Metoclopramide
Generic name: metoclopramide (oral/injection) [ MET-oh-KLOE-pra-mide ]
Brand names: Metozolv ODT, Reglan
Drug classes: GI stimulants, Miscellaneous antiemetics
What is metoclopramide?
Metoclopramide increases muscle contractions in the upper digestive tract. This speeds up the rate at which the stomach empties into the intestines.
Metoclopramide oral (taken by mouth) is used for 4 to 12 weeks to treat heartburn caused by gastroesophageal reflux in people who have used other medications without relief.
Metoclopramide oral is also used to treat gastroparesis (slow stomach emptying) in people with diabetes, which can cause heartburn and stomach discomfort after meals.
Metoclopramide injection is used to treat severe diabetic gastroparesis. The injection is also used to prevent nausea and vomiting caused by chemotherapy or surgery, or to aid in certain medical procedures involving the stomach or intestines.
Warnings
Do not use this medicine if you've ever had muscle movement problems after using metoclopramide or similar medicines, or if you've had a movement disorder called tardive dyskinesia. You also should not use this medicine if you've had stomach or intestinal problems (a blockage, bleeding, or a hole or tear), epilepsy or other seizure disorder, or an adrenal gland tumor (pheochromocytoma).
NEVER USE METOCLOPRAMIDE IN LARGER AMOUNTS THAN RECOMMENDED, OR FOR LONGER THAN 12 WEEKS. High doses or long-term use can cause a serious movement disorder that may not be reversible. The longer you use metoclopramide, the more likely you are to develop this movement disorder. The risk of this side effect is higher in diabetics and older adults (especially women).
Before you take metoclopramide, tell your doctor if you have kidney or liver disease, congestive heart failure, high blood pressure, diabetes, Parkinson's disease, or a history of depression.
Do not drink alcohol. It can increase some of the side effects of metoclopramide.
Stop using metoclopramide and call your doctor at once if you have tremors or uncontrolled muscle movements, fever, stiff muscles, confusion, sweating, fast or uneven heartbeats, rapid breathing, depressed mood, thoughts of suicide or hurting yourself, hallucinations, anxiety, agitation, seizure, or jaundice (yellowing of your skin or eyes).
Before taking this medicine
You should not use metoclopramide if you are allergic to it, or if you have:
-
tardive dyskinesia (a disorder of involuntary movements);
-
stomach or intestinal problems such as a blockage, bleeding, or perforation (a hole or tear in your stomach or intestines);
-
epilepsy or other seizure disorder;
-
an adrenal gland tumor (pheochromocytoma); or
-
if you've ever had muscle movement problems after using metoclopramide or similar medicines.
Tell your doctor if you have ever had:
-
liver or kidney disease;
-
problems with muscle movements;
-
congestive heart failure or a heart rhythm disorder;
-
diabetes; or
-
depression or mental illness.
This medicine may contain phenylalanine. Check the medication label if you have phenylketonuria (PKU).
Tell your doctor if you are pregnant. Metoclopramide may harm an unborn baby if you use the medicine during late pregnancy.
It may not be safe to breast-feed a baby while you are using this medicine. Ask your doctor about any risks.
Metoclopramide is not approved for use by anyone younger than 18 years old.
How should I use metoclopramide?
Take metoclopramide exactly as prescribed by your doctor. Follow the directions on your prescription label and read all medication guides. Use the medicine exactly as directed.
A metoclopramide injection is given into a muscle or as an infusion into a vein. A healthcare provider will give the injection, usually during surgery, chemotherapy, or a medical procedure.
Metoclopramide oral is taken for only 4 to 12 weeks.
NEVER USE METOCLOPRAMIDE IN LARGER AMOUNTS THAN RECOMMENDED, OR FOR LONGER THAN 12 WEEKS. High doses or long-term use of metoclopramide can cause a serious movement disorder that may not be reversible. The longer you use metoclopramide, the more likely you are to develop this movement disorder. The risk of this side effect is higher in diabetics and older adults (especially women).
Metoclopramide is usually taken 30 minutes before meals and at bedtime, or only with meals that usually cause heartburn. Follow your doctor's dosing instructions very carefully.
Do not use two different forms of metoclopramide (such as tablets and oral syrup) at the same time.
Measure liquid medicine carefully. Use the dosing syringe provided, or use a medicine dose-measuring device (not a kitchen spoon).
To take the orally disintegrating tablet (ODT):
-
Remove a tablet from its blister pack only when you are ready to take the tablet. Use dry hands and take care not to damage a tablet while pushing it out of the blister.
-
Place the tablet in your mouth and allow it to dissolve, without chewing or swallowing it whole. You may sip liquid if needed to help swallow the dissolved tablet.
