Hydralazine Side Effects
Medically reviewed by Drugs.com. Last updated on Jun 27, 2024.
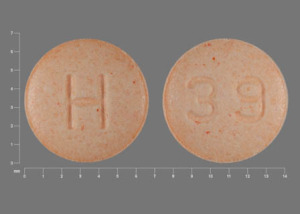
Applies to hydralazine: oral tablet.
Other dosage forms:
Precautions
It is important that your doctor check your progress at regular visits to make sure that this medicine is working properly. Blood tests may be needed to check for unwanted effects.
Hydralazine may cause some people to have headaches or to feel dizzy. Make sure you know how you react to this medicine before you drive, use machines, or do anything else that could be dangerous if you are dizzy or not alert.
Do not take other medicines unless they have been discussed with your doctor. This especially includes over-the-counter (nonprescription) medicines for appetite control, asthma, colds, cough, hay fever, or sinus problems, since they may tend to increase your blood pressure.
Serious side effects of hydralazine
Along with its needed effects, hydralazine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking hydralazine:
More common side effects
- arm, back, or jaw pain
- chest pain or discomfort
- chest tightness or heaviness
- fast, pounding, or irregular heartbeat or pulse
- nausea
- shortness of breath
- sweating
Less common side effects
- black, tarry stools
- blindness or vision changes
- blisters on the skin
- blurred vision
- burning of the face or mouth
- burning, crawling, itching, numbness, painful, prickling, "pins and needles", or tingling feelings
- chills
- clumsiness or unsteadiness
- confusion
- cough
- difficult or labored breathing
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- fever and sore throat
- general feeling of discomfort or illness or weakness
- joint pain
- lower back or side pain
- muscle pain
- numbness, tingling, pain, or weakness in the hands or feet
- painful or difficult urination
- pale skin
- shakiness in the legs, arms, hands, or feet
- skin rash or itching
- swelling of the feet or lower legs
- swollen, painful, or tender lymph glands in the neck, armpit, or groin
- tightness in the chest
- trembling or shaking of the hands or feet
- ulcers, sores, or white spots in the mouth
- unusual bleeding or bruising
- unusual tiredness or weakness
- weakness in hands or feet
Rare side effects
- dark urine
- light-colored stools
- upper right abdominal or stomach pain
- yellow eyes and skin
Get emergency help immediately if any of the following symptoms of overdose occur while taking hydralazine:
Symptoms of overdose
- feeling of warmth
- headache
- redness of the face, neck, arms, and occasionally, upper chest
Other side effects of hydralazine
Some side effects of hydralazine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- diarrhea
- loss of appetite
- weight loss
Less common side effects
- constipation
- difficulty with moving
- dizziness
- feeling anxious or depressed
- muscle cramps, pain, or stiffness
- pain in the joints
- rash, hives, welts, or itching
- stuffy nose
- watery eyes
See also:
Lasix
Lasix is a loop diuretic used to treat fluid retention from heart, liver, or kidney conditions, and ...
Enalapril
Enalapril is used to treat high blood pressure, congestive heart failure and to improve survival ...
Botox
Botox is used for cosmetic purposes and to treat overactive bladder symptoms, urinary incontinence ...
Valsartan
Valsartan is an angiotensin II receptor blocker (ARB) that may be used to treat high blood pressure ...
Hydrochlorothiazide
HCTZ (hydrochlorothiazide) used to treat high blood pressure (hypertension) and edema. Includes ...
Atenolol
Atenolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Furosemide
Furosemide is a loop diuretic used to treat fluid retention and high blood pressure by increasing ...
Metoprolol
Metoprolol is used to treat angina (chest pain) and hypertension (high blood pressure). Learn about ...
Losartan
Losartan is used to treat high blood pressure (hypertension). It is also used to lower the risk of ...
Lisinopril
Lisinopril is an ACE inhibitor. It is used to treat high blood pressure, congestive heart failure ...
For healthcare professionals
Applies to hydralazine: compounding powder, injectable solution, oral tablet.
General adverse events
The most frequently reported side effects were palpitations and tachycardia.[Ref]
Cardiovascular
- Very common (10% or more): Palpitations, tachycardia
- Common (1% to 10%): Angina pectoris, flushing, hypotension
- Uncommon (0.1% to 1%): Heart failure, vasculitis
- Very rare (less than 0.01%): Paradoxical pressor response[Ref]
Gastrointestinal
- Common (1% to 10%): Nausea, vomiting, diarrhea, gastrointestinal disturbances
- Very rare (less than 0.01%): Paralytic ileus
- Frequency not reported: Constipation[Ref]
Nervous system
- Common (1% to 10%): Headache
- Uncommon (0.1% to 1%): Dizziness
- Very rare (less than 0.01%): Peripheral neuritis, paresthesia, tremor, polyneuritis
- Frequency not reported: Tingling, numbness[Ref]
Musculoskeletal
- Common (1% to 10%): Arthralgia, joint swelling, myalgia
- Uncommon (0.1% to 1%): Systemic lupus erythematosus-like syndrome
- Frequency not reported: Muscle cramp[Ref]
Metabolic
- Common (1% to 10%): Anorexia[Ref]
Immunologic
- Common (1% to 10%): Positive antinuclear factor[Ref]
Respiratory
- Uncommon (0.1% to 1%): Nasal congestion, dyspnea, pleural pain[Ref]
Hematologic
- Uncommon (0.1% to 1%): Anemia, leukopenia, neutropenia, thrombocytopenia
- Very rare (less than 0.01%): Hemolytic anemia, leukocytosis, lymphadenopathy, pancytopenia, splenomegaly, agranulocytosis, eosinophilia
- Frequency not reported: Blood dyscrasias, hemoglobin decreased, red cell count decreased[Ref]
Renal
- Uncommon (0.1% to 1%): Serum creatinine increased, glomerulonephritis
- Very rare (less than 0.01%): Acute renal failure[Ref]
Dermatologic
- Uncommon (0.1% to 1%): Rash, purpura, urticaria, pruritus[Ref]
Hepatic
- Uncommon (0.1% to 1%): Jaundice, liver enlarged, abnormal liver function, hepatitis[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Hypersensitivity reaction[Ref]
Genitourinary
- Uncommon (0.1% to 1%): Proteinuria, hematuria, urinary retention
- Very rare (less than 0.01%): Retroperitoneal fibrosis
- Frequency not reported: Urination difficult[Ref]
Ocular
- Uncommon (0.1% to 1%): Lacrimation increased, conjunctivitis
- Very rare (less than 0.01%): Exophthalmos[Ref]
Other
- Uncommon (0.1% to 1%): Edema, fever, weight decreased, malaise
- Frequency not reported: Chills[Ref]
Psychiatric
- Uncommon (0.1% to 1%): Agitation, anxiety
- Very rare (less than 0.01%): Depression, hallucinations
- Frequency not reported: Psychotic reactions, disorientation, anxiety[Ref]
References
1. (2001) "Product Information. Apresoline (hydralazine)." Ciba-Geigy Pharmaceuticals
2. Cerner Multum, Inc. "UK Summary of Product Characteristics."
3. Cerner Multum, Inc. "Australian Product Information."
4. (2016) "Product Information. HydrALAZINE Hydrochloride (hydralazine)." Akorn Inc
More about hydralazine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (92)
- Drug images
- Dosage information
- Patient tips
- During pregnancy
- Drug class: vasodilators
- Breastfeeding
- En español
Patient resources
- Hydralazine drug information
- Hydralazine (Injection) (Advanced Reading)
- Hydralazine Tablets
- Hydralazine Injection
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Hydralazine side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.