Watchman Implant
Medically reviewed by Drugs.com. Last updated on May 4, 2025.
AMBULATORY CARE:
The Watchman® implant
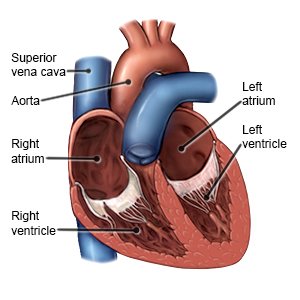
is a permanent heart device. The implant is designed to prevent blood clots caused by atrial fibrillation (A-fib) from getting into the bloodstream. A-fib prevents the heart from pumping blood correctly. Blood that is not pumped out may pool in a part of the heart called the left atrial appendage. Blood clots may form in the pooled blood. If a clot moves out of the appendage and into the bloodstream, it can cause a stroke. The implant closes off the appendage to prevent clots from moving into the bloodstream. This helps lower your risk for a stroke.
 |
How to prepare for the implant to be placed:
- Your healthcare provider will tell you how to prepare for the procedure. He or she may tell you not to eat or drink anything after midnight on the day of the procedure. Arrange to have someone drive you home after you are discharged.
- Your provider will use a type of CT scan to check your atrial appendage for clots. The size, shape, and exact location of your atrial appendage will also be checked.
- You may need blood tests or scans of your leg and heart veins. You will be checked heart or carotid artery problems. Certain problems will prevent you from being able to get the implant.
What will happen during the procedure:
- General anesthesia is usually used. General anesthesia will keep you asleep and free from pain. Your surgeon will insert a catheter (thin tube) into a vein in your leg. He or she will move the catheter up and into the left atrial appendage.
- The catheter will be removed. The device will be pushed through the catheter and into the appendage. As it comes out of the catheter, the implant will open like a parachute. It will fill the opening of the appendage. Over time, heart tissue will grow over the implant. This seals the opening so clots cannot come out of the appendage.
- The catheter will be removed from the vein in your leg. The site will be covered with a bandage. Pressure may be applied to help stop any bleeding. You will then be taken to a room to be monitored for any problems. When healthcare providers see you are okay, you will be taken to a hospital room.
What to expect after the procedure:
- You will may in the hospital overnight after the procedure. You may be able to go home the next day. Your healthcare provider will tell you if you need to stay longer for more monitoring.
- You may have a bruise or swelling where the catheter went into your skin. The area may be sore or tender. These symptoms are normal and should go away in a few days.
- You will need to take blood thinning medicine until heart tissue grows over the implant. This usually takes about 6 weeks.
- Your healthcare provider will use a transesophageal echocardiogram (TEE) about 45 days after the procedure. The TEE will show any gaps around the implant. It will also show any blood clots that may have formed because of the implant.
Risks of the Watchman implant:
Your heart may be punctured during the procedure. You may have an air embolism (air or bubbles block a blood vessel). An air embolism can cause a stroke. The device may cause a clot to form and move into your bloodstream. The device may not cover the whole atrial appendage. A gap can allow blood clots to leave the atrial appendage and move into your bloodstream. It may take longer than expected for your body to heal over the device. You may have an allergic reaction to the implant. Your heart may develop an irregular rhythm. You may develop a fistula (abnormal opening between 2 areas). You may bleed more than expected or have brain, groin, or stomach bleeding. Your blood pressure may drop too low. You may develop an infection or pneumonia.
Call your local emergency number (911 in the US) if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- You have trouble breathing or shortness of breath.
- You cough up blood.
Drugs used to treat this and similar conditions
Xarelto
Xarelto (rivaroxaban) is a factor Xa inhibitor used to reduce the risk of blood clots and stroke in ...
Multaq
Multaq (dronedarone) is an antiarrhythmic medication used to treat atrial fibrillation and atrial ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Coreg
Coreg (carvedilol) is used to treat heart failure and hypertension (high blood pressure). Includes ...
Lanoxin
Lanoxin (digoxin) is used to treat congestive heart failure and atrial fibrillation. Includes ...
Rivaroxaban
Rivaroxaban systemic is used for atrial fibrillation, cardiovascular risk reduction, congenital ...
Propafenone
Propafenone systemic is used for atrial fibrillation, atrial flutter, ventricular tachycardia ...
Sotalol
Sotalol is a beta-blocker with antiarrhythmic properties that affects the heart and circulation ...
Carvedilol
Carvedilol (Coreg) is used to treat heart failure and hypertension (high blood pressure). Includes ...