Store at room temperature in a tightly-closed container, away from moisture and heat. Keep the bottle tightly closed.
After you stop taking metoclopramide, you may have unpleasant withdrawal symptoms such as headache, dizziness, or nervousness.
Dosing information
Usual Adult Dose for Nausea/Vomiting:
Postoperative nausea and vomiting:
Parenteral: 10 to 20 mg IM at or near the end of surgery
Usual Adult Dose for Gastroesophageal Reflux Disease:
Oral: 10 to 15 mg up to 4 times a day 30 minutes before meals and at bedtime, depending upon symptoms being treated and clinical response. Therapy should not exceed 12 weeks.
Usual Adult Dose for Small Intestine Intubation:
If the tube has not passed the pylorus with conventional methods in 10 minutes, a single (undiluted) dose may be administered IV slowly over 1 to 2 minutes:
Adults and pediatric patients greater than or equal to 14 years: 10 mg IV as a single dose administered over 1 to 2 minutes.
Usual Adult Dose for Radiographic Exam:
Adults and pediatric patients greater than or equal to 14 years: 10 mg IV as a single dose administered over 1 to 2 minutes to facilitate gastric emptying where delayed gastric emptying interferes with radiological examination of the stomach and/or small intestine.
Usual Adult Dose for Gastroparesis:
During the earliest manifestations of diabetic gastric stasis, oral administration may be initiated. If severe symptoms are present, therapy should begin with IM or IV administration for up to 10 days until symptoms subside at which time the patient can be switched to oral therapy. Since diabetic gastric stasis is often recurrent, therapy should be reinstituted at the earliest manifestation.
Parenteral: 10 mg 4 times daily, IV (slowly over a 1 to 2 minute period) or IM for up to 10 days.
Oral: 10 mg 4 times daily, 30 minutes before meals and at bedtime, for 2 to 8 weeks depending on clinical response.
Usual Adult Dose for Nausea/Vomiting -- Chemotherapy Induced:
IV infusion: 1 to 2 mg/kg/dose (depending on the emetogenic potential of the agent) IV (infused over a period of not less than 15 minutes) 30 minutes before administration of chemotherapy. The dose may be repeated twice at 2 hour intervals following the initial dose. If vomiting is still not suppressed, the same dose may be repeated 3 more times at 3 hour intervals.
For doses higher than 10 mg, the injection should be diluted in 50 mL of a parenteral solution. Normal saline is the preferred diluent.
If acute dystonic reactions occur, 50 mg of diphenhydramine hydrochloride may be injected IM.
Usual Adult Dose for Migraine:
Use for treatment of migraine headaches is not an FDA approved indication; however, metoclopramide has shown efficacy in studies at a dose of 10 to 20 mg IV once (used in combination with analgesics or ergot derivatives).
Usual Pediatric Dose for Gastroesophageal Reflux Disease:
Metoclopramide is not approved by the FDA for gastroesophageal reflux disease in pediatric patients; however, the following doses have been studied:
Oral, IM, IV:
Infants and Children: 0.4 to 0.8 mg/kg/day in 4 divided doses
Usual Pediatric Dose for Small Intestine Intubation:
Metoclopramide IV is approved by the FDA for pediatric use to facilitate small bowel intubation by causing gastric emptying where delayed gastric emptying interferes with radiological examination of the stomach and/or small intestine.
If the tube has not passed the pylorus with conventional methods in 10 minutes, a single (undiluted) dose may be administered IV slowly over 1 to 2 minutes:
Less than 6 years: 0.1 mg/kg IV as a single dose
6 to 14 years: 2.5 to 5 mg IV as a single dose
Children greater than 14 years: 10 mg as a single dose
Usual Pediatric Dose for Nausea/Vomiting -- Chemotherapy Induced:
Metoclopramide is not approved by the FDA for chemotherapy induced nausea and vomiting in pediatric patients; however, the following doses have been studied:
IV:
1 to 2 mg/kg/dose IV every 30 minutes before chemotherapy and every 2 to 4 hours
Usual Pediatric Dose for Nausea/Vomiting -- Postoperative:
Metoclopramide is not approved by the FDA for postoperative nausea and vomiting in pediatric patients; however, the following doses have been studied:
IV:
Children less than or equal to 14 years: 0.1 to 0.2 mg/kg/dose (maximum dose: 10 mg/dose); repeat every 6 to 8 hours as needed
Children greater than 14 years and Adults: 10 mg; repeat every 6 to 8 hours as needed
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. Overdose symptoms may include drowsiness, confusion, or uncontrolled muscle movements.
