Ethacrynic Acid (Monograph)
Brand names: Edecrin, Sodium Edecrin
Drug class: Loop Diuretics
- Diuretics, Loop
VA class: CV702
Warning
-
Ethacrynic acid is a potent diuretic which, if given in excessive amounts, can lead to a profound diuresis with water and electrolyte depletion.129 (See Electrolyte, Fluid, and Renal Effects under Cautions.)
-
Careful medical supervision is required; dosage selection and titration should be adjusted to the individual patient’s needs. (See Dosage and Administration.)129
Introduction
A loop-type diuretic129 and antihypertensive agent.b
Uses for Ethacrynic Acid
Edema
Management of edema associated with heart failure, hepatic cirrhosis, and renal disease (e.g., nephrotic syndrome).129
Considered a diuretic of choice for most patients with heart failure.524
Most experts state that all patients with symptomatic heart failure who have evidence for, or a history of, fluid retention generally should receive diuretic therapy in conjunction with moderate sodium restriction, an agent to inhibit the renin-angiotensin-aldosterone (RAA) system (e.g., ACE inhibitor, angiotensin II receptor antagonist, angiotensin receptor-neprilysin inhibitor [ARNI]), a β-adrenergic blocking agent (β-blocker), and in selected patients, an aldosterone antagonist.524 700 713
Short-term management of ascites associated with malignancy, idiopathic edema, or lymphedema.129
Short-term management of hospitalized pediatric patients, other than infants, with congenital heart disease or nephrotic syndrome.129 (See Pediatric Use under Cautions.)
IV ethacrynate sodium is used when rapid onset of diuresis is needed (e.g., acute pulmonary edema).129
Hypertension
Has been used in the management of hypertension† [off-label].b However, not a recommended agent in current hypertension management guidelines.501 502 503 504 1200
May still be considered when diuretic therapy is indicated in patients hypersensitive to sulfonamides (e.g., other loop diuretics, thiazides) because ethacrynic acid is not a sulfonamide.103 104 130
IV ethacrynate sodium has been used as an adjunct to hypotensive agents in the management of hypertensive crisis† [off-label], especially when accompanied by pulmonary edema.b
Hypercalcemia
IV ethacrynate sodium has been used in the management of hypercalcemia† [off-label], alone or with sodium chloride 0.9% injection.b
Ethylene Glycol or Bromide Poisoning
Has been used with mannitol in the management of ethylene glycol poisoning† [off-label].b
Management of bromide intoxication† [off-label].b
Diabetes Insipidus
Treatment of nephrogenic diabetes insipidus† that is refractory to vasopressin or chlorpropamide.b
Ethacrynic Acid Dosage and Administration
General
Edema
-
Careful etiologic diagnosis should precede the use of any diuretic.b
-
Hospitalization of the patient during initiation of therapy is advisable, especially for patients with hepatic cirrhosis and ascites or chronic renal failure.b
-
In prolonged diuretic therapy, intermittent use of the drug (e.g., on 2-4 consecutive days each week) may be advisable.b
-
For the management of fluid retention associated with heart failure (e.g., edema), experts state that diuretics should be administered at a dosage sufficient to achieve optimal volume status and relieve congestion without inducing an excessively rapid reduction in intravascular volume, which could result in hypotension, renal dysfunction, or both.524
Administration
Administer ethacrynic acid orally. 129 b Administer ethacrynate sodium by IV infusion or slow IV injection.129 b Do not administer ethacrynate sodium sub-Q or IM because of local pain and irritation.129 b
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Use IV administration when a rapid onset of diuresis is desired (e.g., acute pulmonary edema, impaired GI absorption, in patients unable to take the drug orally).129 b
Reconstitution
Reconstitute vial containing ethacrynate sodium equivalent to 50 mg of ethacrynic acid with 50 mL of 5% dextrose injection or 0.9% sodium chloride injection to provide a solution containing 1 mg of ethacrynic acid per mL.129 b
Do not use if solution is hazy or opalescent, which may occur if reconstituted with 5% dextrose injection having a pH <5. 129
Rate of Administration
Infuse slowly over 20–30 minutes through the tubing of a running IV infusionb or by direct IV injection over several minutes.129 b
Dosage
Available as ethacrynic acid and ethacrynate sodium; dosage expressed in terms of ethacrynic acid.129 b
Select dosage carefully to prevent a more rapid or substantial loss of fluid or electrolyte than is indicated or necessary.129 (See Electrolyte, Fluid, and Renal Effects under Cautions.)
