Tisagenlecleucel
Medically reviewed by Drugs.com. Last updated on Jul 21, 2025.
Pronunciation
(tis a jen lek LOO sel)
Index Terms
- Autologous CART-19 TCR:4-1BB cells
- CD19CAR-CD3zeta-4-1BB-Expressing Autologous T Lymphocytes
- CTL019
Dosage Forms
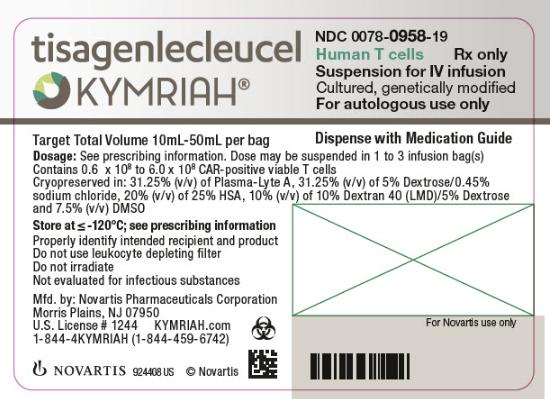
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Intravenous:
Kymriah: (1 ea) [contains albumin human, dextran 40, dimethyl sulfoxide]
Brand Names: U.S.
- Kymriah
Pharmacologic Category
- Antineoplastic Agent, Anti-CD19
- Antineoplastic Agent, CAR-T Immunotherapy
- CAR-T Cell Immunotherapy
- Cellular Immunotherapy, Autologous
- Chimeric Antigen Receptor T-Cell Immunotherapy
Pharmacology
Tisagenlecleucel is a CD19-directed genetically modified autologous T cell immunotherapy (containing human cells modified with a lentivirus) in which a patient's T cells are reprogrammed with a transgene encoding a chimeric antigen receptor (CAR) to identify and eliminate CD19-expressing malignant and normal cells. The CAR is comprised of a murine single-chain antibody fragment which recognizes CD19 and is fused to intracellular signaling domains from 4-1BB (CD137) and CD3 zeta. CD3 zeta is a critical component for initiating T-cell activation and antitumor activity, while 4-1BB enhances expansion and persistence of tisagenlecleucel. After binding to CD19-expressing cells, the CAR transmits a signal to promote T-cell expansion, activation, target cell elimination, and persistence of the tisagenlecleucel cells. Tisagenlecleucel is prepared from the patient's peripheral blood cells obtained via leukapheresis.
Distribution
High distribution into bone marrow.
Time to Peak
~10 days (in responding patients)
Half-Life Elimination
ALL: ~17 days (in responding patients); DLBCL: ~45 days (in responding patients)
Use: Labeled Indications
Acute lymphoblastic leukemia (relapsed or refractory): Treatment of B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse in patients up to 25 years of age.
Diffuse large B-cell lymphoma (relapsed or refractory): Treatment of relapsed or refractory large B-cell lymphoma in adults (after 2 or more lines of systemic therapy), including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high-grade B-cell lymphoma, and DLBCL arising from follicular lymphoma.
Limitation of use: Not indicated for treatment of primary CNS lymphoma.
Contraindications
There are no contraindications listed in the manufacturer's labeling.
Dosing: Adult
Note: For autologous use only; confirm patient identity on each bag prior to infusion. A single dose may be contained in up to 3 patient-specific infusion bags (acute lymphoblastic leukemia [ALL] doses are contained in a single infusion bag); verify the number of bags received for the dose with the certificate of conformance/analysis (cells from all bags must be infused to complete a single dose). The actual number of CAR-positive T cells in tisagenlecleucel are provided in the certificate of analysis. Delay tisagenlecleucel infusion for unresolved serious adverse reactions from chemotherapy (eg, pulmonary/cardiac reactions or hypotension), or active uncontrolled infection, active graft versus host disease (GVHD), or worsening leukemia burden following lymphodepleting chemotherapy.
Premedications: Premedicate with acetaminophen and diphenhydramine (or another H1-antihistamine) ~30 to 60 minutes prior to tisagenlecleucel infusion. Avoid prophylactic use of corticosteroids (may interfere with tisagenlecleucel activity).
