Elexacaftor, Tezacaftor, And Ivacaftor (Monograph)
Brand name: Trikafta
Drug class: Cystic Fibrosis Transmembrane Conductance Regulator Correctors
Warning
- Drug-induced Liver Injury and Liver Failure
-
Can cause serious and potentially fatal drug-induced liver injury.
-
Assess liver function tests (ALT, AST, alkaline phosphatase, bilirubin) prior to initiating therapy.
-
Monitor liver function tests every month for initial 6 months of treatment, then every 3 months for next 12 months, and at least annually thereafter. Interrupt therapy for significant elevations in liver function tests or signs/symptoms of liver toxicity.
-
Follow patients closely until abnormalities resolve and resume therapy only if benefit outweighs risk.
-
Do not use in patients with severe hepatic impairment (Child-Pugh Class C). Not recommended in patients with moderate hepatic impairment (Child-Pugh Class B).
Introduction
Fixed combination containing elexacaftor and tezacaftor (cystic fibrosis transmembrane conductance regulator [CFTR] correctors) and ivacaftor (CFTR potentiator).
Uses for Elexacaftor, Tezacaftor, And Ivacaftor
Cystic Fibrosis
Elexacaftor/tezacaftor/ivacaftor combination therapy: Treatment of cystic fibrosis in patients ≥2 years of age who have at least one F508del mutation in the CFTR gene or a mutation in the CFTR gene that is responsive to the combination drug regimen based on clinical and/or in vitro data.
Designated an orphan drug by FDA for this use.
If patient's genotype unknown, use FDA-approved cystic fibrosis mutation test to confirm presence of at least one indicated mutation. Refer to the prescribing information for a list of CFTR gene mutations responsive to therapy.
There are several approved therapies for specific subpopulations of cystic fibrosis patients; however, the treatment effect in some mutations (e.g. homozygous F508del) are modest. Elexacaftor/tezacaftor/ivacaftor provides a therapeutic option for patients with mutations not covered by other approved CFTR modulators.
The 2018 Cystic Fibrosis Foundation pulmonary guideline specifically addresses the use of CFTR modulators in patients with cystic fibrosis. Elexacaftor/tezacaftor/ivacaftor was approved after publication of the guideline, and therefore is not addressed.
Elexacaftor, Tezacaftor, And Ivacaftor Dosage and Administration
General
Pretreatment Screening
-
Obtain a baseline ophthalmologic examination in pediatric patients.
-
Obtain liver function tests (ALT, AST, alkaline phosphatase, bilirubin) prior to initiation of therapy.
Patient Monitoring
-
Perform follow-up ophthalmologic examinations in pediatric patients.
-
Monitor liver function tests every month during the initial 6 months of therapy, then every 3 months for the next 12 months, and then at least annually thereafter. Consider monitoring more frequently in patients with a history of liver disease or liver function test elevations at baseline.
Administration
Oral Administration
Administer orally as tablets or oral granules.
Administer tablets or oral granules with fat-containing food (e.g., eggs, cheese, nuts, peanut butter, whole milk, meats, food prepared with butter or oils) to increase systemic absorption of the drug.
Tablets: Swallow tablets whole.
Oral granules: Administer immediately before or after ingestion of fat-containing food. Mix entire contents of each packet of oral granules with one teaspoon (5 mL) of age-appropriate soft food or liquid such as pureed fruits or vegetables, yogurt, applesauce, water, milk, or juice that is at or below room temperature. Once mixed, the product should be consumed completely within 1 hour.
Combination therapy consists of a morning dose of the fixed-combination of elexacaftor/tezacaftor/ivacaftor and an evening dose of single-entity ivacaftor; take morning and evening doses approximately 12 hours apart.
If a dose of elexacaftor/tezacaftor/ivacaftor combination therapy is missed by ≤6 hours, the dose should be taken as soon as it is remembered and the original dosing schedule should be resumed.
If a morning dose is missed by >6 hours, the dose should be taken as soon as possible and the evening dose of single-entity ivacaftor should be omitted; the morning fixed-combination dose on the following day should be taken at the regularly scheduled time.
