niCARdipine Hydrochloride (Monograph)
Brand name: Cardene
Drug class: Dihydropyridines
Introduction
Calcium-channel blocking agent; dihydropyridine derivative.
Uses for niCARdipine Hydrochloride
Hypertension
Oral management of hypertension (alone or in combination with other classes of antihypertensive agents).
Therapy with extended-release capsules generally is preferred because of less frequent dosing, potentially smoother BP control, and concerns raised by experience with short-acting (conventional, immediate-release) nifedipine.
Calcium-channel blockers are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines; other preferred options include ACE inhibitors, angiotensin II receptor antagonists, and thiazide diuretics. While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Other hypertension guidelines generally based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment is recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg. Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Calcium-channel blockers may be beneficial in hypertensive patients with certain coexisting conditions (e.g., ischemic heart disease) and in geriatric patients, including those with isolated systolic hypertension.
Calcium-channel blockers may be particularly useful in black patients with hypertension; such patients generally respond better to monotherapy with calcium-channel blockers or thiazide diuretics than to other antihypertensive drug classes (e.g., ACE inhibitors, angiotensin II receptor antagonists). However, the combination of an ACE inhibitor or an angiotensin II receptor antagonist with a calcium-channel blocker or thiazide diuretic produces similar BP lowering in black patients as in other racial groups.
IV, short-term management of hypertension when oral therapy is not feasible or desirable.
IV management of hypertensive crises (e.g., emergencies) in adults.
IV, rapid reduction of BP in the management of acute severe hypertension and life-threatening symptoms in children and adolescents† [off-label].
Angina
Management of chronic stable angina pectoris (alone or in combination with other antianginal agents).
niCARdipine Hydrochloride Dosage and Administration
General
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, thiazide diuretic). Many patients will require ≥2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved with 2 antihypertensive agents, add a third drug.
Severe Hypertension and Hypertensive Emergency
-
Adults with a compelling indication—severe preeclampsia or eclampsia or pheochromocytoma crisis: Reduce SBP to <140 mm Hg during the first hour.
-
Adults with a compelling indication—acute aortic dissection: Reduce SBP to <120 mm Hg within the first 20 minutes.
-
Initial goal of IV therapy in adults with a hypertensive emergency without a compelling indication is to reduce SBP by ≤25% within the first hour, followed by further BP reduction if stable to 160/110 or 160/100 mm Hg within the next 2–6 hours, avoiding excessive declines in BP that could precipitate renal, cerebral, or coronary ischemia. If this BP is well tolerated and the patient is clinically stable, may implement further gradual reductions toward normal BP in the next 24–48 hours.
-
Children and adolescents: Reduce BP by ≤25% of the planned reduction over the first 8 hours.
Administration
Administer orally or by IV infusion.
Oral Administration
Conventional Capsules
Administer orally 3 times daily.
Extended-release Capsules
Administer orally twice daily.
IV Administration
Administer by slow, continuous IV infusion.
Some experts state drug may be administered by direct IV (“bolus”) injection in children and adolescents with acute severe hypertension and life-threatening symptoms.
Must dilute commercially available injection concentrate containing 2.5 mg/mL with a compatible IV infusion solution prior to administration.
Alternatively, administer as premixed solution (0.1 mg/mL in either 4.8% dextrose or 0.86% sodium chloride injection, 0.2 mg/mL in either 5% dextrose or 0.83% sodium chloride injection).
If administered via a peripheral vein, change infusion site every 12 hours to minimize risk of venous irritation.
Monitor BP closely during and after completion of IV administration; avoid rapid or excessive reduction in systolic or diastolic BP.
Dilution
Injection concentrate: Dilute each 25-mg ampul containing 2.5 mg/mL with 240 mL of a compatible IV solution to provide a solution containing 0.1 mg/mL.
Standardize 4 Safety
Standardized concentrations for nicardipine have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Multidisciplinary expert panels were convened to determine recommended standard concentrations. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web].
dosing units differ from concentration units
|
Patient Population |
Concentration Standards |
Dosing Units |
|---|---|---|
|
Adults |
0.1 mg/mL |
mg/hour |
|
0.2 mg/mL |
||
|
Pediatric patients (<50 kg) |
0.1 mg/mL |
mcg/kg/min |
|
0.2 mg/mL |
||
|
0.5 mg/mL |
Dosage
Available as nicardipine hydrochloride; dosage is expressed in terms of the salt.
Pediatric Patients
Acute Severe Hypertension† [off-label]
Rapid Reduction of BP† [off-label]
IVDirect IV (“bolus”) injection: 30 mcg/kg (up to 2 mg) per dose.
IV infusion: 0.5–4 mcg/kg per minute.
Adults
Hypertension
Conventional Capsules
OralInitially, 20 mg 3 times daily.
