urine.
- You have pain at the surgery site that does not get better with pain medicine.
- You have questions or concerns about your condition or care.
Medicines:
- Antiplatelets , such as aspirin, help prevent blood clots. Take your antiplatelet medicine exactly as directed. These medicines make it more likely for you to bleed or bruise. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Related medications
Care for the surgery area as directed:
- Keep the area clean and dry. Your healthcare provider will tell you when you can bathe. You will need to keep the bandage in place and dry for a day or two after your surgery. Cover the bandage with a plastic bag and tape the opening around your skin to keep water out.
- Carefully wash around the area with soap and water when it is okay to bathe. Let soap and water run gently over the area.
- Dry the area and put on new, clean bandages as directed. Check the area every day for signs of infection, such as redness, swelling, or pus. Change your bandage if it gets wet or dirty.
Wear a compression device as directed:
Examples include pressure stockings, intermittent pneumatic compression, and sequential compression devices. A compression device puts pressure on your lower legs to help keep blood from pooling in your leg veins. Your healthcare provider can prescribe the right device for you. Do not buy over-the-counter devices unless your provider says it is okay. They may not fit correctly or may have elastic that cuts off your circulation. Ask your provider when to start wearing a compression device and how long to wear it.
 |
Keep your leg elevated as directed:
Keep your leg above the level of your heart when you are sitting. Prop your leg on pillows to keep it elevated comfortably. Ask how long to keep your leg elevated each day. You will need to balance elevation with movement to prevent blood clots.
 |
Watch for bleeding and bruising:
It is normal to have a bruise and soreness where you had an embolectomy. Contact your healthcare provider if your bruise gets larger. If the area bleeds, use your hand to put pressure on the bandage. If you do not have a bandage, use a clean cloth to put pressure over and just above the area. Seek care immediately if the bleeding does not stop within 10 minutes.
 |
Follow your healthcare provider's directions for daily activities:
Your provider will give you instructions based on the type of embolectomy you had. The following are general safely guidelines to follow:
- Your provider will tell you when it is safe to drive, be active, and do normal daily activities. An active lifestyle can help prevent blood clots. Try to get at least 30 minutes of activity on most days of the week. If you sit most of the day for work, stand or walk around every half hour. After a future injury or illness, try to become active again as soon as possible. Activity can also help you manage your weight. Extra body weight can put pressure on your leg veins and cause blood to pool. This increases your risk for another blood clot.
- Do not lift anything heavier than 10 pounds for 2 days after your surgery. For example, a gallon of milk weighs 8 pounds.
- Do not strain when you have a bowel movement. This may cause bleeding from the area where you had the embolectomy. Ask your provider if you need medicine to help make your bowel movements easier.
Drink more liquids:
Liquid can help prevent blood clots. Ask your healthcare provider how much liquid to drink each day and which liquids are best for you.
Do not smoke:
Nicotine and other chemicals in cigarettes and cigars can cause blood vessel and lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Limit alcohol as directed:
Limit alcohol to 1 drink a day if you are female. Limit alcohol to 2 drinks a day if you are male. A drink is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
Follow up with your surgeon or hematologist as directed:
You may need to be checked for blood clots for up to 3 years after treatment. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