If an evening dose of single-entity ivacaftor is missed by >6 hours, the evening dose should be omitted and the next morning fixed-combination dose should be taken at the regularly scheduled time.
Do not take the morning and evening doses at the same time.
Dosage
Pediatric Patients
Cystic Fibrosis
Oral
Children 2 to <6 years of age: Recommended dosage is weight-based. For patients <14 kg, the recommended dosage is one packet (as oral granules containing elexacaftor 80 mg/tezacaftor 40 mg/ivacaftor 60 mg) once daily in the morning and one packet (as oral granules containing ivacaftor 59.5 mg) once daily in the evening, approximately 12 hours apart with fat-containing food. For those ≥14 kg, the recommended dosage is one packet (as oral granules containing elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75mg) once daily in the morning and one packet (as oral granules containing ivacaftor 75 mg) once daily in the evening, approximately 12 hours apart with fat-containing food.
Children 6 to <12 years of age: Recommended dosage is weight-based. For patients <30 kg, recommended dosage is elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg (administered as 2 fixed-combination tablets each containing elexacaftor 50 mg, tezacaftor 25 mg, and ivacaftor 37.5 mg) once daily in the morning and ivacaftor 75 mg (administered as a single-entity tablet) once daily in the evening approximately 12 hours apart. For patients ≥30 kg, recommended dosage is the same for children ≥12 years of age and adults.
Children ≥12 years of age: Elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg (administered as 2 fixed-combination tablets each containing elexacaftor 100 mg, tezacaftor 50 mg, and ivacaftor 75 mg) once daily in the morning and ivacaftor 150 mg (administered as a single-entity tablet) once daily in the evening approximately 12 hours apart.
Adults
Cystic Fibrosis
Oral
Elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg (administered as 2 fixed-combination tablets each containing elexacaftor 100 mg, tezacaftor 50 mg, and ivacaftor 75 mg) once daily in the morning and ivacaftor 150 mg (administered as a single-entity tablet) once daily in the evening approximately 12 hours apart.
Dosage Modification for Patients Taking CYP3A Inhibitors
Dosage adjustment necessary when co-administered with strong (e.g., ketoconazole, itraconazole, posaconazole, voriconazole, and clarithromycin) or moderate (e.g.,fluconazole, erythromycin) CYP3A inhibitors (see Table 1).
|
Age |
Weight |
Moderate CYP3A Inhibitors |
Strong CYP3A Inhibitors |
|---|---|---|---|
|
2 to <6 years of age |
<14 kg |
Alternating daily dosing schedule is as follows: Day 1: One packet (containing elexacaftor 80 mg/tezacaftor 40 mg/ivacaftor 60 mg) in the morning Day 2: One packet (containing ivacaftor 59.5 mg) oral granules in the morning No evening packet of ivacaftor oral granules. |
One packet (containing elexacaftor 80 mg/tezacaftor 40 mg/ivacaftor 60 mg) in the morning twice a week, approximately 3 to 4 days apart. No evening packet of ivacaftor oral granules. |
|
2 to <6 years of age |
≥14 kg |
Alternating daily dosing schedule is as follows: Day 1: One packet (containing elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg) in the morning Day 2: One packet (containing ivacaftor 75 mg) oral granules in the morning No evening packet of ivacaftor oral granules. |
One packet (containing elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg) in the morning twice a week, approximately 3 to 4 days apart. No evening packet of ivacaftor oral granules. |
|
≥6 years of age |
<30 kg |
Alternating daily dosing schedule is as follows: Day 1: Two tablets of elexacaftor 50 mg/tezacaftor 25 mg/ivacaftor 37.5 mg (total dose of elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg) in the morning Day 2: One tablet of ivacaftor 75 mg in the morning No evening ivacaftor tablet dose. |
Two tablets of elexacaftor 50 mg/tezacaftor 25 mg/ivacaftor 37.5 mg (total dose of elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg) in the morning twice a week, approximately 3 to 4 days apart. No evening ivacaftor tablet dose. |
|
≥6 years of age |
≥30 kg |
Alternating daily dosing schedule is as follows: Day 1: Two tablets elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg (total dose of elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg) in the morning Day 2: One tablet of ivacaftor 150 mg in the morning No evening ivacaftor tablet dose. |
Two tablets elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg (total dose of elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg) in the morning twice a week, approximately 3 to 4 days apart. No evening ivacaftor tablet dose. |
|
≥12 years of age |
Alternating daily dosing schedule is as follows: Day 1: Two tablets elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg (total dose of elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg) in the morning Day 2: One tablet of ivacaftor 150 mg in the morning No evening ivacaftor tablet dose. |
Two tablets elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg (total dose of elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg) in the morning twice a week, approximately 3 to 4 days apart. No evening ivacaftor tablet dose. |
Special Populations
Hepatic Impairment
Mild hepatic impairment (Child-Pugh class A): Dosage adjustment not necessary.