Weigh patients under standard conditions before initiating and during diuretic therapy.129
Adjust dosage according to patient’s requirements and response.b In adults, use smallest dosage required to produce gradual weight loss of 0.45–0.9 kg (1–2 pounds) daily.129
Some clinicians suggest not to give the drug for more than 2 consecutive days until the patient’s responsiveness is known.b
Pediatric Patients
Edema
Oral
Hospitalized pediatric patients excluding infants: Initially 25 mg.129 Increase with caution in 25-mg increments daily until desired effect is achieved.129 Once desired response is obtained, may reduce dosage to the minimum required for maintenance.b (See Pediatric Use under Cautions.)
Hypertension†
IV†
Although manufacturer does not recommend IV use in pediatric patients,129 b some clinicians consider 1-mg/kg doses safe and effective in such patients.b
Adults
Edema
Oral
Day 1: 50 mg after a meal129 (preferably in the morning).b
Day 2: 50 mg twice daily after meals, if needed.129
Day 3: 100 mg in the morning and 50–100 mg after the noon or evening meal, depending on response to the morning dose.129 b
Some clinicians recommend a dosage of 50 mg daily for several days and then increasing dosage only if necessary.b
Adjust dosage gradually in increments of 25–50 mg daily to avoid alterations in electrolyte and water excretion.129 b Some patients (usually those with severe, refractory edema) may require up to 200 mg twice daily.129
When added to existing diuretic regimen, initial dose should be 25 mg; increase in increments of 25 mg. b
For maintenance therapy, use smallest effective dose once or twice daily.b May reduce frequency of administration after effective diuresis (dry weight) is achieved (usually with doses of 50–100 mg);129 may administer drug intermittently (e.g., on alternate days or less frequently).129 b
IV
Average size adults: 50 mg or 0.5–1 mg/kg; single IV doses should not exceed 100 mg. 129 Usually only one dose is necessary; if a second dose is needed, use a new injection site to avoid possible thrombophlebitis. 129
Hypertension†
Oral
Initial dosage of 25 mg daily and usual maximum dosage of 100 mg daily (in 2 or 3 divided doses) have been recommended;101 102 103 104 however, other antihypertensive agents are preferred.501 502 503 504 1200 (See Hypertension under Uses.)
Prescribing Limits
Adults
Edema
Oral
Maximum 200 mg twice daily.129
IV
Maximum 100 mg per dose. b
Special Populations
Hepatic Impairment
Initiate therapy in a hospital in cirrhotic patients with ascites. 129
Geriatric Patients
Select dosage with caution because of age-related decreases in renal function.129
Cautions for Ethacrynic Acid
Contraindications
-
Anuria, hypotension, dehydration with low serum sodium concentrations, or metabolic alkalosis with hypokalemia.129 b
-
Increasing azotemia and/or oliguria, electrolyte imbalance, or severe, watery diarrhea that occurs during use.129 b
-
Known hypersensitivity to ethacrynic acid or any ingredient in the formulation.129 b
-
Use in infants.129
Warnings/Precautions
Warnings
Electrolyte, Fluid, and Renal Effects
Excessive diuresis may cause fluid and electrolyte (chloride, calcium, magnesium, sodium) depletion; these effects likely to occur with large doses of the drug, in patients on restricted salt intake,b those with secondary hyperaldosteronism (associated with cirrhosis and nephrosis),b or use of digoxin.b Resultant hypovolemia may result in dehydration, blood volume reduction leading to circulatory collapse and thromboembolic episodes (e.g., cerebral vascular thrombosis, pulmonary emboli [may be fatal]), particularly in geriatric patients.129 b
Fatal arrhythmias associated with hypokalemia reported in patients with severe myocardial disease receiving digitalis.129 Hypokalemia and hypochloremia may result in metabolic alkalosis, especially in patients with other losses of potassium and chloride resulting from vomiting, diarrhea, GI drainage, excessive sweating, paracentesis, or potassium-losing renal diseases.b To reduce or prevent potassium depletion, administer drug intermittently and/or give potassium-rich foods or a potassium-sparing diuretic.b Potassium supplements may be necessary in patients whose serum potassium concentration is less than approximately 3 mEq/L or those receiving digitalis glycosides.b
Risk of orthostatic hypotension or acute hypotensive episodes, especially with brisk diuresis (evidenced by rapid and excessive weight loss) or in patients receiving other antihypertensive agents; monitor BP closely.129 b
