Ferric Citrate (Monograph)
Brand name: Auryxia
Drug class: Phosphate-reducing Agents
Chemical name: 2-Hydroxy-1,2,3-propanetricarboxylic acid iron (III) hydrate
Molecular formula: C6H5FeO7•nH2O
CAS number: 2338-05-8
Introduction
Phosphate binder used to reduce the intestinal absorption of phosphates.
Uses for Ferric Citrate
Hyperphosphatemia
Reduction of serum phosphorus in patients with chronic kidney disease who are undergoing dialysis.
Ferric Citrate Dosage and Administration
Administration
Oral Administration
Administer orally in divided doses with meals.
Dosage
Adults
Hyperphosphatemia
Oral
Initially, 2 g 3 times daily.
Monitor serum phosphorus concentrations and titrate dosage at intervals of 1 week or longer in decrements or increments of 1–2 g daily as needed to maintain target serum phosphorus concentrations.
Average dosage of 8–9 g daily was required to control serum phosphorus concentrations in a clinical study.
Prescribing Limits
Adults
Hyperphosphatemia
Oral
Maximum 12 g daily.
Special Populations
No special population dosage recommendations.
Cautions for Ferric Citrate
Contraindications
-
Iron overload syndromes (e.g., hemochromatosis).
Warnings/Precautions
Iron Overload
Iron absorption from ferric citrate may lead to excessive elevations in iron stores, especially when IV iron is used concomitantly. Elevations in serum ferritin concentrations and transferrin saturation (TSAT) observed in clinical trials.
Assess iron indices (e.g., serum ferritin and TSAT) prior to initiating ferric citrate and monitor iron indices during therapy. Patients receiving IV iron may require dosage reduction or discontinuance of IV iron.
Accidental Iron Overdosage
Accidental overdosage of iron-containing preparations is a leading cause of fatal poisoning in children <6 years of age. Keep out of reach of children. Contact a clinician or poison control center immediately in case of accidental overdosage.
GI Inflammation or Bleeding
Clinical studies did not include patients with inflammatory bowel disease or active, symptomatic GI bleeding; safety not established in these populations.
Specific Populations
Pregnancy
Category B.
Use caution. Requirements for vitamins and other nutrients are increased during pregnancy; effect of ferric citrate on absorption of vitamins and other nutrients not studied in pregnant women. Iron overdosage may carry a risk for spontaneous abortion, gestational diabetes, and fetal malformation.
Effects on labor and delivery not known.
Lactation
Iron is distributed into milk in rats; breast-fed infants may be exposed to iron from the phosphate binder when ferric citrate is administered to nursing women.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Keep out of reach of children to prevent accidental iron overdosage; iron from ferric citrate can be absorbed systemically.
Geriatric Use
No apparent differences in tolerability or efficacy relative to younger adults.
Common Adverse Effects
Diarrhea, nausea, constipation, vomiting, cough.
Drug Interactions
Effects on GI Absorption of Drugs
Possible decreased bioavailability of orally administered drugs given concomitantly; no empiric data concerning avoidance of interactions between ferric citrate and most oral drugs.
Consider administering ferric citrate and any concomitant drugs at different times if reduced bioavailability would have a clinically important effect on safety or efficacy. The spacing of doses depends on absorption characteristics of the concomitant drug (e.g., time to peak plasma concentration, formulation [i.e., immediate release or extended release]).
Consider monitoring clinical response and/or blood concentrations of concomitant drugs with a narrow therapeutic index.
Nutrients
No formal drug-food interaction studies to date. (See Actions.)
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
β-Adrenergic blockers |
Metoprolol, propranolol: No clinically meaningful interaction in vitro |
Metoprolol, propranolol: May be administered concomitantly with ferric citrate |
|
Amlodipine |
No clinically meaningful interaction in vitro |
May be administered concomitantly |
|
Aspirin |
No clinically meaningful interaction in vitro |
May be administered concomitantly |
|
Clopidogrel |
No clinically meaningful interaction in vitro |
May be administered concomitantly |
|
Digoxin |
No clinically meaningful interaction in vitro |
May be administered concomitantly |
|
Doxycycline |
Extensive binding of doxycycline in vitro |
Administer oral doxycycline at least 1 hour before ferric citrate |
|
Enalapril |
No clinically meaningful interaction in vitro |
May be administered concomitantly |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin, fluvastatin, pravastatin: No clinically meaningful interaction in vitro |
Atorvastatin, fluvastatin, pravastatin: May be administered concomitantly with ferric citrate |
|
Levofloxacin |
No clinically meaningful interaction in vitro |
May be administered concomitantly |
|
Sitagliptin |
No clinically meaningful interaction in vitro |
May be administered concomitantly |
|
Vitamin D analogs |
Calcitriol, doxercalciferol: No clinically meaningful interaction in vitro |
Calcitriol, doxercalciferol: May be administered concomitantly with ferric citrate |
|
Warfarin |
No clinically meaningful interaction in vitro |
May be administered concomitantly |
Ferric Citrate Pharmacokinetics
Absorption
Formal pharmacokinetic studies not performed. Changes in serum iron indices indicate iron from ferric citrate is systemically absorbed.
Stability
Storage
Oral
Tablets
20–25°C (may be exposed to 15–30°C). Protect from moisture.
Actions
-
Ferric iron binds dietary phosphate in GI tract, forming insoluble complex (ferric phosphate) that is excreted in feces.
-
Reduces serum phosphate concentration in dose-dependent manner.
-
Also alters serum iron indices, increasing ferritin, iron, and TSAT.
-
Clinical data suggest ferric citrate does not affect serum concentrations of folate or vitamins A, B12, D, E, or K.
Advice to Patients
-
Importance of adhering to instructions about diet.
-
Importance of taking ferric citrate as directed with meals.
-
Importance of instructing patients about any concomitantly used drugs that should be taken at a different time of day than when ferric citrate is taken.
-
Potential for ferric citrate to cause discolored (dark) stools.
-
Potential for ferric citrate to cause diarrhea, nausea, constipation, and vomiting. Importance of reporting severe or persistent GI symptoms to clinician.
-
Risk of fatal iron poisoning in children <6 years of age. Importance of keeping ferric citrate out of reach of children. Contact a clinician or poison control center immediately in case of accidental overdosage.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
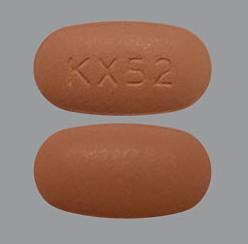
Oral |
Tablets, film-coated |
1 g (equivalent to 210 mg of ferric iron) |
Auryxia |
Keryx |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions September 28, 2015. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about ferric citrate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (8)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: phosphate binders
- Breastfeeding
- En español