Moderate hepatic impairment (Child-Pugh class B): Use with caution at a reduced dosage (see Table 2).
|
Age |
Weight |
Morning Dose |
Evening Dose |
|---|---|---|---|
|
2 to <6 years of age |
<14 kg |
Weekly dosing schedule as follows: Days 1-3: One packet (containing elexacaftor 80 mg/tezacaftor 40 mg/ivacaftor 60 mg) oral granules each day Day 4: no dose Days 5-6: One packet (containing elexacaftor 80 mg/tezacaftor 40 mg/ivacaftor 60 mg) oral granules each day Day 7: no dose |
No evening dose of ivacaftor oral granules |
|
2 to <6 years of age |
≥14 kg |
Weekly dosing schedule as follows: Days 1-3: One packet (containing elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg) oral granules each day Day 4: no dose Days 5-6: One packet (containing elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg) oral granules each day Day 7: no dose |
No evening dose of ivacaftor oral granules |
|
6 to <12 years of age |
<30 kg |
Alternating daily dosing schedule as follows: Day 1: Two tablets of elexacaftor 50 mg/tezacaftor 25 mg/ivacaftor 37.5 mg (total dose of elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg) Day 2: One tablet of elexacaftor 50 mg/tezacaftor 25 mg/ivacaftor 37.5 mg |
No evening ivacaftor tablet dose |
|
6 to <12 years of age |
≥30 kg |
Alternating daily dosing schedule as follows: Day 1: Two tablets of elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg (total dose of elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg) Day 2: One tablet elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg |
No evening ivacaftor tablet dose |
|
≥12 years of age |
Alternating daily dosing schedule as follows: Day 1: Two tablets of elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg (total dose of elexacaftor 200 mg/tezacaftor 100 mg/ivacaftor 150 mg) Day 2: One tablet elexacaftor 100 mg/tezacaftor 50 mg/ivacaftor 75 mg |
No evening ivacaftor tablet dose |
Severe hepatic impairment (Child-Pugh class C): Use not recommended.
Renal Impairment
Mild to moderate renal impairment: Dosage adjustment not necessary.
Severe renal impairment (eGFR <30 mL/minute per 1.73 m2) or end-stage renal disease (ESRD): Caution advised.
Geriatric Patients
No specific dosage recommendations.
Cautions for Elexacaftor, Tezacaftor, And Ivacaftor
Contraindications
-
None.
Warnings/Precautions
Warnings
Drug-Induced Liver Injury and Liver Failure
Elexacaftor/tezacaftor/ivacaftor associated with serious and potentially fatal drug-induced liver injury (see Boxed Warning). Cases of liver failure leading to transplantation and death reported in patients administered elexacaftor/tezacaftor/ivacaftor with and without a history of liver disease. Liver injury has occurred within the initial month of therapy and up to 15 months following treatment initiation. In all patients, assess liver function tests (ALT, AST, alkaline phosphatase, and bilirubin) prior to treatment initiation. Subsequently, monitor liver function tests every month during the initial 6 months of treatment, then every 3 months for the next 12 months, and at least annually thereafter. Consider more frequent monitoring in patients with a history of liver disease or liver function test elevations at baseline. Interrupt therapy if clinical symptoms of liver injury (e.g., jaundice, right upper quadrant pain, nausea, vomiting, altered mental status, ascites) and/or significant elevations in liver function tests (e.g., ALT or AST >5 times the upper limit of normal [ULN] or ALT or AST >3 times ULN with bilirubin >2 times ULN) are present. Consider referral to a hepatologist for patients with clinical and laboratory abnormalities suggestive of liver dysfunction and follow closely until abnormalities resolve. Upon resolution of abnormalities, and if the benefit of therapy outweighs the risk, resume therapy with close monitoring. Do not administer elexacaftor/tezacaftor/ivacaftor in patients with severe hepatic impairment (Child-Pugh Class C). Not recommended in patients with moderate hepatic impairment (Child-Pugh Class B). For these patients, consider therapy only if benefit outweighs risk; if used, administer a reduced dosage and monitor closely.