Rapid or excessive diuresis may cause an abrupt fall in GFR and renal blood flow.b
Transient rise in BUN may occur, especially in patients with chronic renal disease; usually reversible upon discontinuance. b
If excessive diuresis occurs, discontinue the drug until homeostasis is restored.129
If excessive electrolyte depletion occurs, reduce dosage or withdraw drug temporarily.129
Adequate Patient Evaluation and Monitoring
Monitor serum electrolytes, BUN, and CO2 early in therapy and periodically thereafter; discontinue or reduce dosage if excessive diuresis and/or electrolyte abnormalities occur.129 b Correct electrolyte abnormalities as appropriate.129 b
Observe carefully for manifestations of fluid and electrolyte depletion (e.g., thirst, weakness, lethargy, dizziness, faintness, mental confusion, lassitude, restlessness, muscle pains or cramps, muscular fatigue, headache, paresthesia, anorexia, hypotension, oliguria, arrhythmia, nausea, vomiting).b
Ototoxicity
Tinnitus, vertigo with a sense of fullness in the ears, and temporary (lasting 1–24 hours) or permanent deafness have occurred, usually after IV administration in patients with severe renal impairment or in those concomitantly receiving ototoxic drugs or in those who received ethacrynic acid or ethacrynate sodium doses larger than those recommended.129 (See Specific Drugs under Interactions.)
Sensitivity Reactions
Rash has been reported. 129
General Precautions
Metabolic Effects
Hyperglycemia and alterations in glucose tolerance reported.129
Specific Populations
Pregnancy
Category B.129
Lactation
Not known whether ethacrynic acid is distributed into milk.129 b Discontinue nursing or the drug.129 b
Pediatric Use
Safety and efficacy not established in infants; do not administer to infants until further accumulation of data.129 109 (See Contraindications under Cautions.)
The manufacturer states that dosage recommendations for short-term management of hospitalized pediatric patients (excluding infants) with edema associated with congenital heart disease or nephrotic syndrome are empiric, since no well-controlled studies have been published.109 129
Safety and efficacy of ethacrynate sodium in pediatric patients not established. b
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out. 129 Other reported clinical experience has not identified differences in responses between geriatric and younger patients.129
Assess renal function periodically, since ethacrynic acid is substantially eliminated by kidneys and geriatric patients are more likely to have decreased renal function.129 Select dosage with caution.129
Hepatic Impairment
Manufacturer recommends initiating therapy in a hospital in cirrhotic patients with ascites.129
Administer with caution in patients with advanced cirrhosis, especially those with a history of previous episodes of electrolyte imbalance or hepatic encephalopathy.129
In patients with hepatic cirrhosis, rapid alterations in fluid and electrolyte balance may precipitate hepatic pre-coma or coma.129 Deaths have occurred in patients with severely decompensated hepatic cirrhosis with ascites, with or without encephalopathy as a result of intensification of preexisting electrolyte imbalance.129
Potassium depletion possible; consider supplemental potassium and/or potassium-sparing agents in cirrhotic patients.129
Renal Impairment
When used in the treatment of renal edema, hypoproteinemia may reduce responsiveness to ethacrynic acid and the use of albumin human should be considered.129 b
Potassium depletion possible; consider supplemental potassium and/or potassium-sparing agents in nephrotic patients. 129
Common Adverse Effects
Anorexia, malaise, abdominal pain/discomfort, dysphagia, nausea, vomiting, diarrhea, reversible hyperuricemia, hyperglycemia, acute gout, deafness, tinnitus, vertigo, headache, fatigue, apprehension, confusion, rash, fever, chills, hematuria; local irritation and pain has been occasionally reported after IV use. 129
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Alcohol |
May augment effects of alcoholb |
|
|
Antidiabetic agents (e.g., insulin, oral agents) |
Possible antagonism of hypoglycemic effect as result of hypokalemiab |
Observe for possible decreased diabetic control; correct potassium deficit and/or adjust dosage of antidiabetic agentb |
|
Antihypertensive agents |
Additive antihypertensive effect; orthostatic hypotension may occurb |
Reduce dosage of both drugsb |
|
