Decision Aid for Breast Cancer in Women
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
What do I need to know about decisions for breast cancer?
You can work with your healthcare provider to make decisions about being screened or treated for breast cancer. Screening is a test done to find cancer early. Screening is different from diagnosis because screening is used before you first start to have signs or symptoms. This may mean management or treatment can start early. You can also help plan treatment if cancer is found or if you develop it later on.
What do I need to know about breast cancer?
- Breast cancer starts in the tissue or ducts of the breast. Breast cancer cells are able to spread to other parts of the body, such as the liver, lung, and brain.
- About 30% of cancer that is diagnosed in women is breast cancer. The average risk is about 1 in 8, or 12%.
- Some women develop breast cancer even though they have no known risk factors. The following may increase your risk:
- Older age
- A family history of breast, ovarian, prostate, or pancreatic cancer, or breast cancer 1 (BRCA1) and breast cancer 2 (BRCA2) genes
- First monthly period before age 11, or menopause that starts after age 54
- Long-term use of estrogen or progestin, or exposure to high-dose chest radiation
- Not giving birth
- First pregnancy after the age of 40, not breastfeeding, or breastfeeding for only a short time
- Extra body weight, eating large amounts of high-fat food, or lack of physical activity
- Use of cigarettes or alcohol
- The rate of death from breast cancer in women has decreased over the past 50 years. More breast cancer is being found early, and cancer treatment has improved. About 90% of women who have breast cancer are still alive 5 years after it is found and treated.
Am I a good candidate for breast cancer screening?
Screening may be helpful for you if any of the following is true:
- You are 40 to 74 years old and are at average risk for breast cancer.
- You are younger than 40 years but have a high risk for breast cancer.
- You have a family history of breast cancer or other cancers.
- You do not have another health condition that may prevent you from living longer than another 10 years.
- You want to have treatment as early as possible, if needed.
- You are willing to have screening as often as recommended by your healthcare provider.
How is screening done?
You may need more than 1 of the following:
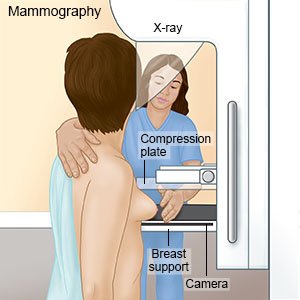
- A mammogram is a type of x-ray. Your breast will be pressed between 2 plates for a few seconds while the x-ray is taken. You and your healthcare provider will decide when and how often to get a mammogram. The timing depends on your risk factors for breast cancer. Experts recommend a mammogram every 2 years from age 40 to 74 if you are at average risk. You may need to start earlier and get a yearly mammogram if you are at high risk. Mammograms are usually done every 1 to 2 years until age 74.
- An MRI or ultrasound may be used if you are at high risk or have dense breast tissue. Do not enter the MRI room with anything metal. The MRI machine uses a powerful magnet. Metal may cause serious injury from the magnet.
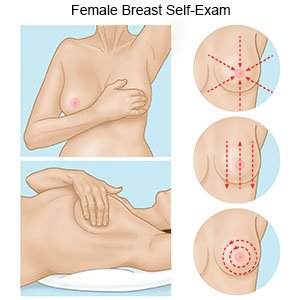
- A breast exam means your provider feels your breasts for lumps or other problems. Your provider will feel around your breasts in a circular pattern.
- A breast self-exam means you feel your breasts regularly for lumps or other changes. Your provider can give you more information on how to do a breast self-exam. You will need to do it when you are lying down and when you are standing up. A breast self-exam is not a replacement for a mammogram, MRI, or exam by your provider. You may not be able to feel small lumps.
What are the benefits and risks of screening?
Talk with your healthcare provider about the risks and benefits of screening:
- Benefits include finding breast cancer early. Cancer treatment is often more successful when it starts early. This means you can make more decisions about treatment.