Acute lymphoblastic leukemia (relapsed or refractory): Note: A treatment course consists of lymphodepleting chemotherapy (with fludarabine and cyclophosphamide) followed by tisagenlecleucel 2 to 14 days following completion of the fludarabine/cyclophosphamide regimen. Dosing is based on weight reported at the time of leukapheresis.
<25 years and ≤50 kg: IV: 0.2 to 5 x 106 CAR-positive viable T cells per kg body weight
<25 years and >50 kg: IV: 0.1 to 2.5 x 108 CAR-positive viable T cells
Diffuse large B-cell lymphoma (relapsed or refractory): IV: 0.6 to 6 x 108 CAR-positive viable T cells. A treatment course consists of lymphodepleting chemotherapy (with fludarabine and cyclophosphamide or with bendamustine for cyclophosphamide intolerance or resistance to a previous cyclophosphamide-containing regimen) followed by tisagenlecleucel 2 to 11 days following completion of the lymphodepleting regimen; lymphodepleting chemotherapy may be omitted if the WBC ≤1,000/mm3 within 1 week prior to tisagenlecleucel infusion.
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing: Pediatric
For autologous use only; confirm patient identity prior to prescribing.
Acute lymphoblastic leukemia (relapsed or refractory): Tisagenlecleucel is administered 2 to 14 days after completion of a lymphodepleting chemotherapy course of fludarabine and cyclophosphamide. Note: Delay tisagenlecleucel infusion for unresolved serious adverse reactions from chemotherapy (eg, pulmonary/cardiac reactions or hypotension), active uncontrolled infection, active graft versus host disease (GVHD), or increasing leukemia burden following lymphodepleting chemotherapy.
Premedicate with acetaminophen and diphenhydramine (or another H1-antihistamine) ~30 to 60 minutes prior to tisagenlecleucel infusion. Do not use corticosteroids at any time (except for life-threatening situations). Refer to the certificate of analysis for the actual number of CAR-positive T cells in tisagenlecleucel provided in patient-specific product.
Children and Adolescents weighing ≤50 kg: IV: 0.2 to 5 x 106 CAR-positive viable T cells per kg body weight.
Children and Adolescents weighing >50 kg: IV: 0.1 to 2.5 x 108 CAR-positive viable T cells.
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing adjustment for toxicity: Children and Adolescents:
Cytokine release syndrome (CRS):
Prodromal syndrome (low-grade fever, fatigue, anorexia): Observe in person, exclude infection, administer antibiotics (per local guidelines) if neutropenic, manage symptomatically.
CRS requiring mild intervention (one or more of the following: High fever, hypoxia, and/or mild hypotension): Administer antipyretics, oxygen, IV fluids, and/or low-dose vasopressors as needed.
CRS requiring moderate to aggressive intervention (one or more of the following: Hemodynamic instability despite IV fluids and vasopressor support, worsening respiratory distress [including pulmonary infiltrates and increasing oxygen requirement including high-flow oxygen and/or need for mechanical ventilation], rapid clinical deterioration): Administer high-dose or multiple vasopressors, oxygen, mechanical ventilation, and/or other supportive care as needed. Administer IV tocilizumab over 1 hour (weight-dependent dosing: If weight <30 kg: Tocilizumab 12 mg/kg; if weight ≥30 kg: Tocilizumab 8 mg/kg; maximum tocilizumab dose: 800 mg/dose; see tocilizumab monograph). If no clinical improvement, repeat tocilizumab as needed with at least an 8-hour interval between consecutive doses; if no response to the second tocilizumab dose consider a third tocilizumab dose or pursue alternative CRS management. Limit tocilizumab to a maximum of 4 doses. If no clinical improvement within 12 to 18 hours of the first tocilizumab dose or worsening at any time, administer methylprednisolone 2 mg/kg initially, then 2 mg/kg/day until vasopressors and high-flow oxygen are no longer needed, then taper corticosteroids.
Dosing: Adjustment for Toxicity
Cytokine release syndrome (CRS):
Prodromal syndrome (low-grade fever, fatigue, anorexia): Observe in person, exclude infection, administer antibiotics (per local guidelines) if neutropenic, manage symptomatically.
CRS requiring mild intervention (one or more of the following: High fever, hypoxia, and/or mild hypotension): Administer antipyretics, oxygen, IV fluids, and/or low-dose vasopressors as needed.
