Peripheral Artery Disease
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is peripheral artery disease (PAD)?
PAD is narrow, weak, or blocked arteries that prevents blood flow to your legs and arms. It may affect any arteries outside of your heart and brain. PAD is usually the result of a buildup of fat and cholesterol, also called plaque, along your artery walls. Inflammation, a blood clot, or abnormal cell growth could also block your arteries. You are at risk for an amputation if poor blood flow keeps wounds from healing or causes gangrene (tissue death). Without treatment, PAD can also cause a heart attack or stroke.
What increases my risk for PAD?
- Cigarette use
- Diabetes
- High blood pressure
- High cholesterol
- Age 65 years or older
- Age 50 years or older, if you also have at least 1 other risk factor
- Heart disease or a family history of heart disease
What are the signs and symptoms of PAD?
Mild PAD usually does not cause symptoms. As the disease worsens, you may have the following:
- Pain or cramps in your leg or hip while you walk
- A numb, weak, or heavy feeling in your legs
- Dry, scaly, red, or pale skin on your legs
- Thick or brittle nails, or hair loss on your arms and legs
- Foot sores that will not heal
- Burning or aching in your feet and toes while resting (this may be worse when you lie down)
How is PAD diagnosed?
- Angiography is a test that shows pictures of the arteries in your arms and legs. You will be given contrast liquid to help the arteries show up better on the pictures. The pictures will be taken with an MRI or CT scan. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. The MRI uses a powerful magnet. Metal can cause serious injury from the magnet. Tell a healthcare provider if you have any metal in or on your body.
- Doppler ankle brachial index (ABI) is a test that compares blood pressure in your ankles to blood pressure in your arms. This tells your healthcare provider how well blood is flowing through the arteries in your legs.
Related medications
How is PAD treated?
Treatment can help reduce your risk for a heart attack, stroke, or amputation. You may need more than one of the following:
- Medicines may be given to help prevent blood clots. You may also need medicines to lower your cholesterol or blood pressure.
- A supervised exercise program helps you stay active in normal daily activities. Healthcare providers will help you safely walk or do strength training exercises 3 times a week for 30 to 60 minutes. You will do this for several months, then transition to walking on your own.
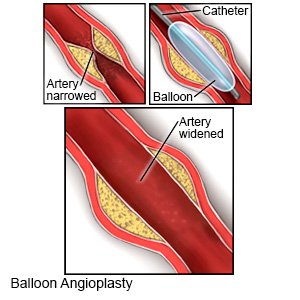
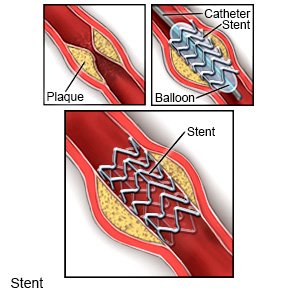
- Angioplasty is a procedure to open your artery so blood can flow through normally. A thin tube called a catheter is used to insert a small balloon into your artery. The balloon is inflated to open your blocked artery, and then removed. A tube called a stent may be placed in your artery to hold it open.
- Bypass surgery is used to make a new connection to your artery with a vein from another part of your body, or an artificial graft. The vein or graft is attached to your artery above and below your blockage. This allows blood to flow around the blocked portion of your artery.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I manage PAD?
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can worsen PAD. They can also increase your risk for a heart attack or stroke. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Manage any other health conditions you have. Take your medicines as directed. Follow your provider's instructions if you have high blood pressure or high cholesterol. Check your blood sugar levels as directed if you have diabetes.
- Eat heart-healthy foods. Eat whole grains, fruits, and vegetables every day. Limit salt and high-fat foods. Ask your provider for more information on a heart healthy diet. Ask what a healthy weight is for you. Your provider can help you create a healthy weight-loss plan, if needed.

- Check your feet each day. You may not be able to feel a cut or sore, or shoes that are too tight. Check your whole foot for wounds, corns, and calluses. Do not ignore small problems, such as dry skin or small wounds. These can become life-threatening without proper care. A foot specialist may need to cut your toenails, care for wounds, or remove corns. Your provider may tell you how often to see the specialist.
Call your local emergency number (911 in the US) if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
When should I seek immediate care?
- You have sores or wounds that will not heal.
- You notice black or discolored skin on your arm or leg.
- Your skin is cool to the touch.
When should I call my doctor?
- You have leg pain when you walk ⅛ mile (200 meters) or less, even with treatment.
- Your legs are red, dry, or pale, even with treatment.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Peripheral Artery Disease
Treatment options
- Medications for Aortic Aneurysm
- Medications for Bleeding Disorder
- Medications for Cardiovascular Conditions and Disorders
- Medications for Peripheral Arterial Disease
- Medications for Renal Artery Atherosclerosis
- Medications for Thromboangiitis Obliterans
- Medications for Thrombotic/Thromboembolic Disorder
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