Other Warnings/Precautions
Hypersensitivity Reactions
Hypersensitivity reactions, including cases of angioedema and anaphylaxis, reported.
Discontinue if signs or symptoms of serious hypersensitivity reactions develop during treatment and institute appropriate therapy. Consider benefits and risks for the individual patient to determine whether to resume treatment.
Interactions with CYP3A Inducers
Concomitant use of elexacaftor/tezacaftor/ivacaftor and potent CYP3A inducers (e.g., rifampin, rifabutin, phenobarbital, carbamazepine, phenytoin, St. John's wort [Hypericum perforatum]) substantially decreases systemic exposure of ivacaftor and may decrease exposure of elexacaftor and tezacaftor; decreased exposures may reduce therapeutic efficacy. Concomitant use with potent CYP3A inducers not recommended.
Interactions with CYP3A Inhibitors
Concomitant use of elexacaftor/tezacaftor/ivacaftor and strong or moderate CYP3A inhibitors (e.g., ketoconazole, itraconazole, posaconazole, voriconazole, clarithromycin, fluconazole, erythromycin) increases systemic exposure of elexacaftor, tezacaftor, and ivacaftor. Reduce dosage of elexacaftor/tezacaftor/ivacaftor when used concomitantly with moderate or strong CYP3A inhibitors.
Cataracts
Ocular lens opacities (not congenital in nature) reported in pediatric patients receiving ivacaftor-containing drug regimens. Although other risk factors were present in some cases (e.g., corticosteroid use, radiation exposure), possible risk attributable to ivacaftor therapy cannot be excluded. Baseline and follow-up ophthalmologic examinations recommended in pediatric patients.
Specific Populations
Pregnancy
Limited data available regarding use of elexacaftor/tezacaftor/ivacaftor combination therapy or its individual components in pregnant women. Evidence of teratogenicity or adverse effects on fetal development not observed in animals receiving elexacaftor, tezacaftor, or ivacaftor. No animal data available with concomitant use of elexacaftor, tezacaftor, and ivacaftor. Placental transfer of individual components observed in animals.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Consider developmental and health benefits of breast-feeding and clinical importance of therapy to the woman when deciding whether to use caution or discontinue nursing. Effects of elexacaftor/tezacaftor/ivacaftor on nursing infants or milk production unknown.
Pediatric Use
Safety and efficacy not established in pediatric patients <2 years of age.
Geriatric Use
Clinical trials did not include any patients ≥65 years of age.
Hepatic Impairment
Mild hepatic impairment (Child-Pugh class A): Dosage adjustment not necessary. Monitor liver function tests closely.
Moderate hepatic impairment (Child-Pugh class B): Increased exposure; use with caution and at reduced dosage after weighing risks and benefits of therapy. Monitor liver function tests closely. In a clinical study of 11 subjects with moderate hepatic impairment (Child-Pugh class B), one subject developed total and direct bilirubin elevations >2 times the ULN and one subject developed direct bilirubin elevation >4.5 times the ULN.
Severe hepatic impairment (Child-Pugh class C): Effect on pharmacokinetics not studied, but increased exposure expected. Use not recommended.
Renal Impairment
Mild or moderate renal impairment: Dosage adjustment not necessary.
Severe renal impairment (eGFR <30 mL/minute per 1.73 m2) or ESRD: Use with caution.
Severe Lung Dysfunction
Safety and efficacy in 18 patients with baseline FEV1 <40% of predicted receiving elexacaftor/tezacaftor/ivacaftor combination therapy in one of the principal efficacy studies was comparable to overall study population.
