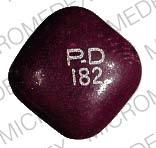
Pyridium Plus Disease Interactions
There are 33 disease interactions with Pyridium Plus (butabarbital / hyoscyamine / phenazopyridine).
- Autonomic neuropathy
- GI obstruction
- Glaucoma
- Obstructive uropathy
- Reactive airway diseases
- Myasthenia gravis
- Infectious diarrhea
- Acute alcohol intoxication
- Drug dependence
- Liver disease
- Porphyria
- Rash
- Respiratory depression
- G-6-PD deficiency
- Hepatitis
- Renal dysfunction
- Cardiac disease
- Tachycardia
- Coronary artery disease
- Gastric ulcer
- Gastroesophageal reflux
- Ulcerative colitis
- Liver disease
- Renal failure
- Adrenal insufficiency
- Depression
- Hematologic toxicity
- Osteomalacia
- Paradoxical reactions
- Hypertension
- Hyperthyroidism
- Diarrhea
- Fever
Anticholinergics (applies to Pyridium Plus) autonomic neuropathy
Major Potential Hazard, High plausibility.
Agents with anticholinergic activity can exacerbate many of the manifestations of autonomic neuropathy, including tachycardia, anhidrosis, bladder atony, obstipation, dry mouth and eyes, cycloplegia and blurring of vision, and sexual impotence in males. Therapy with antimuscarinic agents and higher dosages of antispasmodic agents (e.g., dicyclomine or oxybutynin) should be administered cautiously in patients with autonomic neuropathy.
Anticholinergics (applies to Pyridium Plus) GI obstruction
Major Potential Hazard, High plausibility. Applicable conditions: Gastrointestinal Obstruction, Esophageal Obstruction
Anticholinergics are contraindicated in patients with obstructive diseases such as achalasia, esophageal stricture or stenosis, pyloroduodenal stenosis, stenosing peptic ulcer, pyloric obstruction, and paralytic ileus. Anticholinergics may further suppress intestinal motility with resultant precipitation or aggravation of toxic megacolon.
Anticholinergics (applies to Pyridium Plus) glaucoma
Major Potential Hazard, High plausibility. Applicable conditions: Glaucoma/Intraocular Hypertension
Anticholinergic agents are contraindicated in patients with primary glaucoma, a tendency toward glaucoma (narrow anterior chamber angle), or adhesions (synechiae) between the iris and lens, as well as for the elderly and others in whom undiagnosed glaucoma or excessive pressure in the eye may be present. Because anticholinergics cause mydriasis, they may exacerbate these conditions.
Anticholinergics (applies to Pyridium Plus) obstructive uropathy
Major Potential Hazard, High plausibility. Applicable conditions: Urinary Retention
In general, the use of anticholinergic agents is contraindicated in patients with urinary retention and bladder neck obstruction caused by prostatic hypertrophy. Dysuria may occur and may require catheterization. Also, anticholinergic drugs may aggravate partial obstructive uropathy. Caution is advised even when using agents with mild to moderate anticholinergic activity, particularly in elderly patients.
Anticholinergics (applies to Pyridium Plus) reactive airway diseases
Major Potential Hazard, Moderate plausibility. Applicable conditions: Asthma
The use of systemic anticholinergics is contraindicated in the treatment of lower respiratory tract symptoms including asthma. Muscarinic receptor antagonists reduce bronchial secretions, which can result in decreased fluidity and increased thickening of secretions. However, ipratropium does not produce these effects and can be used safely in treating asthma.
Antimuscarinics (applies to Pyridium Plus) myasthenia gravis
Major Potential Hazard, Moderate plausibility.
Because antimuscarinic agents have anticholinergic effects, they are contraindicated in patients with myasthenia gravis. Their use may be appropriate to reduce adverse muscarinic effects caused by an anticholinesterase agent.
