Bladder Fulguration
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
Bladder fulguration
is a procedure to destroy abnormal growths or tissue. The procedure may be used to treat problems such as cystitis or some forms of cancer. Your healthcare provider will use a laser or electrocautery device to create energy. The energy makes heat that destroys tissue.
 |
How to prepare for the procedure:
- Your healthcare provider will tell you how to prepare. He or she may tell you not to eat or drink anything the night before the procedure. Arrange to have someone drive you home from the procedure.
- Tell your provider about all medicines you currently take. He or she will tell you if you need to stop any medicine for the procedure, and when to stop. He or she will tell you which medicines to take or not take on the day of your procedure.
- You may need to have an ultrasound or urine tests. Your provider will tell you when to have these tests before your procedure.
What will happen during the procedure:
- You may be given general anesthesia to keep you asleep and pain free during your procedure. Your healthcare provider may instead put local anesthesia into your urethra and bladder. With local anesthesia, you will not feel pain, but you may be able to feel some pressure during your procedure. You may also feel burning or a need to urinate during the procedure.
- A cystoscope will be placed through your urethra and into your bladder. A cystoscope is a small tube with a light and magnifying camera on the end. Your healthcare provider will look at the walls of your urethra as the scope goes through to your bladder. Your bladder will be filled with liquid so your provider can see the inside of your bladder more clearly.
- Tools may be inserted through the cystoscope to treat any problems in your urethra or bladder. Your provider may also take a sample of tissue and send it to a lab for tests. A laser or other device will be used to destroy tissue. New, healthy tissue may grow back in the same place.
What to expect after the procedure:
- You will be taken to a recovery room until you are fully awake. Do not get out of bed until healthcare providers say it is okay. When providers see that you are okay, you will be taken back to your hospital room.
- You will be helped to walk around after the procedure. Movement helps prevent blood clots.
- Your healthcare provider will check to make sure you can urinate on your own. You may see small amounts of blood in your urine. This is normal. It is also normal to have an increased need to urinate. You may also have burning or mild discomfort in your bladder or kidney area when you urinate.
- Medicines may be given to prevent or treat pain or nausea. Blood thinning medicine may be given to help prevent blood clots.
Risks of bladder fulguration:
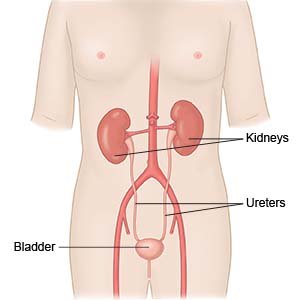
You may bleed more than expected or develop an infection. Your urethra, bladder, or ureters may get damaged during your procedure. Swelling caused by the cystoscopy may cause a blockage or slow urine flow. These problems may make it hard to control your urine.
Related medications
Seek care immediately if:
- You have severe pain in your bladder or abdomen.
- Your abdomen becomes tender and hard.
- Your urine turns from pink to red, or you have clots in your urine.
- You cannot urinate and your bladder feels full.
Call your doctor or urologist if:
- You have problems urinating.
- You urinate less than usual, or still feel like you have to urinate after you use the bathroom.
- You have a fever.
- Your pain or burning during urination becomes worse or lasts longer than 1 day.
- Your urine stays pink for longer than 1 day.
- You have nausea or are vomiting.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antibiotics help prevent or treat a bacterial infection.
- Medicine will be given to prevent a burning feeling when you urinate. The medicine will make your urine turn orange or blue. This is normal.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care:
- Get more rest. Rest when you need to while you heal. Slowly start to do more each day. Return to your daily activities as directed. Your healthcare provider will tell you when it is okay to drive.
- Drink more liquids. Ask your healthcare provider how much liquid you should drink each day, and which liquids are best for you.
- Apply a warm, damp washcloth over your urethral opening. This may help to relieve discomfort.
- Do not have sex until your healthcare provider tells you it is okay. Sex may increase your risk for a urinary tract infection.
Follow up with your doctor or urologist as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