Common Adverse Effects
Adverse effects occurring in ≥5% of patients: Headache, upper respiratory tract infection, abdominal pain, diarrhea, rash, increased ALT concentrations, nasal congestion, increased CK concentrations, increased AST concentrations, rhinorrhea, rhinitis, influenza, sinusitis, increased bilirubin concentrations.
Drug Interactions
Elexacaftor is a substrate of CYP3A isoenzymes (e.g., CYP3A4, 3A5) and P-glycoprotein (P-gp) transport. In vitro, elexacaftor has shown low potential to inhibit CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP3A4, and P-gp. In vitro, elexacaftor and its M23 metabolite inhibit the uptake of organic anion transporting polypeptide (OATP) 1B1 and 1B3.
Tezacaftor is a substrate of CYP3A isoenzymes (e.g., CYP3A4, 3A5), P-gp transport, breast cancer resistance protein (BCRP), and OATP1B1. In vitro, tezacaftor has shown low potential to inhibit CYP1A2, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP3A4, P-gp, BCRP, organic cation transporter (OCT) 2, organic anion transporter (OAT) 1, and OAT3.
Ivacaftor is a sensitive substrate of CYP3A (e.g., CYP3A4, 3A5). In vitro, ivacaftor has shown potential to inhibit CYP3A and P-gp, and also may inhibit CYP2C8 and CYP2C9.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Strong CYP3A inhibitors (e.g., clarithromycin, itraconazole, ketoconazole, posaconazole, voriconazole): Possible increased elexacaftor, tezacaftor, and ivacaftor exposures. Reduced dosage recommended.
Moderate CYP3A inhibitors (e.g., fluconazole, erythromycin): Possible increased elexacaftor, tezacaftor, and ivacaftor exposures. Reduced dosage recommended.
Strong CYP3A inducers: Possible decreased ivacaftor exposure; decreased elexacaftor and tezacaftor exposure expected. Concomitant use not recommended.
Drugs Affected by P-glycoprotein Transport
P-gp substrates: Possible increased exposure, prolonged therapeutic effect, or increased risk of adverse effects of the substrate drug. Use P-gp substrates with narrow therapeutic index concomitantly with caution; monitor patients appropriately.
Drugs Affected by Organic Anion-transporting Polypeptide 1B1 and 1B3
Substrates of OATP1B1 and 1B3: Possible increased exposure, prolonged therapeutic effect, or increased risk of adverse effects of the substrate drug. Use substrates of these transporters concomitantly with caution; monitor patients appropriately.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin) |
Possible decreased elexacaftor, tezacaftor, and ivacaftor exposures and reduced efficacy of elexacaftor/tezacaftor/ivacaftor |
Concomitant use not recommended |
|
Antidiabetic agents, sulfonylureas (glimepiride, glipizide, glyburide, nateglinide, repaglinide) |
Possible increased exposures of glimepiride, glipizide, glyburide, nateglinide, repaglinide |
Use concomitantly with caution and monitor patients appropriately |
|
Antifungals, azoles (fluconazole, itraconazole, ketoconazole, posaconazole, voriconazole) |
Itraconazole: Concomitant use with tezacaftor/ivacaftor results in 4- and 15.6-fold increased tezacaftor and ivacaftor AUCs, respectively; concomitant use with single doses of elexacaftor and tezacaftor increased AUCs of elexacaftor and tezacaftor by 2.8- and 4- to 4.5-fold, respectively Ketoconazole: Concomitant use with a single 150-mg dose of ivacaftor results in 8.5-fold increased AUC of ivacaftor Fluconazole: Concomitant use with ivacaftor results in 2.9-fold increased AUC of ivacaftor; concomitant use with elexacaftor and tezacaftor may increase AUCs of elexacaftor and tezacaftor by 1.9- to 2.3- and 2.1-fold, respectively |
Itraconazole, ketoconazole, posaconazole, voriconazole: Reduced dosage of elexacaftor/tezacaftor/ivacaftor recommended |
|
Anti-infective agents, macrolides (clarithromycin, erythromycin) |
Possible increased elexacaftor, tezacaftor, and ivacaftor exposures |
Clarithromycin, erythromycin: Reduced dosage of elexacaftor/tezacaftor/ivacaftor recommended |