Carbonic anhydrase inhibitors (e.g., acetazolamide, dichlorphenamide, methazolamide) |
May potentiate action of carbonic anhydrase inhibitors; augmentation of natriuresis and kaliuresis129 |
Cautiously dose ethacrynic acid 129 |
|
Cardiac glycosides (e.g., digoxin) |
Possible electrolyte disturbances (e.g., hypokalemia, hypomagnesemia), increased risk of cardiac glycoside toxicity and/or fatal cardiac arrhythmiasb |
Periodically monitor electrolytes; correct hypokalemiab |
|
Corticosteroids |
Possible increased risk of gastric hemorrhage associated with corticosteroids129 (See also Drugs that Cause Potassium Loss) |
|
|
Diuretics |
Reduce ethacrynic acid dosage when it is added to an existing diuretic regimenb |
|
|
Diuretics, loop (e.g., bumetanide, furosemide, torsemide) |
Share similar mechanisms of actionb |
No therapeutic rationale for concomitant useb |
|
Diuretics, potassium-sparing (e.g., amiloride, spironolactone, triamterene) |
Possible reduction in potassium loss129 |
May be used for therapeutic advantage129 |
|
Diuretics, thiazides |
Additive diuretic effectb |
Use reduced dosage of ethacrynic acid when added to existing diuretic regimenb |
|
Drugs that cause potassium loss (e.g., corticosteroids, corticotropin, amphotericin B) |
Additive hypokalemic effectsb |
Monitor electrolytes; correct hypokalemiab |
|
Lithium |
Reduced renal clearance of lithium and increased risk of lithium toxicity129 b |
Avoid concomitant use; if concomitant therapy is necessary, hospitalize patient and monitor for lithium toxicity129 b |
|
Neuromuscular blocking agents, nondepolarizing (e.g., tubocurarine chloride) |
Potential for prolonged neuromuscular blockade, associated with potassium depletionb |
|
|
NSAIAs |
Possible decreased diuretic, natriuretic, and antihypertensive effects108 119 129 b Increased risk of developing renal failure associated with decreased renal blood flow, resulting from prostaglandin inhibition by NSAIAs117 118 |
Monitor closely for desired diuretic effect129 |
|
Ototoxic drugs (e.g., aminoglycosides, some cephalosporins) |
Possible additive ototoxic effect (transient or permanent deafness), especially with IV ethacrynate sodium 129 b |
|
|
Uricosuric drugs (probenecid, sulfinpyrazone) |
Urinary excretion and efficacy of ethacrynic acid may decrease.b Possible antagonism of uricosuric effectsb |
Monitor serum uric acid concentrations; dosage of uricosuric agents may need to be increasedb |
|
Warfarin |
Possible potentiation of anticoagulant effect (because of displacement of warfarin from protein-binding sites)129 b |
Ethacrynic Acid Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from the GI tract.b
Onset
Following oral administration, diuretic effect occurs within 30 minutes and peaks in about 2 hours.129 b
Following IV administration of ethacrynate sodium, diuresis usually occurs within 5 minutes and reaches a maximum within 15–30 minutes.129 b
Duration
Diuretic effect persists 6–8 hours (up to 12 hours) following oral administration, and about 2 hours following IV administration of ethacrynate sodium.129 b
Distribution
Extent
In animals, substantial amounts accumulate only in the liver.b
Not known whether ethacrynic acid crosses the placentab or is distributed into human milk.129 b
Elimination
Metabolism
Metabolized to a cysteine conjugate (which may contribute to the pharmacologic effects of the drug) and to an unstable, unidentified compound.b
Elimination Route
IV Ethacrynate sodium: Excreted in urine (about 30–65%) and in bile (about 35–40%); partially as the cysteine conjugate.b
Rate of urinary excretion increases as urinary pH increases. b
Stability
Storage
Oral
Tablets
Tight containers at 25°C (may be exposed to 15–30°C).120 129
Parenteral
Powder for Injection
25°C (may be exposed to 15–30°C).120 129
Use reconstituted solutions within 24 hours of preparation.129 b
Reconstituted solutions stable for short periods of time at pH 7 at room temperature; less stable as pH and/or temperature increase.b Some 5% dextrose solutions have pH <5, which may result in a hazy or opalescent solution that should not be used.129
Compatibility
Parenteral
Solution Compatibilityb
|
Compatible |
|---|
|
Dextrose 5% in water |
|
Dextrose 5% in sodium chloride 0.9% |
|
Ringer’s injection |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.9% |
|
Incompatible |
|
Normosol-M |
Drug CompatibilityHID
|
Compatible |
|---|
|
Chlorpromazine HCl |
|
Prochlorperazine edisylate |
|
Incompatible |
|
Hydralazine HCl |
|
Procainamide HCl |
|
Ranitidine HCl |
|
Compatible |