CRS requiring moderate to aggressive intervention (one or more of the following: Hemodynamic instability despite IV fluids and vasopressor support, worsening respiratory distress [including pulmonary infiltrates, increasing oxygen requirement including high-flow oxygen and/or need for mechanical ventilation], rapid clinical deterioration): Administer high-dose or multiple vasopressors, oxygen, mechanical ventilation and/or other supportive care as needed. Administer IV tocilizumab over 1 hour (patients ≥30 kg: tocilizumab 8 mg/kg; maximum tocilizumab dose: 800 mg; see tocilizumab monograph). If no clinical improvement, repeat tocilizumab as needed with at least an 8-hour interval between consecutive doses; if no response to the second tocilizumab dose consider a third tocilizumab dose or pursue alternative CRS management. Limit tocilizumab to a maximum of 4 doses. If no clinical improvement within 12 to 18 hours of the first tocilizumab dose or worsening at any time, administer methylprednisolone 2 mg/kg initially, then 2 mg/kg/day until vasopressors and high-flow oxygen are no longer needed, then taper corticosteroids.
Reconstitution
Inspect patient specific infusion bag(s) for breaks or cracks prior to thawing (if bag is compromised, contact manufacturer). Place infusion bag inside a second sterile bag in case of leaks and to protect ports from contamination. If more than 1 bag has been received for the treatment dose, thaw 1 bag at a time. Wait to thaw/infuse the next bag until it is determined that the previous bag is safely administered. Thaw at 37°C using a water bath or dry thaw method until there is no visible ice in the infusion bag, remove bag from thawing device immediately (once thawed and at room temperature, infuse within 30 minutes). Do not wash, spin down, and/or resuspend tisagenlecleucel in new media prior to infusion. Inspect the contents of the thawed infusion bag for visible cell clumps; if visible cell clumps remain, gently mix the contents of the bag (small clumps of cellular material should disperse with gentle manual mixing). Do not infuse if clumps are not dispersed, if the infusion bag is damaged or leaking, or if it otherwise appears to be compromised (contact manufacturer).
Administration
IV: For IV use only. Coordinate the timing of administration with thawing (once thawed and at room temperature, infuse within 30 minutes); infusion start time may need to be adjusted based on thawing.
Prime the tubing with NS prior to infusion. Infuse at a rate of 10 to 20 mL/minute, adjusting as appropriate for smaller volumes. Infuse entire contents of bag (infusion bag volume ranges from 10 to 50 mL), then (while maintaining a closed tubing system) rinse infusion bag with 10 to 30 mL NS to assure as many cells as possible are infused. Do not use a lymphocyte depleting filter. If more than 1 bag is being administered, thaw 1 bag at a time, wait to thaw/infuse the next bag until it is determined that the previous bag is safely administered. Cells from all bags must be infused to complete a single dose (doses for ALL will be contained in a single infusion bag).
Prior to administration: Ensure tocilizumab and emergency equipment are available prior to infusion and during recovery period. Premedicate with acetaminophen and diphenhydramine (or other histamine-1 antihistamine) ~30 to 60 minutes prior to tisagenlecleucel infusion. Avoid prophylactic use of corticosteroids (may interfere with tisagenlecleucel activity). Confirm patient identity and match to patient identifiers (preceded by the letters "DIN" or "Aph ID") on the infusion bag. Inspect the contents of the thawed infusion bag(s) for visible cell clumps; if visible cell clumps remain, gently mix the contents of the bag (small clumps of cellular material should disperse with gentle manual mixing). Do not infuse if clumps are not dispersed, if the infusion bag is damaged or leaking, or if it otherwise appears to be compromised. Apply universal precautions for product handling.
Storage
Store infusion bag(s) (frozen suspension) in the vapor phase of liquid nitrogen (≤-120°C), in a temperature-monitored system. After thawing, may only be stored for up to 30 minutes at room temperature of 20°C to 25°C.