Antiperistaltic agents (applies to Pyridium Plus) infectious diarrhea
Major Potential Hazard, High plausibility. Applicable conditions: Infectious Diarrhea/Enterocolitis/Gastroenteritis
The use of drugs with antiperistaltic activity (primarily antidiarrheal and antimuscarinic agents, but also antispasmodic agents such as dicyclomine or oxybutynin at high dosages) is contraindicated in patients with diarrhea due to pseudomembranous enterocolitis or enterotoxin-producing bacteria. These drugs may prolong and/or worsen diarrhea associated with organisms that invade the intestinal mucosa, such as toxigenic E. coli, Salmonella and Shigella, and pseudomembranous colitis due to broad-spectrum antibiotics. Other symptoms and complications such as fever, shedding of organisms and extraintestinal illness may also be increased or prolonged. In general, because antiperistaltic agents decrease gastrointestinal motility, they may delay the excretion of infective gastroenteric organisms or toxins and should be used cautiously in patients with any infectious diarrhea, particularly if accompanied by high fever or pus or blood in the stool. Some cough and cold and other combination products may occasionally include antimuscarinic agents for their drying effects and may, therefore, require careful selection when necessary.
Barbiturates (applies to Pyridium Plus) acute alcohol intoxication
Major Potential Hazard, High plausibility.
The use of barbiturates is contraindicated in patients with acute alcohol intoxication exhibiting depressed vital signs. The central nervous system depressant effects of barbiturates may be additive with those of alcohol. Severe respiratory depression and death may occur. Therapy with barbiturates should be administered cautiously in patients who might be prone to acute alcohol intake.
Barbiturates (applies to Pyridium Plus) drug dependence
Major Potential Hazard, High plausibility. Applicable conditions: Drug Abuse/Dependence, Alcoholism
Barbiturates have the potential to cause dependence and abuse. Tolerance as well as physical and psychological dependence can develop, particularly after prolonged use of excessive dosages. Abrupt cessation and/or a reduction in dosage may precipitate withdrawal symptoms. In patients who have developed tolerance to a barbiturate, overdosage can still produce respiratory depression and death, and cross-tolerance usually will occur with other agents in the class. Addiction-prone individuals, such as those with a history of alcohol or substance abuse, should be under careful surveillance or medical supervision when treated with barbiturates. It may be prudent to refrain from dispensing large quantities of medication to these patients. After prolonged use or if dependency is suspected, withdrawal of barbiturates should be undertaken gradually using a dosage-tapering schedule.
Barbiturates (applies to Pyridium Plus) liver disease
Major Potential Hazard, High plausibility.
Barbiturates are extensively metabolized by the liver. The plasma clearance of barbiturates may be decreased and the half-lives prolonged in patients with impaired hepatic function. Therapy with barbiturates should be administered cautiously and initiated at reduced dosages in patients with liver disease. Barbiturates are not recommended for use in patients with cirrhosis, hepatic failure, hepatic coma, or other severe hepatic impairment.
Barbiturates (applies to Pyridium Plus) porphyria
Major Potential Hazard, High plausibility.
The use of barbiturates is contraindicated in patients with a history of porphyria. Barbiturates may exacerbate acute intermittent porphyria or porphyria variegata by inducing the enzymes responsible for porphyrin synthesis.
Barbiturates (applies to Pyridium Plus) rash
Major Potential Hazard, High plausibility. Applicable conditions: Dermatitis - Drug-Induced
Skin eruptions may precede rare but potentially fatal barbiturate-induced reactions such as systemic lupus erythematosus and exfoliative dermatitis, the latter of which may be accompanied by hepatitis and jaundice. Therapy with barbiturates should be administered cautiously in patients with preexisting drug-induced dermatitis, since it may delay the recognition of a potential reaction to barbiturates. Barbiturate therapy should be withdrawn promptly at the first sign of a dermatologic adverse effect. However, cutaneous reactions may proceed to an irreversible stage even after cessation of medication due to the slow rate of metabolism and excretion of barbiturates. Patients should be advised to promptly report signs that may indicate impending development of barbiturate-related cutaneous lesions, including high fever, severe headache, stomatitis, conjunctivitis, rhinitis, urethritis, and balanitis. Rashes may be more likely to occur with phenobarbital and mephobarbital.
Barbiturates (applies to Pyridium Plus) respiratory depression
Major Potential Hazard, High plausibility. Applicable conditions: Pulmonary Impairment, Asphyxia, Respiratory Arrest
Barbiturates may produce severe respiratory depression, apnea, laryngospasm, bronchospasm and cough, particularly during rapid intravenous administration. In usual hypnotic dosages, the degree of respiratory depression produced is similar to that which occurs during physiologic sleep, while at higher dosages, the rate, depth and volume of respiration may be markedly decreased. However, some patients may be susceptible at commonly used dosages, including the elderly, debilitated or severely ill patients, those receiving other CNS depressants, and those with limited ventilatory reserve, chronic pulmonary insufficiency or other respiratory disorders. Therapy with barbiturates should be administered cautiously in these patients. Appropriate monitoring and individualization of dosage are particularly important, and equipment for resuscitation should be immediately available if the parenteral route is used. Barbiturates, especially injectable formulations, should generally be avoided in patients with sleep apnea, hypoxia, or severe pulmonary diseases in which dyspnea or obstruction is evident.