|---|
|
Heparin sodium with hydrocortisone sodium succinate |
|
Potassium chloride |
|
Incompatible |
|
Nesiritide |
Actions
-
In vitro, inhibits active transport of chloride in the lumen of the ascending limb of the loop of Henle and thereby, diminishes reabsorption of sodium and chloride at that site.b
-
Increases potassium excretion in the distal renal tubule, and exerts a direct effect on electrolyte transport at the proximal tubule. b
-
Does not inhibit carbonic anhydrase and is not an aldosterone antagonist.b Aldosterone secretion may increase during therapy and may contribute to hypokalemia.b
-
Enhances excretion of sodium, chloride, potassium, hydrogen, calcium, and magnesium.b
-
Initially, sodium and chloride excretion is substantial, and chloride loss exceeds that of sodium.129
-
With prolonged administration, sodium and chloride excretion declines, and excretion of potassium and hydrogen may increase.129 b Excessive losses of potassium, hydrogen, and chloride may result in metabolic alkalosis.
-
Maximum diuresis and electrolyte loss are greater with ethacrynic acid than with the thiazides or most other diuretics except furosemide.b
-
Has little or no direct effect on GFR or renal blood flow; however, a fall in GFR may accompany pronounced reductions in plasma volume associated with rapid or excessive diuresis.129
-
A hypotensive effect may result from decreased plasma volume.b
Advice to Patients
-
Importance of reporting manifestations of fluid and electrolyte depletion (e.g., dryness of mouth, thirst, weakness, dizziness, faintness, mental confusion, lassitude, lethargy, drowsiness, restlessness, muscle pains or cramps, paresthesia, muscular fatigue, hypotension, headache, oliguria, tachycardia, arrhythmia, anorexia, nausea, vomiting).129 b
-
Importance of discussing dietary measures and supplementation to prevent or correct hypokalemia.b
-
Importance of informing patients with diabetes mellitus that blood glucose and urine glucose concentrations may increase.b
-
Importance of immediately reporting severe diarrhea.b
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs as well as any concomitant illnesses.129
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.129
-
Importance of informing patients of other important precautionary information.129 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
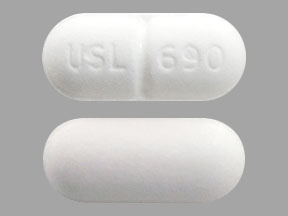
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
25 mg |
Edecrin (scored) |
Aton Pharma |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection, for IV use only |
equivalent to ethacrynic acid 50 mg |
Sodium Edecrin |
Aton Pharma |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
Only references cited for selected revisions after 1984 are available electronically.
100. Fischer AF, Parker BR, Stevenson DK. Nephrolithiasis following in utero diuretic exposure: an unusual case. Pediatrics. 1988; 81:712-4. https://pubmed.ncbi.nlm.nih.gov/3282218
101. The Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The 1984 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1984; 144:1045-57. https://pubmed.ncbi.nlm.nih.gov/6143542
102. 1988 Joint National Committee. The 1988 report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1988; 148:1023-38. https://pubmed.ncbi.nlm.nih.gov/3365073
103. Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993; 153:154-83. https://pubmed.ncbi.nlm.nih.gov/8422206
104. National Heart, Lung, and Blood Institute National High Blood Pressure Education Program. The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). Bethesda, MD: National Institutes of Health. (NIH publication No. 98-4080.)
105. Kaplan NM. Choice of initial therapy for hypertension. JAMA. 1996; 275:1577-80. https://pubmed.ncbi.nlm.nih.gov/8622249
106. Psaty BM, Smith NL, Siscovich DS et al. Health outcomes associated with antihypertensive therapies used as first-line agents: a systematic review and meta-analysis. JAMA. 1997; 277:739-45. https://pubmed.ncbi.nlm.nih.gov/9042847
107. Whelton PK, Appel LJ, Espeland MA et al. for the TONE Collaborative Research Group. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). JAMA. 1998; 279:839-46. https://pubmed.ncbi.nlm.nih.gov/9515998
108. Anon. Consensus recommendations for the management of chronic heart failure. On behalf of the membership of the advisory council to improve outcomes nationwide in heart failure. Part II. Management of heart failure: approaches to the prevention of heart failure. Am J Cardiol. 1999; 83:9A-38A.