Drug Interactions
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Corticosteroids (Systemic): May diminish the therapeutic effect of Tisagenlecleucel. Management: Avoid use of corticosteroids as premedication or at any time during treatment with tisagenlecleucel, except in the case of life-threatening emergency (such as resistant cytokine release syndrome). Consider therapy modification
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Management: Consider avoiding Echinacea in patients receiving therapeutic immunosuppressants. If coadministered, monitor for reduced efficacy of the immunosuppressant during concomitant use. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Granulocyte Colony-Stimulating Factors: May enhance the adverse/toxic effect of Tisagenlecleucel. Avoid combination
Inebilizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Leflunomide: Immunosuppressants may enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Consider therapy modification
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Management: Avoid use of immunosuppressants (including systemic corticosteroids) prior to initiation of nivolumab. Use of immunosuppressants after administration of nivolumab (eg, for immune-related toxicity) is unlikely to affect nivolumab efficacy. Consider therapy modification
Ocrelizumab: May enhance the immunosuppressive effect of Immunosuppressants. Monitor therapy
Ozanimod: Immunosuppressants may enhance the immunosuppressive effect of Ozanimod. Monitor therapy
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Management: Consider avoiding concomitant use of roflumilast and immunosuppressants as recommended by the Canadian product monograph. Inhaled or short-term corticosteroids are unlikely to be problematic. Consider therapy modification
Siponimod: Immunosuppressants may enhance the immunosuppressive effect of Siponimod. Monitor therapy
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Talimogene Laherparepvec: Immunosuppressants may enhance the adverse/toxic effect of Talimogene Laherparepvec. Specifically, the risk for disseminated herpetic infection may be increased. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
Upadacitinib: Immunosuppressants may enhance the immunosuppressive effect of Upadacitinib. Management: Concomitant use of upadacitinib with potent immunosuppressants is not recommended. Avoid combination
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated less than 2 weeks before starting or during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Immunosuppressants may enhance the adverse/toxic effect of Vaccines (Live). Immunosuppressants may diminish the therapeutic effect of Vaccines (Live). Management: Avoid use of live organism vaccines with immunosuppressants; live-attenuated vaccines should not be given for at least 3 months after immunosuppressants. Avoid combination
Vaccines (Live): Tisagenlecleucel may enhance the adverse/toxic effect of Vaccines (Live). Specifically, the risk of infection may be increased. Tisagenlecleucel may diminish the therapeutic effect of Vaccines (Live). Management: Avoid live virus vaccines for two weeks prior to initiation of lymphodepleting therapy, during tisagenlecleucel infusion, and after treatment until full immune recovery is achieved. Consider therapy modification
Test Interactions
May result in false positive results with some commercial HIV nucleic acid tests.
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
>10%:
Cardiovascular: Hypotension (26% to 31%), tachycardia (children, adolescents, and adults: 26%; adults: 13%), edema (21% to 23%), hypertension (children, adolescents, and adults: 19%; adults: 2%)
Central nervous system: Headache (children, adolescents, and adults: 37%; adults: 21%), encephalopathy (children, adolescents, and adults: 34%; adults: 16%), fatigue (25% to 26%), delirium (children, adolescents, and adults: 21%; adults: 6%), pain (15% to 18%), chills (10% to 13%), anxiety (9% to 13%), dizziness (6% to 11%)
Dermatologic: Skin rash (8% to 16%)
Endocrine & metabolic: Hypokalemia (children, adolescents, and adults; grades 3/4: 27%; adults, grades 3/4: 12%), hypophosphatemia (grades 3/4: 19% to 24%), hyponatremia (adults, grades 3/4: 11%), weight loss (adults: 11%)