|
Antilipemic agents, hydroxymethylglutaryl-CoA (HMG-CoA) reductase inhibitors (i.e., statins) |
Possible increased statin exposure |
Use concomitantly with caution and monitor patients appropriately |
|
Antimycobacterials (rifabutin, rifampin) |
Rifabutin: Possible decreased elexacaftor, tezacaftor, and ivacaftor exposures and reduced efficacy of elexacaftor/tezacaftor/ivacaftor Rifampin: Decreased ivacaftor exposure by 89%, and decreased elexacaftor and tezacaftor exposure also expected; possible reduced efficacy of elexacaftor/tezacaftor/ivacaftor |
Concomitant use not recommended |
|
Ciprofloxacin |
No clinically important effect on elexacaftor, tezacaftor, or ivacaftor exposures expected |
Dosage adjustment not needed |
|
Digoxin |
Increased digoxin exposure; possible prolonged therapeutic effect of digoxin or increased risk of digoxin-associated adverse effects |
Use concomitantly with caution and appropriately monitor |
|
Estrogens and progestins |
Ethinyl estradiol and levonorgestrel: No substantial effect on exposures of ethinyl estradiol or levonorgestrel Hormonal contraceptives: Concomitant use not expected to affect efficacy of hormonal contraceptives Concomitant hormonal contraceptives may play role in rash associated with elexacaftor/tezacaftor/ivacaftor therapy |
Consider interruption of elexacaftor/tezacaftor/ivacaftor in patients receiving hormonal contraceptives who develop a rash; once rash resolves, consider resuming elexacaftor/tezacaftor/ivacaftor without the hormonal contraceptive; if rash does not recur, consider resuming hormonal contraceptive |
|
Grapefruit or grapefruit juice |
Possible increased elexacaftor, tezacaftor, and ivacaftor exposures |
Avoid concomitant use |
|
Immunosuppressants (cyclosporine, everolimus, sirolimus, tacrolimus) |
Possible increased immunosuppressant exposures, prolonged therapeutic effect, or increased risk of immunosuppressant-associated adverse effects |
Use concomitantly with caution; monitor patients appropriately |
|
St. John’s wort (Hypericum perforatum) |
Possible decreased elexacaftor, tezacaftor, and ivacaftor exposures and reduced efficacy of elexacaftor/tezacaftor/ivacaftor |
Concomitant use not recommended |
|
Warfarin |
Possible increased warfarin exposure |
Monitor INR and adjust warfarin dose if needed |
Elexacaftor, Tezacaftor, And Ivacaftor Pharmacokinetics
Absorption
Bioavailability
Elexacaftor: Absolute bioavailability 80%.
Tezacaftor and ivacaftor: Oral bioavailability not determined.
Peak plasma concentrations of elexacaftor, tezacaftor, and ivacaftor achieved approximately 6, 3, and 4 hours, respectively, following oral administration in the fed state.
Systemic exposure increases with accumulation ratio of approximately 2.2, 2.1, and 2.4 for elexacaftor, tezacaftor, and ivacaftor, respectively.
Steady-state concentrations of elexacaftor (once daily), tezacaftor (once daily), and ivacaftor (twice daily) achieved within 7, 8, and 3–5 days, respectively.
Food
Administration of single dose of fixed combination elexacaftor/tezacaftor/ivacaftor with fat-containing food resulted in systemic exposures of elexacaftor and ivacaftor about 1.9- to 2.5-fold and 2.5- to 4-fold, respectively, higher when compared with administration in fasting state; systemic exposures of tezacaftor similar to those observed with administration in fasting state.
Special Populations
Mild hepatic impairment (Child-Pugh class A): Effect on pharmacokinetics not studied.
Moderate hepatic impairment (Child-Pugh class B): Increases in AUCs of 25, 73, and 36% and in peak plasma concentrations of 12, 70, and 24% for elexacaftor, the active M23 metabolite of elexacaftor, and elexacaftor and the active M23 metabolite of elexacaftor combined, respectively. A 1.5-fold increase in AUC and a 10% increase in peak plasma concentrations reported for ivacaftor; tezacaftor AUC increases by 20%, and tezacaftor peak plasma concentrations not affected.