109. Merck. Edecrin (ethacrynic acid) tablets and Intravenous Sodium Edecrin (ethacrynate sodium) prescribing information (dated 1997 Jun). In: Physicians’ desk reference. 53rd ed. Montvale, NJ: Medical Economics Company Inc; 1999:1790-1.
110. Leary WP, Reyes AJ. Drug interactions with diuretics. S Afr Med J. 1984; 65:455-61. https://pubmed.ncbi.nlm.nih.gov/6701709
111. The Captopril-Digoxin Multicenter Research Group. Comparative effects of therapy with captopril and digoxin in patients with mild to moderate heart failure. JAMA. 1988; 259:539-44. https://pubmed.ncbi.nlm.nih.gov/2447297
112. Richardson A, Bayliss J, Scriven AJ et al. Double-blind comparison of captopril alone against frusemide plus amiloride in mild heart failure. Lancet. 1987; 2:709-11. https://pubmed.ncbi.nlm.nih.gov/2888942
113. Sherman LG, Liang CS, Baumgardner S et al. Piretanide, a potent diuretic with potassium-sparing properties, for the treatment of congestive heart failure. Clin Pharmacol Ther. 1986; 40:587-94. https://pubmed.ncbi.nlm.nih.gov/3533372
114. Patterson JH, Adams KF Jr, Applefeld MM et al. Oral torsemide in patients with chronic congestive heart failure: effects on body weight, edema, and electrolyte excretion. Pharmacotherapy. 1994; 14:514-21. https://pubmed.ncbi.nlm.nih.gov/7997385
115. Wilson JR, Reichek N, Dunkman WB et al. Effect of diuresis on the performance of the failing left ventricle in man. Am J Med. 1981;70:234-9.
116. Parker JO. The effects of oral ibopamine in patients with mild heart failure—a double blind placebo controlled comparison to furosemide. Int J Cardiol. 1993; 40:221-7. https://pubmed.ncbi.nlm.nih.gov/8225657
117. Hansten PD, Horn JR. Diuretics and non-steroidal anti-inflammatory drugs. Drug Interact Newsl. 1986; 6:27-9.
118. O’Brien WM. Pharmacology of nonsteroidal anti-inflammatory drugs: practical review for clinicians. Am. J Med. 1983; 10:32-9.
119. Brater DC. Drug-drug and drug-disease interactions with nonsteroidal anti-inflammatory drugs. Am J Med. 1986; 80(Suppl 1A):62-77. https://pubmed.ncbi.nlm.nih.gov/3511686
120. Edecrin (ethacrynic acid and ethacrynate sodium) tablets and injection. In: MedWatch: summary of safety-related drug labeling changes approved by FDA. Rockville, MD: US Food and Drug Administration; 1999 Oct.
121. The United States pharmacopeia, 24th rev, and The national formulary, 19th ed. Rockville, MD: The United States Pharmacopeial Convention, Inc; 2000:689.
122. Izzo JL, Levy D, Black HR. Importance of systolic blood pressure in older Americans. Hypertension. 2000; 35:1021-4. https://pubmed.ncbi.nlm.nih.gov/10818056
123. Frohlich ED. Recognition of systolic hypertension for hypertension. Hypertension. 2000; 35:1019-20. https://pubmed.ncbi.nlm.nih.gov/10818055
124. Bakris GL, Williams M, Dworkin L et al. Preserving renal function in adults with hypertension and diabetes: a consensus approach. Am J Kidney Dis. 2000; 36:646-61. https://pubmed.ncbi.nlm.nih.gov/10977801
125. Associated Press (American Diabetes Association). Diabetics urged: drop blood pressure. Chicago, IL; 2000 Aug 29. Press Release from web site. http://www.diabetes.org/newsroom/
128. The Guidelines Subcommittee of the WHO/ISH Mild Hypertension Liaison Committee. 1999 guidelines for the management of hypertension. J Hypertension. 1999; 17:392-403.