- Risks include the following:
- A mammogram uses radiation that may be harmful to breast tissue. Some breast cancers may not show up on mammograms.
- The tests can give a false-negative result. This means the result looks like you do not have cancer even though you do. Treatment or monitoring may be delayed because the tests suggested you do not have cancer.
- Tests can also give a false-positive result. This means you do not actually have cancer but the test shows you do. You may get more tests, a biopsy, or even treatments that are not needed. It can also be stressful to think you have breast cancer when you do not.
Related medications
What questions should I ask my healthcare provider to help me make decisions about screening?
- How high is my risk for breast cancer?
- How often do I need to have screening?
- Where is the screening done?
- Do I need to do anything to get ready to have screening?
What happens after I have screening?
- You will meet with your healthcare provider to go over the results of your screening.
- You may need more tests to diagnose anything that showed up on the screening test.
- If cancer is found, your healthcare provider will assign a number, or stage. The stages go from 0 to 4, with 0 meaning the cells have not spread to other tissues. Stage 0 breast cancer is called in situ disease. This means it is a precancer breast disease. The stages can help you understand how quickly the cancer is likely to grow, and if it has or may spread.
- You and your healthcare provider will use the stage to talk about your treatment options. Your provider will tell you if your breast cancer is at low, medium, or high risk for growing and spreading. The need for more tests and the range of treatment options depend on the risk level. Together you and your provider can create a treatment plan that is right for you.
How is breast cancer treated, and what are the benefits of treatment?
- Watchful waiting means you do not receive treatment right away. If the cancer does not grow or spread, you may never need treatment. Watchful waiting may be used if your tumor risk is low. The benefit of this option is that you will not have invasive or difficult treatment. You can choose a different treatment option if tests show the tumor is growing or spreading over time.
- Active surveillance also means you do not receive treatment right away. You will need to have tests over time to continue to check the tumor. A benefit of this option is that follow-up tests can show a change early. Treatment options may be less invasive than if the tumor is found at a later stage.
- Hormone medicine may be used if the cancer is sensitive to hormones.
- Cryoablation is used to kill cancer cells by freezing them. This is a less invasive treatment. You may have little or no pain after this procedure.
- Radiation may be used to destroy the cancer cells.
- Chemotherapy medicines are used to kill cancer cells. You may receive one medicine or a combination of medicines. Chemotherapy may be done before or with other treatments.
- Surgery may be used to remove a lump, a small part of the breast, or the entire breast.
What are the risks of treatment?
- Watchful waiting and active surveillance can cause you to worry that the cancer is growing or spreading.
- Radiation may not kill all the cancer cells.
- Cryoablation may not kill all the cancer cells. You may develop scar tissue. You can also have swelling or pain in your chest. Tissue outside the breast may be damaged during cryoablation.
- Chemotherapy can lower your body's ability to fight infections. Some types of chemotherapy can damage heart muscle.
- Surgery can damage tissue in or around your breast. You may bleed more than expected during surgery or develop an infection. Surgery may not be able to remove all the tumor cells.
What questions should I ask my healthcare provider to help me make decisions about treatment?
- How often will I need follow-up tests if I choose active surveillance first?
- How will each treatment option affect my daily activities?
- What are the benefits and risks of having other treatments before surgery?
- Am I a good candidate for surgery?
- Which surgery may work best to treat my symptoms?
- Where is the surgery done?
- How long is recovery after surgery?
- Will my insurance cover treatment?
What do I need to think about to help me make decisions about treatment?
- If I have treatment and lose one or both breasts, how will I feel? How will this affect my self-esteem and my relationships?
- If my cancer risk is low, will I be comfortable with watchful waiting or active surveillance instead of immediate treatment? How will I feel if the cancer grows or spreads?
- Will I go in for follow-up tests over time if I do not want treatment right away?
- Am I willing to accept problems that might happen with treatment?
- How will my family or others in my life be affected by my treatment decisions?
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
