Implantable Cardioverter Defibrillator
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about implantable cardioverter defibrillator (ICD):
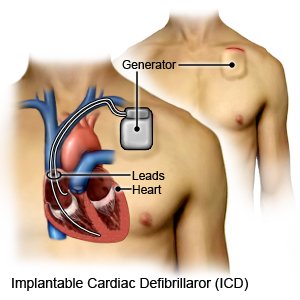
An ICD is a small device that monitors your heart rate and rhythm. It is placed inside your chest or abdomen. An ICD may be used if you have a life-threatening arrhythmia. An arrhythmia is an irregular heart rate or a heart rate that is too fast or too slow. Some arrhythmias may cause your heart to stop beating suddenly. An ICD can give a shock to your heart to make it start beating again. It can also make your heartbeat faster or slower.
 |
How to prepare for insertion of an ICD:
- Your surgeon will talk to you about how to prepare for the procedure. Your surgeon may tell you not to eat or drink anything after midnight on the day of your procedure. Arrange to have someone drive you home and stay with you after the procedure.
- Tell your surgeon about all medicines you currently take. Your surgeon will tell you if you need to stop any medicine for the procedure, and when to stop. Your surgeon will tell you which medicines to take or not take on the day of your procedure.
- Tell your surgeon about all your allergies, including antibiotics. You may be given an antibiotic through your IV to help prevent a bacterial infection.
- Make arrangements at home and work, if needed. You will not be able to lift anything heavy for several days after the procedure. Someone may need to help you around the house during this time. Ask your surgeon when you can return to work after the procedure. You may need to arrange for time off.
What will happen during insertion of an ICD:
- You may be given general anesthesia to keep you asleep and free from pain during the procedure. You may also be given a sedative and local anesthesia to numb the procedure area. With local anesthesia, you may still feel pressure or pushing during the procedure, but you should not feel any pain. Your surgeon will make an incision in your chest or abdomen. A lead will be placed into a vein near your collarbone or neck and guided into your heart. You may have multiple leads placed into your heart.
- The other end of the leads will be attached to the generator and placed in a pocket under your skin. This pocket is usually in the shoulder area, but may be in the abdominal area. The generator has a metal shell with a battery and a small computer. The computer will monitor your heart rate and rhythm. If the computer senses an irregular heartbeat, it will send electricity from the generator through the leads to your heart. These electrical shocks will make your heart beat normally.
- Your surgeon will close the incision with stitches or staples. A bandage or tape may be placed over your incision.
What the shocks from an ICD feel like:
You may not notice the low-energy shocks from your ICD, or they may feel like a flutter in your chest. The high-energy shocks are very short. They may feel like thumping or a painful kick in the chest. Your healthcare provider may give you medicine to decrease the number of high-energy shocks.
What to expect after ICD insertion:
- You will be taken to a recovery room where you will rest until you are awake.
- You will be on a heart monitor. A heart monitor is an EKG that stays on continuously to record your heart's electrical activity.
- You may need a chest x-ray to make sure the ICD is in the right place.
- You may be able to leave when you are awake and your pain is controlled. You may go to a hospital room to spend the night.
Risks of ICD insertion:
You may bleed more than expected or develop a blood clot after the procedure. You may develop an infection. The leads could poke a hole in your heart, lung, or vein. The leads may also cause arrhythmias when they are placed. Blood may collect in the pocket where the generator is placed and cause pain or an infection. The leads may disconnect or break, and you may need another procedure. You may also need another procedure to replace the entire ICD. Your ICD may not shock your heart when it needs it. It may also shock more than it should.
Call your local emergency number (911 in the US), or have someone call if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You become weak, dizzy, or faint.
- You feel your heart skip beats or beat very fast or slow, but you do not feel a shock from your ICD.
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
- You have trouble breathing.
Related medications
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- Your stitches or staples come apart.
- Blood soaks through your bandage.
- You feel more than 3 shocks in a row from your ICD.
Call your doctor or cardiologist if:
- You have a fever.
- You feel a shock from your ICD and feel fine afterward.
- Your feet or ankles swell.
- The skin around your stitches or staples is red, swollen, or draining pus or fluid.
- You have chills, a cough, and feel weak or achy.
