Before CABG (Coronary Artery Bypass Graft)
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
AMBULATORY CARE:
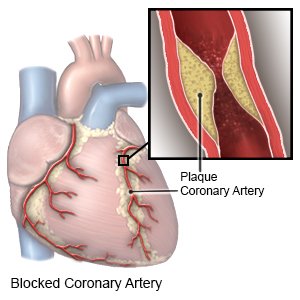
Coronary artery bypass graft (CABG)
is open heart surgery to clear blocked arteries in your heart. CABG surgery improves blood flow to your heart by bypassing (sending blood around) the blocked part of an artery. This restores blood flow to your heart and helps prevent a heart attack.
 |
Call your doctor or cardiologist if:
- You have a fever or symptoms of the flu the day before, or the day of, your surgery.
- You have questions or concerns about your condition or care.
Tests
may be needed several days before or on the day of surgery. You may need blood tests, an electrocardiogram (EKG), or an echocardiogram. You may also need a cardiac catheterization or a coronary angiogram. These tests will help your healthcare provider see where the blood flow is blocked and help him plan your surgery.
Eating and drinking before surgery:
Your healthcare provider may tell you not to eat or drink anything after midnight on the day of your surgery.
Medicines before surgery:
Your healthcare provider will tell you which medicines to take or not take on the day of your surgery. Talk to your healthcare provider several days before your surgery about any medicines that you take regularly:
- You may need to stop taking blood thinner, aspirin, or NSAID medicine several days before surgery. This may prevent bleeding during and after your surgery.
- You may need to stop taking certain vitamins or herbal supplements several days before surgery. Some vitamins and herbal supplements increase the risk for bleeding and other complications.
- If you have diabetes, ask about your insulin. On the morning of your surgery, you may need to skip your dose or take a smaller dose. This will prevent your blood sugar level from going too low. Do not take your oral diabetic medicine on the morning of your surgery.
- Ask your healthcare provider if you should take your blood pressure or heart medicine before your surgery. Do not stop your medicine without talking to your healthcare provider.
- Take any medicine you were told to take with a sip of water on the morning of your surgery.
Related medications
Crestor
Crestor (rosuvastatin) is used to treat high cholesterol and high triglycerides in the blood ...
Ranexa
Ranexa (ranolazine) is used to chronic treat angina (chest pain). Learn about side effects ...
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
Metoprolol
Metoprolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Ibuprofen
Ibuprofen (Advil, Motrin) treats minor aches and pains caused by the common cold, headaches ...
Gabapentin
Gabapentin is an anti-epileptic drug, also called an anticonvulsant. It is used to treat some types ...
Nitroglycerin
Nitroglycerin is used for anal fissure and fistula, angina, angina pectoris prophylaxis, heart ...
Tramadol
Tramadol is an opioid medication that may be used to treat moderate to moderately severe chronic ...
Tylenol
Tylenol is a pain reliever and a fever reducer used to treat many conditions such as headaches ...
Acetaminophen
Acetaminophen is a widely used pain reliever and fever reducer for conditions like headaches ...
Blood donation before surgery:
You may be able to donate your own blood before surgery. This is called autologous blood donation. You may also ask a family member or friend with the same blood type to donate blood for you. This is called directed blood donation.
Weight loss before surgery:
You may need to lose weight before your surgery. This helps decrease the stress on your heart and your risk for complications during or after surgery. Talk to your healthcare provider if you need help to lose weight.
Quit smoking before surgery:
Nicotine and other chemicals in cigarettes and cigars can damage your heart and lungs. Smoking may prevent healing and increase your risk for complications during or after your surgery. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
What to expect after surgery:
- You may spend 1 to 3 days in an intensive care unit (ICU). Healthcare providers will closely monitor your breathing, blood pressure, oxygen levels, and heart rate. They will also watch for any complications. You may need several medicines to control your blood pressure and heart rate, and to prevent blood clots. You may also need a blood transfusion. After you leave the ICU, you may need to spend 3 to 5 days in the hospital before you can go home.
- You may wake up from surgery with an endotracheal tube (ET tube). An ET tube is inserted through your mouth and into your lungs. It is attached to a ventilator. A ventilator is a machine that gives you oxygen and breathes for you when you cannot breathe well on your own. Healthcare providers will remove the ET tube when you are awake, you can breathe on your own, and your heart is working correctly.
- When your ET tube is removed, it is important to cough, and deep breathe. This will decrease your risk for a lung infection. It is also important to walk around as soon as healthcare providers tell you it is okay. This will help prevent blood clots.
- You may have several drains, IVs, and a pacemaker. You may have a drain in your bladder to empty your urine. A drain may be placed in your chest to prevent blood from collecting around your heart. You may have several IVs in your arm, neck, or chest. You may also have a temporary pacemaker to control your heartbeat.
- You may have pain in your chest after surgery. Healthcare providers will give you pain medicine. They will also show you how to use a splint when you need to cough and turn in bed. A splint is a pillow or soft object that you can press lightly against your chest. This will decrease pain when you move or cough.
- You may not be able to eat right away. You will be given ice chips and then clear liquids. If you do okay with those, you will be able to eat solid foods.
Cardiac rehabilitation (rehab):
You may need to go to cardiac rehab after surgery. Cardiac rehab is a program run by specialists who help you safely strengthen your heart and prevent more heart disease. The plan includes exercise, relaxation, stress management, and heart-healthy nutrition. Healthcare providers will also check to make sure any medicines you take are working. The plan may also include instructions for when you can drive, return to work, and do other normal daily activities.
Follow up with your doctor or cardiologist as directed:
You may need to go in regularly for tests to check how your heart is doing. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