Severe hepatic impairment (Child-Pugh class C): Effect on pharmacokinetics not studied. Systemic exposures expected to be higher than that observed in patients with moderate hepatic impairment.
Renal impairment: Not studied in patients with severe renal impairment or in those with ESRD. Population pharmacokinetic data indicate that mild or moderate renal impairment does not substantially affect the clearance of elexacaftor or tezacaftor. Renal excretion of elexacaftor, tezacaftor, and ivacaftor is minimal.
Pediatric patients 2 to <18 years of age: Based on population pharmacokinetic analyses, exposures of elexacaftor, tezacaftor, and ivacaftor similar to those observed in adults.
Distribution
Extent
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
Elexacaftor: >99% (mainly albumin).
Tezacaftor: Approximately 99% (mainly albumin).
Ivacaftor: Approximately 99% (mainly α1-acid glycoprotein, albumin, human γ-globulin).
Elimination
Metabolism
Elexacaftor: Extensively metabolized principally by CYP3A4 and 3A5 to metabolites including M23, which has similar potency to the parent drug.
Tezacaftor: Extensively metabolized principally by CYP3A4 and 3A5 to metabolites including M1, which has similar potency to the parent drug.
Ivacaftor: Extensively metabolized principally by CYP3A4 and 3A5 to metabolites including M1, which has approximately one-sixth the potency of ivacaftor.
Elimination Route
Elexacaftor: Mainly excreted unchanged in feces (87.3%, primarily as metabolites); 0.23% excreted in urine.
Tezacaftor: Mainly excreted unchanged in feces (72% as unchanged drug or M2 metabolite); 14% excreted in urine (0.79% unchanged).
Ivacaftor: Mainly excreted in feces (87.8%); 6.6% excreted in urine.
Half-life
Elexacaftor: 27.4 hours (effective) and 24.7 hours (terminal) in patients with cystic fibrosis.
Tezacaftor: 25.1 hours (effective) and 60.3 hours (terminal) in patients with cystic fibrosis.
Ivacaftor: 15 hours (effective) and 13.1 hours (terminal) in patients with cystic fibrosis.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).
Actions
-
Elexacaftor/tezacaftor/ivacaftor combination therapy contains 3 drugs acting directly on CFTR protein, a chloride channel present at epithelial cell surface in multiple organs involved in salt and fluid transport. Elexacaftor and tezacaftor are CFTR correctors; ivacaftor is a CFTR potentiator.
-
Mutations in the gene encoding CFTR affect quantity or function of this protein at the cell surface resulting in cystic fibrosis.
-
Elexacaftor and tezacaftor bind to different sites on the CFTR protein and have an additive effect in facilitating the cellular processing and trafficking of select mutant forms of CFTR (including F508del-CFTR) to increase the amount of CFTR protein delivered to the cell surface.
-
Ivacaftor facilitates increased chloride transport by potentiating the probability of channel opening (or gating) of the CFTR protein at the cell surface.
-
Combined effect of elexacaftor, tezacaftor, and ivacaftor increases quantity and function of CFTR at cell surface, resulting in increased chloride transport.
-
In clinical studies, elexacaftor/tezacaftor/ivacaftor combination therapy improved lung function and decreased sweat chloride concentrations in patients homozygous or heterozygous for F508del mutation.
Advice to Patients
-
Advise patients to read the manufacturer's patient information.
-
Advise patients to take elexacaftor/tezacaftor/ivacaftor combination therapy with fat-containing food (e.g., eggs, butter, peanut butter, whole milk dairy products) to increase systemic absorption of the drug.
-
Advise patients to avoid food or drink containing grapefruit while receiving elexacaftor/tezacaftor/ivacaftor combination therapy.
-
If a dose of elexacaftor/tezacaftor/ivacaftor combination therapy is missed by ≤6 hours, take the dose with fat-containing food as soon as it is remembered. If a morning dose is missed by >6 hours, take the dose as soon as possible and omit the evening dose; take the morning dose on the following day at the regularly scheduled time. If an evening dose is missed by >6 hours, omit the evening dose and take the next morning dose at the regularly scheduled time. Never take the morning and evening doses together at the same time.
