Laparoscopic Oophorectomy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
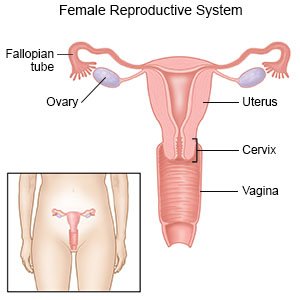
A laparoscopic oophorectomy
is surgery to remove one or both of your ovaries. Your surgeon will use a laparoscope (a thin tube with a light and tiny video camera on the end) and small tools to remove your ovaries. He or she may use a robot (machine) that has mechanical arms to operate the tools. This is called a robotic-assisted laparoscopic oophorectomy.
 |
How to prepare for a laparoscopic oophorectomy:
Your surgeon will talk to you about how to prepare for surgery. He or she may tell you not to eat or drink anything after midnight on the day of your surgery. He or she will tell you what medicines to take or not take on the day of your surgery. You may need to stop taking blood thinners, aspirin, or NSAIDs several days before surgery. You may need blood tests, an x-ray, CT scan, or ultrasound before surgery. Arrange for someone to drive you home when you are discharged.
What will happen during a laparoscopic oophorectomy:
- You will be given general anesthesia to keep you asleep and free from pain during surgery. Your surgeon will make an incision in your belly button and insert a laparoscope. A laparoscope is a long metal tube with a light and camera on the end. Your surgeon will also insert other tools through 2 to 3 smaller incisions made at different places on your abdomen. The abdomen will then be inflated with a gas (carbon dioxide). This lifts your abdomen away from your organs and gives your surgeon more space to work.

- Your surgeon may make more incisions if he or she uses robot assistance. He or she will use small tools to cut and remove one or both of your ovaries. The incisions will be closed with strips of surgical tape, stitches, or surgical glue and covered with bandages. A vaginal pack or sanitary pad may be used to absorb the bleeding. A vaginal pack is a special gauze that is inserted into the vagina and removed before you go home or to a hospital room.
What will happen after a laparoscopic oophorectomy:
Healthcare providers will monitor you until you are awake. You may be able to go home when your pain is controlled, or you may need to spend the night in the hospital. You may have bleeding or discharge from your vagina for several days. You may also feel pain in your shoulder or back. This is caused by the air that is put into your abdomen during surgery. Walk around as soon as you are awake after surgery. This may prevent blood clots.
Risks of a laparoscopic oophorectomy:
If both of your ovaries are removed, you may need to take hormone replacement medicine. This will prevent osteoporosis (brittle bones) and symptoms of menopause. Your uterus, bladder, or intestines may be injured during surgery. Problems may happen during your laparoscopic surgery and you may need an open surgery. You may bleed more than expected or get an infection. You may get a blood clot in your leg or arm. This may become life-threatening.
Call your local emergency number (911 in the US) for any of the following:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Related medications
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- Blood soaks through your bandage.
- Your stitches come apart.
Call your doctor if:
- You have a fever or chills.
- Your wound is red, swollen, or draining pus.
- You have pus or a foul-smelling odor coming from your vagina.
- You have nausea or are vomiting.
- You have trouble urinating or having a bowel movement.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Hormone medicine may be given if both ovaries are removed. This medicine will replace hormones in your body that your ovaries produced. You may not be started on this medicine for until 2 to 3 months after surgery.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for your surgery area as directed:
When you are allowed to bathe, carefully wash around the area with soap and water. Gently dry the area and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. If you have strips of medical tape, let them fall off on their own.
Activity:
Ask your healthcare provider when you can return to your normal activities. Do not have sex, douche, or use tampons until your healthcare provider says it is okay. These actions may cause an infection. Do not exercise or lift anything heavy until your healthcare provider says it is okay. This may put too much stress on your incision.
Ask for help:
This surgery may be life-changing for you and your family. You will no longer be able to get pregnant if both of your ovaries are removed. Sudden changes in the levels of your hormones may occur and cause mood swings and depression. You may feel angry, sad, or frightened, or cry frequently and unexpectedly. These feelings are normal. Talk to your healthcare provider about where you can get support.
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