Adjust dosage according to patient’s peak (approximately 1–2 hours after dosing, particularly during initiation of therapy) and trough (8 hours after dosing) BP responses, but generally no more frequently than at 3-day intervals.
Usual dosage is 20–40 mg 3 times daily.
Extended-Release Capsules
OralInitially, 30 mg twice daily.
Adjust dosage according to BP response 2–4 hours after dosing as well as just prior to next dose.
Usual dosage range is 30–60 mg twice daily.
Switching to Extended-Release Capsules
OralTotal daily dose of conventional tablets not a useful guide to judging effective dose of extended-release capsules. However, may administer the currently effective total daily dose of conventional capsules and adjust dosage according to BP response.
Short-term Management with IV Therapy
IVInitially, 5 mg/hour.
If target BP is not achieved, increase rate by 2.5 mg/hour every 15 minutes, up to 15 mg/hour.
For more rapid reduction, initially, 5 mg/hour. If the target BP is not achieved, increase rate by 2.5 mg/hour every 5 minutes, up to 15 mg/hour.
Following achievement of desired BP response, decrease rate to 3 mg/hour; adjust rate as necessary to maintain desired BP response.
Conversion From Oral to IV Therapy
IV|
Oral Dosage (as Conventional Capsules) |
Equivalent IV Infusion Rates |
|---|---|
|
20 mg every 8 hours |
0.5 mg/hour |
|
30 mg every 8 hours |
1.2 mg/hour |
|
40 mg every 8 hours |
2.2 mg/hour |
Hypertensive Emergency
IV5–15 mg/hour; adjust according to BP response and tolerance.
Angina
Conventional Capsules
OralInitially, 20 mg 3 times daily. Adjust dosage according to patient tolerance and response at ≥3-day intervals.
Usual dosage range is 20–40 mg 3 times daily.
Prescribing Limits
Adults
Hypertension
IV
15 mg/hour.
Special Populations
Hepatic Impairment
Conventional capsules: Initially, 20 mg twice daily in patients with severe hepatic impairment. Individualize dosage, but maintain a twice-daily dosing schedule.
IV infusion: Consider dosage reduction. Use with caution in patients with portal hypertension.
Renal Impairment
Conventional capsules: Initially, 20 mg 3 times daily. Titrate dosage carefully.
Extended-release capsules: Initially, 30 mg twice daily. Titrate dosage carefully.
IV infusion: Titrate dosage carefully.
Geriatric Patients
Cautious dosing recommended. For conventional and extended-release capsules, initiate therapy at low end of dosage range.
Cautions for niCARdipine Hydrochloride
Contraindications
-
Known hypersensitivity to nicardipine or any ingredient in the formulation.
-
Advanced aortic stenosis, since reduction in diastolic pressure may worsen myocardial oxygen balance.
Warnings/Precautions
Warnings
Increased Angina
Increased frequency, duration, and severity of angina upon initiation or dosage increase of calcium channel blockers.
Heart Failure
Use with caution in patients with heart failure or substantial left ventricular dysfunction, especially in those receiving concomitant β-adrenergic blocking agents.
β-Blocker Withdrawal
Taper dosage of β-adrenergic blocking agent, preferably over 8–10 days before initiation of nicardipine. Nicardipine is not a β-adrenergic blocking agent and offers no protection against abrupt withdrawal of these agents.
General Precautions
Hypotension
Possible symptomatic hypotension from decreased peripheral resistance. Use with caution in patients with acute cerebral infarction or hemorrhage; avoid systemic hypotension in these patients.
Monitor BP carefully, especially during initiation of therapy or upward adjustment of dosage.
Pheochromocytoma
Limited clinical experience in patients with hypertension associated with pheochromocytoma. Use with caution.
Specific Populations
Pregnancy
Category C.
Lactation
Distributed into milk in high concentrations in rats. Use not recommended.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Some experts recommend use in children and adolescents† [off-label] for acute severe hypertension with life-threatening symptoms.
Use with caution for rapid reduction of BP in children and adolescents† [off-label] ; may cause reflex tachycardia.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Select dosage with caution; initiate dosage at lower end of recommended range.
Hepatic Impairment
Use with caution in patients with hepatic impairment or reduced hepatic blood flow; dosage adjustments recommended. (See Hepatic Impairment under Dosage and Administration.)
Use of extended-release capsules has not been studied in patients with severe hepatic impairment.
Renal Impairment
Use with caution; careful dosage titration recommended. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
With oral therapy, pedal edema, dizziness, headache, asthenia, flushing, increased angina, vasodilation, palpitation.