-
Stress importance of considering risks and benefits of elexacaftor/tezacaftor/ivacaftor combination therapy in patients with moderate hepatic impairment (Child-Pugh class B) prior to initiating therapy; stress importance of dosage reduction in such patients. Stress importance of closely monitoring liver function tests in patients with mild or moderate hepatic impairment. Avoid use in patients with severe hepatic impairment (Child-Pugh class C).
-
Risk of elevated liver function test results. Monitor liver function tests prior to initiation of elexacaftor/tezacaftor/ivacaftor combination therapy, then every month during the first 6 months of treatment, every 3 months for the next 12 months, and at least annually thereafter. More frequent monitoring may be necessary in patients with a history of liver disease or liver function test elevations at baseline.
-
Instruct patients to interrupt treatment if symptoms of liver injury occur (e.g., jaundice, right upper quadrant pain, nausea, vomiting, altered mental status, ascites) and to notify their clinician immediately.
-
Hypersensitivity reactions including angioedema and anaphylaxis are possible with use of elexacaftor/tezacaftor/ivacaftor combination therapy. Inform patients of the early signs of hypersensitivity reactions including rash, hives, itching, facial swelling, tightness of the chest, and wheezing. Advise patients to discontinue use of elexacaftor/tezacaftor/ivacaftor combination therapy immediately and contact their physician or go to the emergency department if these symptoms occur.
-
Ocular lens opacities (cataracts) observed in some pediatric patients. Stress importance of baseline and follow-up ophthalmologic examinations in pediatric patients receiving elexacaftor/tezacaftor/ivacaftor combination therapy.
-
May cause dizziness. Advise patients to avoid activities requiring alertness, including driving or operating machinery, until effects are known.
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, vitamins, and herbal supplements, as well as any concomitant illnesses (e.g., hepatic impairment). Concomitant use of elexacaftor/tezacaftor/ivacaftor combination therapy with CYP3A inhibitors and inducers requires particular attention.
-
Advise patients to inform clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
The fixed combination of elexacaftor/tezacaftor/ivacaftor can only be obtained through select specialty pharmacies and distributors.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Kit, Granules |
elexacaftor 80 mg, tezacaftor 40 mg, and ivacaftor 60 mg co-packaged with ivacaftor 59.5 mg |
Trikafta (available as 4 wallets, each containing 7 unit-dose packets of elexacaftor, tezacaftor, and ivacaftor oral granules and 7 unit-dose packets of ivacaftor oral granules) |
Vertex Pharmaceuticals |
|
elexacaftor 100 mg, tezacaftor 50 mg, and ivacaftor 75 mg copackaged with ivacaftor 75 mg |
Trikafta (available as 4 wallets, each containing 7 unit-dose packets of elexacaftor, tezacaftor, and ivacaftor oral granules and 7 unit-dose packets of ivacaftor oral granules) |
Vertex Pharmaceuticals |
||
|
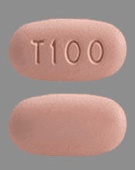
Kit, Tablets |
elexacaftor 50 mg, tezacaftor 25 mg, and ivacaftor 37.5 mg co-packaged with ivacaftor 75 mg |
Trikafta (available as blister cards containing 14 fixed-combination elexacaftor, tezacaftor, and ivacaftor tablets and 7 single-entity ivacaftor tablets) |
Vertex Pharmaceuticals |
|
|
elexacaftor 100 mg, tezacaftor 50 mg, and ivacaftor 75 mg copackaged with ivacaftor 150 mg |
Trikafta (available as 4 wallets, each containing 14 fixed-combination elexacaftor, tezacaftor, and ivacaftor tablets and 7 ivacaftor tablets) |
Vertex Pharmaceuticals |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about elexacaftor / ivacaftor / tezacaftor
- Check interactions
- Compare alternatives
- Reviews (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: CFTR combinations
- En español
Patient resources
- Elexacaftor, ivacaftor, and tezacaftor drug information
- Elexacaftor, tezacaftor, ivacaftor and ivacaftor (Advanced Reading)