Lumbar Puncture
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
A lumbar puncture is a procedure used to collect cerebrospinal fluid (CSF). CSF is a clear, protective fluid that flows around the brain and inside the spinal canal. A lumbar puncture is usually done to check for an infection, inflammation, bleeding, or other conditions that affect the brain. It may also be done to remove CSF to reduce pressure in the brain.
How do I prepare for a lumbar puncture?
- You may need to have blood tests, x-rays, or other tests. Brain imaging tests, such as CT scan or MRI, may also be done.
- Tell the provider if you have a blood disorder or have ever had a bleeding problem. Tell your provider if you are taking any medicine that may make you more likely to bleed. These include aspirin, clot busters, and blood thinners. The provider will have to decide if it is safe for you to have a lumbar puncture. He or she may have you stop taking certain blood thinners a few days before the procedure. Do not stop taking this medicine unless directed by your healthcare provider.
- Tell your healthcare provider if you have any allergies. This includes an allergy to a cleansing solution, such as iodine, or any numbing medicine.
- Tell your healthcare provider if you have a blood disorder or have ever had a bleeding problem.
- Ask a family member or friend to drive you home after your procedure. Do not drive yourself home.
What will happen during a lumbar puncture?
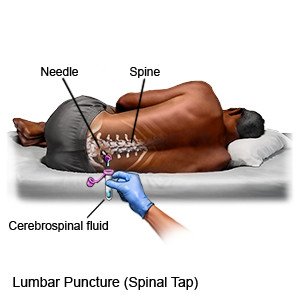 |
- You will be asked to lie on your side or to sit up. If you are on your side, your knees will be bent and drawn up toward your chest. Your neck will be tucked toward your chest and you may be given a pillow. If you are sitting, you will need to bend forward with your neck tucked toward your chest. You may be given medicine to help you relax or make you drowsy.
- Your healthcare provider will feel your lower spine to look for the best place to do the lumbar puncture. He or she will mark this position using a marker. You may be given one or more shots of numbing medicine under the skin. A needle is inserted between the vertebrae (spine) in your lower back. You may feel some pushing or discomfort as the needle enters your back. Tell your healthcare provider if you have pain that does not stop within a few seconds. Your healthcare provider may need to remove, reinsert, or change the position of the needle.
- Your healthcare provider may take readings of your CSF pressure. This is done by connecting a measuring device to the needle. After the pressure is measured, the device is removed and CSF is allowed to flow out of the needle. Samples of your CSF may be taken and placed in sterile bottles. The needle will then be taken out and the area will be covered with a bandage.
Related medications
What should I expect after a lumbar puncture?
Lie flat in bed until your healthcare provider says it is okay to get up. Tell a healthcare provider if you have a headache, back pain, or tingling, numbness, or weakness below your waist.
- Medicines may be given to relieve pain.
- You may develop a headache during the first few hours after your procedure. The headache may last for several days. It may be mild to severe and may get worse when you sit or stand. You may be asked to drink more liquid than usual after your procedure. Caffeine may be used to treat a post-lumbar puncture headache. Caffeine may be given in drinks, such as coffee or soda, every 4 to 6 hours. You may also be given caffeine through an IV.
What are the risks of a lumbar puncture?
You may have neck or back pain. There may be bleeding, infection, or injury to a disc in your spine. Spinal fluid may leak from the puncture site. Your nerves or spinal cord may be damaged. Patients who have blood disorders or who are taking certain medicines are at a higher risk for problems.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