Phenazopyridine (applies to Pyridium Plus) G-6-PD deficiency
Major Potential Hazard, Moderate plausibility.
Patients with glucose-6-phosphate dehydrogenase (G-6-PD) deficiency may be at increased risk for phenazopyridine-induced methemoglobinemia and hemolytic anemia. These conditions have occurred rarely in other patients, except due to acute phenazopyridine overdose or impaired renal function. Therapy with phenazopyridine should be administered cautiously in patients with G-6-PD deficiency.
Phenazopyridine (applies to Pyridium Plus) hepatitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
The use of phenazopyridine is contraindicated in patients with severe hepatitis. Rare cases of hepatotoxicity have been associated with phenazopyridine, usually at overdose levels. Hypersensitivity hepatitis has also been reported. Therapy with phenazopyridine should be administered cautiously in patients with impaired hepatic function.
Phenazopyridine (applies to Pyridium Plus) renal dysfunction
Major Potential Hazard, High plausibility.
The use of phenazopyridine is contraindicated in patients with impaired renal function. Phenazopyridine is primarily eliminated unchanged by the kidney and may accumulate to toxic levels during prolonged administration in such patients. Reported cases of toxicity due to overdosage have resulted in acute renal failure and methemoglobinemia. Likewise, administration of phenazopyridine to patients with preexisting renal failure has led to methemoglobinemia and hemolytic anemia. Phenazopyridine toxicity may be associated with a yellowish tinge of the skin or sclera.
Anticholinergics (applies to Pyridium Plus) cardiac disease
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Cardiovascular Disease
Anticholinergics block vagal inhibition of the SA nodal pacemaker. Therapy with anticholinergics should be administered cautiously to patients with tachycardia, congestive heart failure, or coronary artery disease. Premature ventricular depolarization, ventricular tachycardia, and fibrillation associated with anticholinergics are rare.
Anticholinergics (applies to Pyridium Plus) tachycardia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Arrhythmias
Anticholinergics block vagal inhibition of the SA nodal pacemaker. Therapy with anticholinergics should be administered cautiously in patients with tachycardia, congestive heart failure, or coronary artery disease. Premature ventricular depolarization or ventricular tachycardia or fibrillation associated with anticholinergics is rare.
Antimuscarinics (applies to Pyridium Plus) coronary artery disease
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Arrhythmias, Ischemic Heart Disease
Antimuscarinic agents block vagal inhibition of the SA nodal pacemaker. These agents should be administered cautiously in patients with tachycardia, congestive heart failure, or coronary artery disease. Premature ventricular depolarization or ventricular tachycardia or fibrillation associated with antimuscarinic drugs is rare.
Antimuscarinics (applies to Pyridium Plus) gastric ulcer
Moderate Potential Hazard, Low plausibility. Applicable conditions: Bleeding
Antimuscarinic agents may cause a delay in gastric emptying and possibly antral stasis in patients with gastric ulcer. Therapy with antimuscarinic agents should be administered cautiously to patients with gastric ulcer.
Antimuscarinics (applies to Pyridium Plus) gastroesophageal reflux
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Gastroesophageal Reflux Disease
Antimuscarinic agents decrease gastric motility and relax the lower esophageal sphincter which promotes gastric retention and can aggravate reflux. These drugs should be administered cautiously in patients with gastroesophageal reflux or hiatal hernia associated with reflux esophagitis.
Antimuscarinics (applies to Pyridium Plus) ulcerative colitis
Moderate Potential Hazard, Moderate plausibility.
Antimuscarinic agents may suppress intestinal motility and produce paralytic ileus with resultant precipitation of toxic megacolon. These drugs should be administered cautiously to patients with ulcerative colitis.
Atropine-like agents (applies to Pyridium Plus) liver disease
Moderate Potential Hazard, Moderate plausibility.
Atropine-like agents undergo significant hepatic metabolism. Therapy with atropine-like agents should be administered cautiously to patients with liver disease.