With IV therapy, headache, hypotension, nausea/vomiting, tachycardia.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids (magnesium hydroxide) |
Pharmacokinetic interaction unlikely |
|
|
β-Adrenergic blockers (e.g., propranolol) |
Pharmacokinetic interaction (e.g., effect on plasma protein binding of nicardipine) unlikely |
|
|
Cimetidine |
Increased plasma nicardipine concentrations |
Monitor carefully |
|
Cyclosporine |
Increased plasma cyclosporine concentrations |
Monitor plasma cyclosporine concentrations closely and adjust dosage accordingly |
|
Digoxin |
Potential for increased plasma digoxin concentrations |
Monitor serum digoxin concentrations |
|
Dipyridamole |
No effect on plasma protein binding of nicardipine |
|
|
Fentanyl |
Potential for severe hypotension with concomitant use of a β-adrenergic blocker and a calcium channel blocker |
Increase circulating fluid volume if hypotension occurs |
|
Furosemide |
No effect on plasma protein binding of nicardipine |
|
|
Naproxen |
No effect on plasma protein binding of nicardipine |
|
|
Quinidine |
No effect on plasma protein binding of nicardipine |
|
|
Warfarin |
No effect on plasma protein binding of nicardipine |
niCARdipine Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Completely absorbed from the GI tract following oral administration; peak plasma concentrations of conventional and extended-release capsules are attained within 0.5–2 and 1–4 hours, respectively.
Minimum plasma levels of equivalent doses of conventional and extended-release capsules are similar.
Bioavailability of conventional capsules is about 35%; extended-release capsules have a slightly lower bioavailability, except at the highest doses.
Food
High-fat meal decreases bioavailability of conventional and extended-release capsules.
Special Populations
In patients with severe hepatic impairment, peak plasma concentrations and AUC increased by 1.8 and 4-fold, respectively, and terminal half-life prolonged to 19 hours.
In patients with moderate renal impairment, peak plasma concentrations and AUC increased by 2- to 3-fold following administration of conventional or extended-release capsules.
Distribution
Extent
Distributed into milk in rats.
Plasma Protein Binding
>95%.
Elimination
Metabolism
Extensively metabolized in the liver.
Elimination Route
Excreted in urine (49–60%) and feces (35–43%).
Half-life
Multi-phasic; terminal elimination half-life is 8.6 and 14.4 hours following oral and IV administration, respectively.
Stability
Storage
Oral
Conventional Capsules and Extended-release Capsules
Light resistant containers at 15–30°C.
Parenteral
Injection Concentrate
20–25°C; protect from light. Avoid exposure to increased temperatures.
Premixed Injection for Infusion
20–25°C; protect from light, freezing, and excessive heat.
Actions
-
Inhibits transmembrane influx of extracellular calcium ions across the membranes of myocardial cells and vascular smooth muscle cells, without changing serum calcium concentrations.
-
Peripheral arterial vasodilator; acts directly on vascular smooth muscle causing reduction in peripheral vascular resistance (afterload) and BP.
Advice to Patients
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
20 mg* |
Nicardipine Hydrochloride Capsules |
|
|
30 mg* |
Nicardipine Hydrochloride Capsules |
|||
|
Capsules, extended-release |
30 mg |
Cardene SR |
Chiesi |
|
|
60 mg |
Cardene SR |
Chiesi |
||
|
Parenteral |
For injection, concentrate, for IV infusion |
2.5 mg/mL* |
Cardene I.V. |
Chiesi |
|
Nicardipine Hydrochloride Injection |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for IV infusion |
0.1 mg/mL (20 mg) in 4.8% Dextrose |
Cardene I.V. |
Chiesi |
|
0.2 mg/mL (40 mg) in 5% Dextrose |
Cardene I.V. |
Chiesi |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for IV infusion |
0.1 mg/mL (20 mg) in 0.86% Sodium Chloride |
Cardene I.V. |
Chiesi |
|
0.2 mg/mL (40 mg) in 0.83% Sodium Chloride |
Cardene I.V. |
Chiesi |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about nicardipine
- Check interactions
- Compare alternatives
- Pricing & coupons
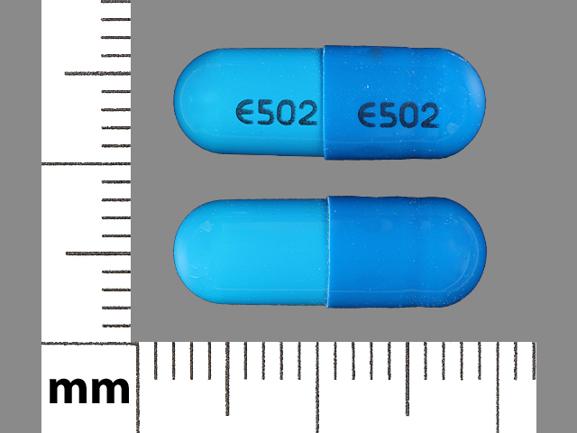
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: calcium channel blockers
- Breastfeeding
- En español