Flecainide
Flecainide systemic is used for atrial fibrillation, atrial flutter, paroxysmal supraventricular ...
Seek care immediately if:
- Your leg feels warm, tender, and painful. It may look swollen and red.
- You have signs of an infection at the catheter site, such as swelling, redness, or pus.
- You feel weak, dizzy, or faint.
- You have numbness or tingling in an arm or leg.
- The bruise where the catheter went in suddenly gets bigger.
- Your catheter insertion site is bleeding heavily and does not stop after 5 to 10 minutes of pressure.
Call your doctor or cardiologist if:
- You have a fever.
- You have pain or bleeding at the catheter site.
- You have questions or concerns about your condition or care.
Medicines:
Your healthcare provider will tell you when to take the following medicines. You will not be taking all of the medicines at the same time. You will take a blood thinner for about 6 weeks. Then, if the implant is working you will stop taking blood thinners and start taking antiplatelets and aspirin. In about 6 months, you may be able to stop taking antiplatelets and only take aspirin. Do not move from one medicine to another until your provider tells you to.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Antiplatelets , such as aspirin, help prevent blood clots. Take your antiplatelet medicine exactly as directed. These medicines make it more likely for you to bleed or bruise. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead.
- Aspirin helps lower the risk for blood clots. Your healthcare provider will tell you how much aspirin to take each day. You will need to continue taking aspirin indefinitely.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Activity:
- Rest as needed. You may feel like resting more for the first day after your procedure. Do not make any important decisions, drive, or operate heavy machinery for 24 hours. You may still feel the effects of general anesthesia during this time.
- Ask when you can return to your regular activities. Your healthcare provider will tell you when it is okay to drive, return to work, and do other activities. Do not lift heavy objects, climb stairs, or do any strenuous activity for at least 3 days. Your provider may also tell you to avoid certain movements, such as bending. You may be able to walk short distances while you heal. Walking helps prevent blood clots. Your provider will give you specific instructions to follow.
Care for the catheter site:
- Keep the bandage on the catheter site for 1 day. Then you can remove the bandage. If the wound starts bleeding, apply firm pressure for 10 minutes. Use gauze or a clean towel to apply pressure.
- Check the catheter site for signs of infection, such as redness, swelling, or pus.
- Ask when you can bathe after your procedure. Your healthcare provider may tell you to take a shower instead of a bath if the bandage is still in place. Cover the bandage and keep it dry during the shower. Pat your skin dry. Do not rub over the catheter site to dry your skin.
- Ice the area to reduce swelling, bruising, and pain. Use an ice pack, or put crushed ice in a plastic bag. Wrap a towel around it before you apply it to the site. Apply it for 20 minutes every hour, or as directed.
Manage A-fib:
The Watchman implant is not a treatment for A-fib. You will still need to do the following to prevent irregular heartbeats or other problems:
- Know your target heart rate. Learn how to take your pulse and monitor your heart rate.
- Manage other health conditions. This includes high blood pressure, sleep apnea, thyroid disease, diabetes, and other heart conditions. Take medicine as directed and follow your treatment plan.
- Limit or do not drink alcohol. Alcohol can make a-fib hard to manage. Ask your healthcare provider if it is okay for you to drink alcohol. He or she may want you to limit the number of drinks you have in a day. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause heart and lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Eat heart-healthy foods. Heart healthy foods will help keep your cholesterol low. These include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Replace butter and margarine with heart-healthy oils such as olive oil and canola oil.

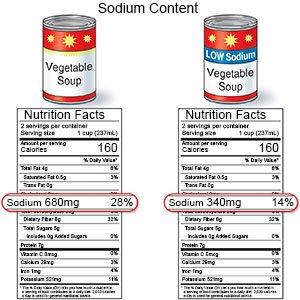
- Eat less sodium (salt). Sodium can affect how your heart works. Your healthcare provider will can tell you how much sodium is okay for you. Try not to add salt to food you cook. If you salt food as you cook, try not adding more at the table. Use herbs to season foods. Read labels in the grocery store so you can choose low-sodium options.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a weight loss plan if you are overweight.
- Exercise for 30 minutes most days of the week. Ask your healthcare provider about the best exercise plan for you.
Follow up with your doctor or cardiologist as directed:
You will need to return in 6 weeks to make sure the atrial appendage is closed. You will also need to return in 6 months for a check. After that, you may be able to come in 1 time each year for a check. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