Atropine-like agents (applies to Pyridium Plus) renal failure
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction
Atropine-like agents are primarily eliminated by the kidney. Therapy with atropine-like agents should be administered cautiously to patients with renal disease.
Barbiturates (applies to Pyridium Plus) adrenal insufficiency
Moderate Potential Hazard, High plausibility. Applicable conditions: Panhypopituitarism
Barbiturates, especially phenobarbital, secobarbital and butabarbital, may diminish the systemic effects of exogenous and endogenous corticosteroids via induction of hepatic microsomal enzymes, thereby accelerating the metabolism of corticosteroids. In addition, barbiturates may interfere with pituitary corticotropin production. Therapy with barbiturates should be administered cautiously in patients with adrenal insufficiency. Patients with borderline hypoadrenalism should be monitored closely, and patients receiving steroid supplementation may require an adjustment in dosage when barbiturates are added to or withdrawn from their medication regimen.
Barbiturates (applies to Pyridium Plus) depression
Moderate Potential Hazard, High plausibility.
Barbiturates depress the central nervous system and may cause or exacerbate mental depression. Therapy with barbiturates should be administered cautiously in patients with a history of depression or suicidal tendencies. It may be prudent to refrain from dispensing large quantities of medication to these patients.
Barbiturates (applies to Pyridium Plus) hematologic toxicity
Moderate Potential Hazard, Low plausibility. Applicable conditions: Bone Marrow Depression/Low Blood Counts
Hematologic toxicity, including agranulocytosis, thrombocytopenic purpura and megaloblastic anemia, has been reported rarely during use of barbiturates. Therapy with barbiturates should be administered cautiously in patients with preexisting blood dyscrasias or bone marrow suppression. Blood counts are recommended prior to and periodically during long-term therapy, and patients should be instructed to immediately report any signs or symptoms suggestive of blood dyscrasia such as fever, sore throat, local infection, easy bruising, petechiae, bleeding, pallor, dizziness, or jaundice. Barbiturate therapy should be discontinued if blood dyscrasias occur.
Barbiturates (applies to Pyridium Plus) osteomalacia
Moderate Potential Hazard, Low plausibility. Applicable conditions: Vitamin D Deficiency
Rickets and osteomalacia have rarely been reported following prolonged use of barbiturates, possibly due to increased metabolism of vitamin D as a result of enzyme induction by barbiturates. Long-term therapy with barbiturates should be administered cautiously in patients with vitamin D deficiency.
Barbiturates (applies to Pyridium Plus) paradoxical reactions
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperkinetic Syndrome of Childhood
Paradoxical reactions characterized by excitability and restlessness may occur in pediatric patients with hyperactive aggressive disorders. Such patients should be monitored for signs of paradoxical stimulation during therapy with barbiturates.
Anticholinergics (applies to Pyridium Plus) hypertension
Minor Potential Hazard, Low plausibility.
Cardiovascular effects of anticholinergics may exacerbate hypertension. Therapy with anticholinergic agents should be administered cautiously in patients with hypertension.
Anticholinergics (applies to Pyridium Plus) hyperthyroidism
Minor Potential Hazard, Low plausibility.
In general, agents with anticholinergic activity may exacerbate hyperthyroidism. Therapy with anticholinergics should be administered cautiously in patients with hyperthyroidism. Thyroid levels should be monitored if usage is prolonged.
Antimuscarinics (applies to Pyridium Plus) diarrhea
Minor Potential Hazard, Moderate plausibility.
Diarrhea may be a symptom of incomplete intestinal obstruction, especially in patients with ileostomy or colostomy. Antimuscarinic agents may further aggravate the diarrhea. Therefore, these drugs should be administered cautiously in patients with diarrhea.
Atropine-like agents (applies to Pyridium Plus) fever
Minor Potential Hazard, Low plausibility.
Atropine-like agents may increase the risk of hyperthermia in patients with fever by producing anhidrosis. Therapy with atropine-like agents should be administered cautiously in febrile patients.
Switch to professional interaction data
Pyridium Plus drug interactions
There are 713 drug interactions with Pyridium Plus (butabarbital / hyoscyamine / phenazopyridine).
Pyridium Plus alcohol/food interactions
There are 2 alcohol/food interactions with Pyridium Plus (butabarbital / hyoscyamine / phenazopyridine).
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.