What to avoid
Drinking alcohol with this medicine can cause side effects.
Avoid driving or hazardous activity until you know how this medicine will affect you. Your reactions could be impaired.
Metoclopramide side effects
Get emergency medical help if you have signs of an allergic reaction to metoclopramide: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Stop taking metoclopramide and call your doctor at once if you have any of these SIGNS OF A SERIOUS MOVEMENT DISORDER, which may occur within the first 2 days of treatment:
-
tremors or shaking in your arms or legs;
-
uncontrolled muscle movements in your face (chewing, lip smacking, frowning, tongue movement, blinking or eye movement); or
-
any new or unusual muscle movements you cannot control.
Call your doctor at once if you have:
-
confusion, depression, thoughts of suicide or hurting yourself;
-
slow or jerky muscle movements, problems with balance or walking;
-
mask-like appearance in your face;
-
a seizure;
-
anxiety, agitation, jittery feeling, trouble staying still, trouble sleeping;
-
swelling, feeling short of breath, rapid weight gain; or
-
severe nervous system reactionvery stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out.
Common metoclopramide side effects may include:
-
feeling restless;
-
feeling drowsy or tired;
-
lack of energy;
-
nausea, vomiting;
-
headache, confusion; or
-
sleep problems (insomnia).
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
What other drugs will affect metoclopramide?
Using metoclopramide with other drugs that make you drowsy can worsen this effect. Ask your doctor before you take opioid pain medication, a sleeping pill, a muscle relaxer, or medicine for anxiety, depression, or seizures.
Tell your doctor about all your current medicines. Many drugs can affect metoclopramide, especially:
-
acetaminophen (Tylenol);
-
cyclosporine (Gengraf, Neoral, Sandimmune);
-
digoxin (digitalis, Lanoxin);
-
glycopyrrolate (Robinul);
-
insulin;
-
levodopa (Larodopa, Atamet, Parcopa, Sinemet);
-
mepenzolate (Cantil);
-
tetracycline (Ala-Tet, Brodspec, Panmycin, Sumycin, Tetracap);
-
atropine (Donnatal, and others), benztropine (Cogentin), dimenhydrinate (Dramamine), methscopolamine (Pamine), or scopolamine (Transderm-Scop);
-
bladder or urinary medications such as darifenacin (Enablex), flavoxate (Urispas), oxybutynin (Ditropan, Oxytrol), tolterodine (Detrol), or solifenacin (Vesicare);
-
blood pressure medications;
-
bronchodilators such as ipratroprium (Atrovent) or tiotropium (Spiriva);
-
irritable bowel medications such as dicyclomine (Bentyl), hyoscyamine (Anaspaz, Cystospaz, Levsin), or propantheline (Pro-Banthine);
-
an MAO inhibitor such as furazolidone (Furoxone), isocarboxazid (Marplan), phenelzine (Nardil), rasagiline (Azilect), selegiline (Eldepryl, Emsam, Zelapar), or tranylcypromine (Parnate); or
-
medicines to treat psychiatric disorders, such as chlorpromazine (Thorazine), clozapine (Clozaril, FazaClo), haloperidol (Haldol), olanzapine (Zyprexa, Symbyax), prochlorperazine (Compazine), risperidone (Risperdal), thiothixene (Navane), and others.
This list is not complete and there are many other drugs that can interact with metoclopramide. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
More about metoclopramide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (524)
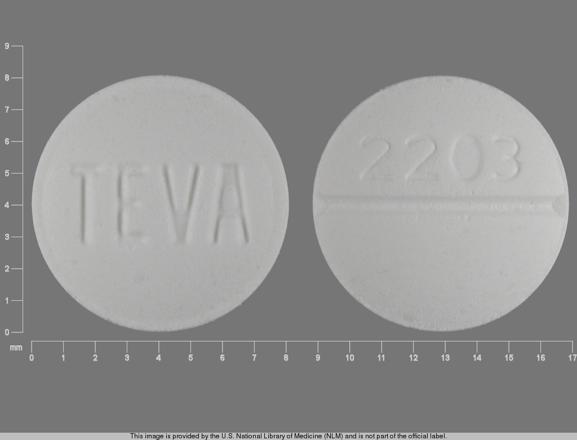
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: GI stimulants
- Breastfeeding
Patient resources
Other brands
Professional resources
- Metoclopramide monograph
- Metoclopramide Injection (FDA)
- Metoclopramide Oral Solution (FDA)
- Metoclopramide Orally DisintegratingTablets (FDA)
- Metoclopramide Tablets (FDA)
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use metoclopramide only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2025 Cerner Multum, Inc. Version: 14.01.