129. Aton Pharma, Inc. Edecrin and Sodium Edecrin (ethacrynic acid and ethacrynate sodium) tablets and injection prescribing information. Lawrenceville, NJ; 2007 Oct. Accessed 2/27/08. http://www.atonrx.com/prescribing_information/Edecrin_PI.pdf
130. Slim HB, Black HR, Thompson PD. Older blood pressure medications-do they still have a place?. Am J Cardiol. 2011; 108:308-16. https://pubmed.ncbi.nlm.nih.gov/21550576
501. James PA, Oparil S, Carter BL et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507-20. https://pubmed.ncbi.nlm.nih.gov/24352797
502. Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013; 31:1281-357. https://pubmed.ncbi.nlm.nih.gov/23817082
503. Go AS, Bauman MA, Coleman King SM et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014; 63:878-85. https://pubmed.ncbi.nlm.nih.gov/24243703
504. Weber MA, Schiffrin EL, White WB et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014; 16:14-26. https://pubmed.ncbi.nlm.nih.gov/24341872
524. WRITING COMMITTEE MEMBERS, Yancy CW, Jessup M et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128:e240-327.
700. Yancy CW, Jessup M, Bozkurt B et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2016; :.
713. Gupta D, Georgiopoulou VV, Kalogeropoulos AP et al. Dietary sodium intake in heart failure. Circulation. 2012; 126:479-85. https://pubmed.ncbi.nlm.nih.gov/22825409
714. Hospira. Dopamine hydrochloride prescribing information. Lake Forest, IL; 2014 Mar.
715. Hospira. Dopamine hydrochloride and 5% dextrose injection prescribing information. Lake Forest, IL; 2014 May.
716. Cicci JD, Reed BN, McNeely EB et al. Acute decompensated heart failure: evolving literature and implications for future practice. Pharmacotherapy. 2014; 34:373-88. https://pubmed.ncbi.nlm.nih.gov/24214219
717. Triposkiadis FK, Butler J, Karayannis G et al. Efficacy and safety of high dose versus low dose furosemide with or without dopamine infusion: the Dopamine in Acute Decompensated Heart Failure II (DAD-HF II) trial. Int J Cardiol. 2014;172(1):115-21.
718. Torres-Courchoud I, Chen HH. Is there still a role for low-dose dopamine use in acute heart failure?. Curr Opin Crit Care. 2014; 20:467-71. https://pubmed.ncbi.nlm.nih.gov/25137402
719. Houston BA, Kalathiya RJ, Kim DA et al. Volume Overload in Heart Failure: An Evidence-Based Review of Strategies for Treatment and Prevention. Mayo Clin Proc. 2015; 90:1247-61. https://pubmed.ncbi.nlm.nih.gov/26189443
720. Chen HH, Anstrom KJ, Givertz MM et al. Low-dose dopamine or low-dose nesiritide in acute heart failure with renal dysfunction: the ROSE acute heart failure randomized trial. JAMA. 2013; 310:2533-43. https://pubmed.ncbi.nlm.nih.gov/24247300 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3934929/
723. Hummel SL, Konerman MC. Dietary Sodium Restriction in Heart Failure: A Recommendation Worth its Salt?. JACC Heart Fail. 2016; 4:36-8. https://pubmed.ncbi.nlm.nih.gov/26738950
724. Yancy CW. The Uncertainty of Sodium Restriction in Heart Failure: We Can Do Better Than This. JACC Heart Fail. 2016; 4:39-41. https://pubmed.ncbi.nlm.nih.gov/26738951
1200. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:el13-e115. https://pubmed.ncbi.nlm.nih.gov/29133356
b. AHFS Drug Information. McEvoy GK, ed. Ethacrynic Acid, Ethacrynate Sodium. Bethesda, MD: American Society of Health-System Pharmacists; 2017:.
HID. Trissel LA. Handbook on injectable drugs. 17th ed. Bethesda, MD: American Society of Health-System Pharmacists, Inc; 2013:463-4.
Related/similar drugs
More about ethacrynic acid
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: loop diuretics
- Breastfeeding
- En español
Patient resources
- Ethacrynic acid drug information
- Ethacrynate sodium (Advanced Reading)
- Ethacrynic acid (Advanced Reading)
Professional resources
- Ethacrynate Sodium Injection prescribing information
- Ethacrynic Acid (FDA)
- Ethacrynic Sodium Injection (FDA)