- You are sad or anxious and find it hard to do your usual activities.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Heart medicine may be given to strengthen or control your heartbeat.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Care for yourself at home:
- Care for the insertion area as directed. Wear loose-fitting clothing over the area. Do not get the area wet until your healthcare provider says it is okay. When it is okay to bathe, do not scrub the area. Just let water run over it. Dry the area and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. Do not put powders or lotions over your incision. Check the area every day for signs of infection, such as swelling, redness, or pus.
- Do not lift anything heavier than 10 pounds, or as directed. Ask your healthcare provider when you can lift heavy objects.
- Limit the use of your arm closest to the ICD. You may be told to place your arm in a sling to keep it from moving. Wear the sling as directed. Elevate your arm when you take off your sling to reduce swelling and pain. Prop your arm on pillows or blankets to keep it elevated comfortably. Do not lift the arm over your head for as long as directed. This may be for at least 4 weeks. You may be able to start gentle range of motion (ROM) exercises after 5 days. Your healthcare provider will give you specific instructions on when you can start. ROM exercises help prevent arm and shoulder stiffness.
Check your pulse, if directed:
Check while you are resting.
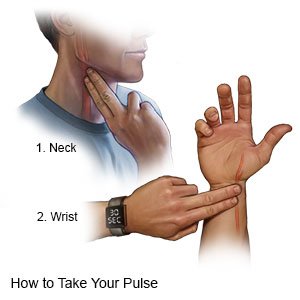 |
- Use a watch with a second hand. Count your pulse for 60 seconds.
- To check the pulse on your wrist, place your index and middle fingers on the inside of your wrist. You should feel your pulse beating just below your thumb.
- To check the pulse on your neck, place your index and middle fingers on one side of your neck. You should feel your pulse beating where your neck meets your jaw.
- Record your information. Include your pulse rate, the date, time, and which side was used to take the pulse. Include anything you notice about your pulse, such as that it is weak, strong, or missing beats. Bring a copy of the information to your follow-up visits.
Safety instructions:
Talk to your healthcare provider about driving and playing sports after you have an ICD placed. The following are instructions to keep you safe with an ICD:
- Carry an ID card for your ICD at all times. This card has important information about your ICD. Healthcare providers need to know if you have an ICD so they can keep you safe during medical procedures and tests.
- Wear medical alert jewelry or carry a card that says you have an ICD. Ask your healthcare provider where to get these items.

- Stay away from magnets or machines with electric fields. These can interfere with how your ICD works. You will get specific safety information based on the type of ICD you have. The following are general safety guidelines:
- Do not lean into a car engine or do welding.
- Do not use an electronic body fat scale or electronic abdominal stimulating exercise machine.
- Check before you have a CT scan. Some CT scan machines may be safe to use with your ICD.
- Check before you have electrolysis for hair removal. Your provider may give you instructions on how to get this procedure safely. He or she may need to give you written permission before you can get electrolysis.
- Check before you use a medical alert system, or let your company know you have an ICD. The company will be able to tell you if an ICD is safe to use with the system.
- Avoid or limit time around electric fence systems. This also includes electric systems to keep pets in a small area. If you cannot avoid it, make your time near it as short as possible.
- Keep your cell phone away from your ICD. Some cell phones may interfere with your ICD. Do not place your cell phone in a breast pocket over your ICD site. Use your cell phone with the ear on the opposite side from your ICD. Wear an arm band for your cell phone on the arm on the opposite side from your ICD.
- Keep headphones away from your ICD. Earbud and clip-on headphones have a material that can interfere with your ICD. Make sure your headphones are always at least 6 inches away from the ICD. Do not put headphones in your shirt pocket over the ICD. Do not let the headphones hang from your neck onto your chest. Do not let anyone who is using headphones put his or her head on your chest.
- Tell airport security you have an ICD. You may need to be searched by hand when you go through a security gate. The security gate or handheld wand could harm your ICD.
- Keep an ICD diary. Record when you get a shock and what you were doing before you got the shock. Keep track of how you felt before and after the shock, and how many shocks you received. Write down the day and time of each shock. Bring the diary with you when you see your healthcare provider or cardiologist.
Follow up with your doctor or cardiologist as directed:
You will need to have your ICD checked often. A type of magnet will be placed over your ICD to check it. Information will be sent to a computer about your heart rhythm, and how well your ICD is working. Your ICD battery may need to be replaced every 5 to 7 years. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Implantable Cardioverter Defibrillator
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