Gastrointestinal: Decreased appetite (children, adolescents, and adults: 37%; adults: 12%), vomiting (children, adolescents, and adults: 26%; adults: 9%), diarrhea (26% to 31%), nausea (26% to 27), constipation (16% to 18%), abdominal pain (9% to 16%)
Hematologic & oncologic: Anemia (children, adolescents, and adults: 100%; adults, grades 3/4: 58%), neutropenia (children, adolescents, and adults: 100%; grades 3/4: 17% to 40%; adults, grades 3/4: 81%), thrombocytopenia (children, adolescents, and adults: 100%; grades 3/4: 12% to 27%; adults, grades 3/4: 54%), lymphocytopenia (adults, grades 3/4: 94%), leukopenia (adults, grades 3/4: 77%), hypogammaglobulinemia (children, adolescents, and adults: 43%; adults: 14%; grades ≥3: 4% to 7%), febrile neutropenia (children, adolescents, and adults: 37%; grades ≥3: 37%; adults: 17%; grades ≥3: 17%), hypofibrinogenemia (children, adolescents, and adults; grades 3/4: 16%; with cytokine release syndrome), increased INR (children, adolescents, and adults: 13%)
Hepatic: Increased serum aspartate aminotransferase (children, adolescents, and adults; grades 3/4: 28%), increased serum alanine aminotransferase (children, adolescents, and adults; grades 3/4: 21%), increased serum bilirubin (children, adolescents, and adults; grades 3/4: 21%)
Hypersensitivity: Cytokine release syndrome (74% to 79%)
Infection: Infection (41% to 55%; unknown pathogen), viral infection (children, adolescents, and adults: 26%; adults: 9%), bacterial infection (children, adolescents, and adults: 19%; adults: 9%), fungal infection (9% to 13%)
Neuromuscular & skeletal: Myalgia (7% to 15%), arthralgia (10% to 12%)
Renal: Acute renal failure (17% to 24%)
Respiratory: Hypoxia (children, adolescents, and adults: 24%; adults: 8%), cough (19% to 21%), dyspnea (16% to 18%), pulmonary edema (children, adolescents, and adults: 16%; adults: 3%), tachypnea (children, adolescents, and adults: 12%)
Miscellaneous: Fever (34% to 40%)
1% to 10%:
Cardiovascular: Cardiac failure (children, adolescents, and adults: 7%), thrombosis (3% to 7%), cardiac arrhythmia (adults: 6%), capillary leak syndrome (1% to 3%), cerebral infarction (adults: 1%)
Central nervous system: Sleep disorder (9% to 10%), peripheral neuropathy (4% to 8%), motor dysfunction (adults: 6%; children, adolescents, and adults: 1%), seizure (3%), speech disturbance (3%), ataxia (adults: 2%)
Dermatologic: Dermatitis (adults: 4%)
Endocrine & metabolic: Fluid retention (children, adolescents, and adults: 10%; adults: 3%)
Gastrointestinal: Abdominal distress (abdominal compartment syndrome; children, adolescents, and adults: 1%), fecal incontinence (adults: 1%)
Hematologic & oncologic: Disseminated intravascular coagulation (children, adolescents, and adults: 9%; adults: 3%), lymphocytosis (histiocytosis lymphoticytic hemophagocytosis; children, adolescents, and adults: 7%; adults: 1%), disorder of hemostatic components of blood (children, adolescents, and adults: 6%), prolonged partial thromboplastin time (children, adolescents, and adults: 6%), tumor lysis syndrome (children, adolescents, and adults: 6%; adults: 1%), pancytopenia (adults: 2%),
Immunologic: Antibody development (adults: 5%), graft versus host disease (children, adolescents, and adults: 1%)
Neuromuscular & skeletal: Back pain (6% to 10%), tremor (7% to 9%), asthenia (adults: 7%)
Ophthalmic: Visual impairment (3% to 7%)
Respiratory: Nasal congestion (children, adolescents, and adults: 10%), pleural effusion (5% to 10%), oropharyngeal pain (6% to 8%), respiratory distress (children, adolescents, and adults: 6%), respiratory failure (children, adolescents, and adults: 6%), acute respiratory distress (children, adolescents, and adults: 4%)
Miscellaneous: Multi-organ failure (3%)
Frequency not defined: Central nervous system: Aphasia, mutism
Related/similar drugs
ALERT: U.S. Boxed Warning
Cytokine release syndrome:Cytokine release syndrome (CRS), including fatal or life-threatening reactions, occurred in patients receiving tisagenlecleucel. Do not administer tisagenlecleucel to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids.
Neurological toxicities:Neurological toxicities, which may be severe or life-threatening, can occur following treatment with tisagenlecleucel, including concurrently with CRS. Monitor for neurological events after treatment with tisagenlecleucel. Provide supportive care as needed.
REMS program:Tisagenlecleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the KYMRIAH REMS.
