After Thrombolysis
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
AMBULATORY CARE:
After thrombosis,
it is important to go to follow-up appointments and to take blood thinners as directed. This will help prevent another deep vein thrombosis.
Call your local emergency number (911 in the US) or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- The procedure area does not stop bleeding even after you apply firm pressure for 10 minutes.
- The leg or arm used for your procedure is numb, painful, or changes color.
- The bruise at your catheter site gets bigger or becomes swollen.
- You have purple spots or blisters on your skin.
Call your doctor or hematologist if:
- You have a fever.
- You have a new skin rash and itching.
- You feel weak, lightheaded, or faint.
- You have new swelling around your eyes.
- You see blood in your urine.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antiplatelets , such as aspirin, help prevent blood clots. Take your antiplatelet medicine exactly as directed. These medicines make it more likely for you to bleed or bruise. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
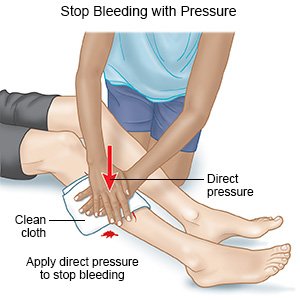
Watch for bleeding and bruising:
It is normal to have a bruise and soreness where the catheter went in. Tell your healthcare provider if your bruise gets larger. If your procedure area bleeds, use your hand to put pressure on the bandage. If you do not have a bandage, use a clean cloth to put pressure over and just above the catheter site. Seek care immediately if the bleeding does not stop within 10 minutes.
 |
Related medications
Wear a compression device as directed:
Examples include pressure stockings, intermittent pneumatic compression, and sequential compression devices. A compression device puts pressure on your lower legs to help keep blood from pooling in your leg veins. Your healthcare provider can prescribe the right device for you. Do not buy over-the-counter devices unless your provider says it is okay. They may not fit correctly or may have elastic that cuts off your circulation. Ask your provider when to start wearing a compression device and how long to wear it.
 |
Keep your leg elevated as directed:
Keep your leg above the level of your heart when you are sitting. Prop your leg on pillows to keep it elevated comfortably. Ask how long to keep your leg elevated each day. You will need to balance elevation with movement to prevent blood clots.
 |
Care for the procedure area as directed:
- Keep the area clean and dry. Ask your healthcare provider when you can bathe. You will need to keep the bandage in place and dry for a day or two after your procedure. Cover the bandage with a plastic bag and tape the opening around your skin to keep water out.
- Your provider will tell you when it is okay to bathe without a bandage. Carefully wash around the area with soap and water. Let soap and water run gently over the area.
- Check the area every day for signs of infection, such as redness, swelling, or pus. Dry the area and put on new, clean bandages as directed. Change your bandage if it gets wet or dirty.
Drink liquids as directed:
Liquid can help prevent blood clots. Ask your healthcare provider how much liquid to drink each day and which liquids are best for you. Do not drink alcohol for 24 hours after your procedure.
Do not smoke:
Nicotine and other chemicals in cigarettes and cigars can cause blood vessel and lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Activity:
- Do not lift anything heavier than 10 pounds for 2 days after your procedure. For example, a gallon of milk weighs 8 pounds.
- Do not strain when you have a bowel movement. Straining may cause bleeding from your procedure area. Ask your healthcare provider if you need medicine to help make your bowel movements easier.
- Your provider will tell you when it is safe to drive and do normal daily activities. An active lifestyle can help prevent blood clots. Try to get at least 30 minutes of activity on most days of the week. If you sit most of the day for work, stand or walk around every half hour. After a future injury or illness, try to become active again as soon as possible.
- Reach or maintain a healthy weight. Too much body weight can put pressure on your leg veins and cause blood to pool. This increases your risk for another blood clot. Activity can help you manage your weight. Ask your provider what a healthy weight is for you. Your provider can help you create a safe weight loss plan, if needed.
- Manage health conditions that can cause a blood clot. Examples are high cholesterol and diabetes.
Follow up with your doctor or hematologist as directed:
You may need to be checked for blood clots for up to 3 years after treatment. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about After Thrombolysis
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
