Peripheral Thrombolysis
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about peripheral thrombolysis?
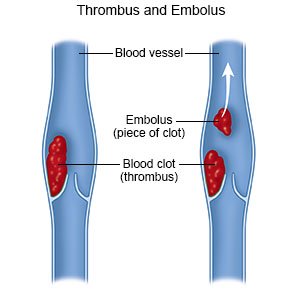
Peripheral thrombolysis is a procedure to break up or dissolve a blood clot in your arm or leg. The clot may be removed with a device during the procedure. You may need thrombolysis to remove a clot quickly so it does not break free. You may need the procedure to remove a blood clot from deep veins, called deep vein thrombosis (DVT). A DVT usually happens in a leg, but it can also happen in an arm. A DVT can also break free. A clot that breaks off in your arm or leg may travel to your lungs. This can be life-threatening.
 |
How do I prepare for the procedure?
- Your healthcare provider will tell you how to prepare. Your provider may tell you not to eat or drink anything after midnight on the day of your procedure. Arrange to have someone drive you home when you are discharged.
- Tell your provider about all your current medicines. Your provider will tell you if you need to stop any medicine for the procedure, and when to stop. Your provider will tell you which medicines to take or not take on the day of your procedure.
- Tell your provider about any allergies you have, including to anesthesia, contrast liquid, or medicines. You may be given contrast liquid before or during the procedure to help your healthcare provider see the clot better. You may be given antibiotics to prevent an infection caused by bacteria.
Related medications
What will happen during the procedure?
- You will be given local anesthesia to numb the procedure area. With local anesthesia, you may still feel pressure or pushing, but you should not feel any pain.
- Your healthcare provider will inject medicine into your IV that will help dissolve or break up the clot. It is most often given into a vein, but it may be given into an artery. A catheter is guided by x-ray so it is near the blood clot.
What should I expect after the procedure?
Healthcare providers will apply pressure on the procedure area to stop any bleeding. You will be monitored closely for any problems. Do not get out of bed until your healthcare provider says it is okay. You will then be able to go home or be taken to your hospital room.
- The catheter may be left in place if the medicine needs to continue to break up the clot. You will need to stay in the hospital if the catheter is left in place. Your healthcare provider will need to do the thrombolysis again to remove the rest of the clot. You will be told not to move the leg or arm used for the procedure while the catheter is in place. You will need to lie still. Tell your healthcare provider if lying flat starts to cause back discomfort. If there is no bleeding, your provider may help you roll onto your side. A Foley catheter may be placed in your bladder. This catheter allows urine to drain from your bladder into a collection bag.
- You may need to wear a pressure device or inflatable boots if your procedure was for a leg clot. These are tight and put pressure on your legs to improve blood flow and prevent clots. The boots have an air pump that tightens and loosens different areas of the boots. You may need to continue wearing a pressure device after you leave the hospital. Your provider will tell you when to start wearing the device and how long to wear it each day.

- You will be helped to walk around the same day of your procedure, or the day after. Movement will help prevent blood clots. You may also be given exercises to do in bed. Do not get out of bed on your own until your healthcare provider says you can. Ask before you get up the first time. You may need help to stand up safely. When you are able to get up on your own, sit or lie down right away if you feel weak or dizzy. Then press the call button to let someone know you need help.
- Medicines:
- Anticoagulants are a type of blood thinner medicine that helps prevent clots. Anticoagulants may cause you to bleed or bruise more easily.
- Antiplatelets help prevent blood clots. This medicine makes it more likely for you to bleed or bruise.
What are the risks of peripheral thrombolysis?
Thrombolysis increases your risk for bleeding. You may have increased nosebleeds or bleeding from your gums. You may also have bleeding in your stomach or brain. Bleeding can become severe and life-threatening. You may have an allergic reaction to the contrast liquid or to the medicine used to break up the clot.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Peripheral Thrombolysis
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