Warnings/Precautions
Concerns related to adverse effects:
• Cytokine release syndrome: [US Boxed Warning]: Cytokine release syndrome (CRS), including fatal or life-threatening reactions, occurred in patients receiving tisagenlecleucel. Do not administer tisagenlecleucel to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or with tocilizumab and corticosteroids. Grade 3 and higher CRS reactions have occurred. The median time to onset of CRS was 3 days (range: 1 to 51 days, although onset after 10 days is rare). Half of ALL patients with CRS received tocilizumab and some patients required addition of corticosteroids (methylprednisolone). Approximately one-fifth of patients with DLBCL received tocilizumab or corticosteroids. Some patients required 2 or 3 doses of tocilizumab. In rare instances, patients with DLBCL received corticosteroids without tocilizumab for CRS management; corticosteroids were used for persistent neurotoxicity following resolution of CRS (also rare). The median time to resolution of CRS was 8 days (range: 1 to 36 days). Key manifestations of CRS include fever, hypotension, hypoxia, and tachycardia, and may be associated with hepatic, renal, and cardiac dysfunction, and coagulopathy. Risk factors for severe CRS in patients with ALL are high pre-infusion tumor burden (>50% blasts in bone marrow), uncontrolled or accelerating tumor burden following lymphodepleting chemotherapy (fludarabine and cyclophosphamide), active infections, and/or inflammatory processes; risk factors for developing severe CRS in DLBCL are not known. Delay tisagenlecleucel infusion after lymphodepleting chemotherapy for unresolved serious adverse reactions from preceding chemotherapies (including pulmonary toxicity, cardiac toxicity, or hypotension), active uncontrolled infection, active graft versus host disease (GVHD), or worsening leukemia burden. Ensure that tocilizumab is available (a minimum of 2 doses) on site prior to tisagenlecleucel infusion. Monitor for signs or symptoms of CRS for at least 4 weeks after treatment (monitor 2 to 3 times during the first week after infusion). Patients should seek immediate medical attention if signs or symptoms of CRS occur at any time. Evaluate patients immediately at the first sign of CRS; hospitalize and begin supportive care, tocilizumab and/or corticosteroids as indicated.
• Cytopenias: Prolonged cytopenias may occur several weeks after lymphodepleting chemotherapy and tisagenlecleucel infusion. Unresolved (by day 28 following tisagenlecleucel treatment) grade 3 or higher cytopenias included neutropenia and thrombocytopenia; some patients still experienced grade 3 or higher neutropenia or thrombocytopenia at 56 days post infusion. Prolonged neutropenia is associated with an increased risk of infection. Myeloid growth factors, particularly GM-CSF (sargramostim), are not recommended during the first 3 weeks after tisagenlecleucel infusion or until CRS has resolved.
• Hepatitis B virus reactivation: Hepatitis B virus (HBV) reactivation (sometimes resulting in fulminant hepatitis, hepatic failure and death) can occur in patients treated with medications directed against B cells. Screen for HBV, HCV, and HIV in accordance with clinical guidelines prior to collection of cells for manufacturing.
• Hypersensitivity: Allergic reactions may occur with tisagenlecleucel infusion. Serious hypersensitivity reactions, including anaphylaxis, may occur due to the dimethyl sulfoxide (DMSO) or dextran 40 components in tisagenlecleucel.
• Hypogammaglobulinemia: Hypogammaglobulinemia and IgG agammaglobulinemia related to B-cell aplasia may occur in patients with a complete remission (CR) after tisagenlecleucel infusion. Monitor immunoglobulin levels after tisagenlecleucel treatment. Manage hypogammaglobulinemia with infection precautions, antibiotic prophylaxis and immunoglobulin treatment (per standard replacement guidelines).
• Infection: Infections (including life-threatening or fatal infections) occurred in patients after tisagenlecleucel infusion, including grades 3 and higher infections. Begin prophylaxis according to local guidelines prior to tisagenlecleucel infusion. Delay tisagenlecleucel infusion for active uncontrolled infection until after resolution. Monitor for signs and symptoms of infection following treatment and manage appropriately. Neutropenic fever (grade 3 or higher) has been observed after tisagenlecleucel infusion and may occur concurrently with CRS. If neutropenic fever occurs, evaluate for infection and manage with broad spectrum antibiotics, fluids and other supportive care as clinically indicated.
• Neurological toxicities: [US Boxed Warning]: Neurological toxicities, which may be severe or life-threatening, can occur following treatment with tisagenlecleucel, and may occur concurrently with CRS. Monitor for neurological events after treatment and provide supportive care as needed; if neurologic symptoms occur, exclude other causes. Monitor for neurotoxicity 2 to 3 times during the first week following infusion. Most neurological toxicities occurred within 8 weeks following tisagenlecleucel infusion. The median time to the first event was 6 days (range: 1 to 359 days) from infusion and the median duration was 6 days (ALL) and 14 days (DLBCL). Neurotoxicity generally resolved within 21 days of onset, although encephalopathy lasting up to 50 days was reported. Grade 3 and higher neurologic toxicities have been observed. The most common neurological toxicities were headache, encephalopathy, delirium, anxiety, sleep disorders, dizziness, tremor, and peripheral neuropathy; other manifestations included seizures, mutism, and aphasia. The onset of neurologic toxicity may be concurrent with CRS, following resolution of CRS, or in the absence of CRS. Due to the potential for neurologic events, including altered mental status or seizures, patients receiving tisagenlecleucel are at risk for altered or decreased consciousness or coordination in the 8 weeks following administration; during this initial period, advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery.
