Removal of Implantable Cardioverter Defibrillator
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
Removal of an implantable cardioverter defibrillator (ICD)
may be needed due to infection around the device or in the heart tissue.
How to prepare for ICD removal:
- Your surgeon will tell you how to prepare for surgery. Your surgeon may tell you not to eat or drink anything after midnight on the day of your surgery. Arrange for someone to drive you home and stay with you after surgery.
- Tell your surgeon about all your current medicines. Your surgeon will tell you if you need to stop any medicine for surgery, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- Make arrangements at home and work, if needed. You will not be able to lift anything heavy for several days after surgery. Someone may need to help you around the house during this time. Ask when you can return to work after surgery. You may need to arrange for time off.
What will happen during ICD removal:
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given IV sedation and local anesthesia to numb the surgery area. With local anesthesia, you may still feel pressure or pushing, but you should not feel pain.
- Your surgeon will make an incision in your chest. All parts of the ICD will then be removed. Your surgeon may remove infected tissue or take a sample to test for the type of germ causing infection.
- Your surgeon may also place a drain to allow the infection to heal. The incision may be closed with stitches or staples. A bandage will be placed over the area to prevent an infection.
What to expect after ICD removal:
- You will be taken to a recovery room where you will rest until you are awake. You may be able to leave when you are awake and your pain is controlled. You may instead be taken to a hospital room.
- You will be on a heart monitor. A heart monitor is an EKG that stays on continuously to record your heart's electrical activity. You may need to stay on a heart monitor in the hospital until your infection is gone and you can have another ICD placed.
- You may need wound care to help your infection heal. You may also need several weeks of IV antibiotic therapy.
Risks of ICD removal:
You may bleed more than usual or get a blood clot after surgery. Your heart or blood vessels may be damaged and you may need more surgery. You may also need a wearable cardioverter defibrillator (WCD), or temporary transcutaneous pacing, to prevent a cardiac arrest. A cardiac arrest is when your heart stops beating. You may need to have another ICD placed after your infection is gone.
Call your local emergency number (911 in the US), or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have trouble breathing.
- You lose consciousness or stop breathing.
Related medications
Seek care immediately if:
- Blood soaks through your bandage.
- Your stitches come apart.
Call your doctor or surgeon if:
- You have a fever or chills.
- Your surgery area is red, swollen, or draining pus.
- You have nausea or are vomiting.
- Your skin is itchy, swollen, or you have a rash.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Heart medicine may be given to strengthen or control your heartbeat.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antibiotics help treat an infection.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for the surgery area as directed:
Wear loose-fitting clothing over the area. Do not get the area wet until your healthcare provider says it is okay. Carefully wash the area with soap and water. Dry the area and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. Do not put powders or lotions on the area. Check every day for signs of infection, such as swelling, redness, or pus. Empty your drain as directed. Write down how much you empty each time.
Self-care:
- Apply ice on the procedure area for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel before you apply it to your skin. Ice helps prevent tissue damage and decreases swelling and pain.
- Do not lift anything heavier than 10 pounds, or as directed. Ask your healthcare provider when you can lift heavy objects.
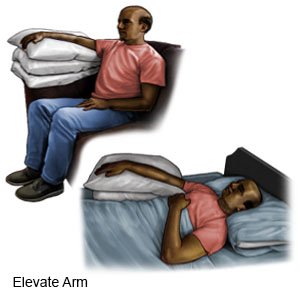
- Limit the use of your arm nearest to the surgery area. Place your arm closest to the area in a sling. Wear the sling as directed to help decrease swelling and pain. Prop your arm on pillows or blankets when you take off your sling to keep it elevated comfortably. Do not lift the arm closest to the incision area over your head for 5 days. Do gentle range of motion exercises (ROM) exercises as directed to prevent arm and shoulder stiffness.
Follow up with your doctor or surgeon as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Removal of Implantable Cardioverter Defibrillator
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