• Secondary malignancy: Patients treated with tisagenlecleucel may develop secondary malignancies or cancer recurrence. Monitor (life-long) for secondary malignancies. If a secondary malignancy occurs, contact the manufacturer (1-844-4KYMRIAH) to obtain patient sampling instructions for testing.
Concurrent drug therapy issues:
• Immunizations: Vaccination with live virus vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during tisagenlecleucel treatment, and until immune recovery following treatment. The safety of immunization with live viral vaccines during or following tisagenlecleucel treatment has not been studied.
Other warnings/precautions:
• Appropriate use: For autologous use only. Confirm availability of tisagenlecleucel prior to starting lymphodepleting regimen. Confirm patient identity and match to patient identifiers on the infusion bag(s) prior to infusion. The manufacturer recommends administering at a certified facility and monitoring 2 to 3 times during the first week following infusion for signs/symptoms of CRS and neurotoxicity. Patients should remain within proximity of the certified facility for at least 4 weeks following infusion.
• REMS program: [US Boxed Warning]: Tisagenlecleucel is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the KYMRIAH REMS. Information is available at http://www.kymriah-rems.com or 1-844-4KYMRIAH.
Monitoring Parameters
Screen for HBV, HCV, and HIV (prior to collection of cells for manufacturing). Monitor immunoglobulin levels (after treatment). Evaluate pregnancy status (prior to therapy in sexually active females of reproductive potential).
Monitor for signs/symptoms of CRS and neurotoxicity 2 to 3 times during the first week following infusion; monitor for signs/symptoms of CRS for at least 4 weeks after treatment (evaluate immediately at the first sign of CRS), monitor for hypersensitivity reactions, neurologic toxicity, signs/symptoms of infection. Monitor (life-long) for secondary malignancies.
Reproductive Considerations
Evaluate pregnancy status prior to use in females of reproductive potential. The duration of contraception needed following tisagenlecleucel administration is not known.
Pregnancy Considerations
Based on the mechanism of action, if placental transfer were to occur, fetal toxicity, including B-cell lymphocytopenia, may occur. Pregnant women who have received tisagenlecleucel may have hypogammaglobulinemia; assess immunoglobulin levels in newborns of mothers treated with tisagenlecleucel.
Data collection to monitor pregnancy and infant outcomes following exposure to tisagenlecleucel is ongoing. Pregnancies that may occur during treatment should be reported to Novartis Pharmaceuticals Corporation (888-669-6682).
Patient Education
What is this drug used for?
• It is used to treat a type of leukemia.
• It is used to treat a type of lymphoma.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Lack of appetite
• Nausea
• Vomiting
• Diarrhea
• Constipation
• Abdominal pain
• Painful extremities
• Muscle pain
• Joint pain
• Back pain
• Weight loss
• Stuffy nose
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Cytokine release syndrome like chills, dizziness, loss of strength and energy, fever, headache, passing out, rash, swelling in your throat, trouble breathing, nausea, vomiting, or wheezing
• Infection
• Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
• Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
• Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
• Electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, seizures, lack of appetite, or severe nausea or vomiting
• Anxiety
• Confusion
• Nervousness
• Agitation
• Restlessness
• Vision changes
• Dizziness
• Passing out
• Sensing things that seem real but are not
• Headache
• Seizures
• Tremors
• Trouble speaking
• Behavioral changes
• Mood changes
• Shortness of breath
• Excessive weight gain
• Swelling of arms or legs
• Fast breathing
• Severe loss of strength and energy
• Fast heartbeat
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine’s uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
Biological Products Related to tisagenlecleucel
Find detailed information on biosimilars for this medication.
Frequently asked questions
More about tisagenlecleucel
- Check interactions
- Compare alternatives
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.