Rofecoxib Side Effects
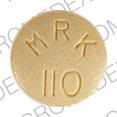
Applies to rofecoxib: oral suspension, oral tablet.
Precautions
If you will be taking this medicine for a long time, your doctor should check your progress at regular visits.
Stomach problems may be more likely to occur if you drink alcoholic beverages while being treated with this medicine. Therefore, do not regularly drink alcoholic beverages while taking this medicine, unless otherwise directed by your doctor.
Taking two or more of the nonsteroidal anti-inflammatory drugs together on a regular basis may increase the chance of unwanted effects. Also, taking acetaminophen, aspirin or other salicylates, or ketorolac (e.g., Toradol) regularly while you are taking a nonsteroidal anti-inflammatory drug may increase the chance of unwanted effects. The risk will depend on how much of each medicine you take every day, and on how long you take the medicines together. If your health care professional directs you to take these medicines together on a regular basis, follow his or her directions carefully. However, do not take acetaminophen or aspirin or other salicylates together with this medicine for more than a few days, and do not take any ketorolac (e.g., Toradol) while taking this medicine, unless your doctor has directed you to do so and is following your progress.
Serious side effects can occur during treatment with this medicine. Sometimes serious side effects can occur without warning. However, possible warning signs often occur, including severe stomach pain, black tarry stools, and/or vomiting of blood or material that looks like coffee grounds; skin rash; swelling of the face, fingers, feet, and/or lower legs. Stop taking rofecoxib and check with your doctor immediately if you notice any of these warning signs.
Rofecoxib may cause a serious type of allergic reaction called anaphylaxis. Although this is rare, it may occur often in patients who are allergic to aspirin or other nonsteroidal anti-inflammatory drugs. Anaphylaxis requires immediate medical attention. The most serious signs of this reaction are very fast or irregular breathing, gasping for breath, wheezing, or fainting. Other signs may include changes in skin color of the face; very fast but irregular heartbeat or pulse; hive-like swellings on the skin; puffiness or swellings of the eyelids or around the eyes. If these effects occur, get emergency help at once. Ask someone to drive you to the nearest hospital emergency room. Call an ambulance, lie down, cover yourself to keep warm, and prop your feet higher than your head. Stay in that position until help arrives.
Serious side effects of rofecoxib
Along with its needed effects, rofecoxib may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor as soon as possible if any of the following side effects occur while taking rofecoxib:
More common side effects
- congestion in chest
- cough
- fever
- sneezing
- sore throat
Less common or rare side effects
- bloody or black, tarry stools
- burning feeling in chest or stomach
- chills
- hives
- loss of appetite
- muscle aches and pain
- prolonged or severe vomiting
- shortness of breath
- skin rash
- tenderness in the stomach area
- unusual weight gain
- vomiting of blood or material that looks like coffee grounds
Other side effects of rofecoxib
Some side effects of rofecoxib may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- back pain
- diarrhea
- dizziness
- headache
- heartburn
- loss of energy or weakness
- nausea
- stuffy or runny nose
- swelling of legs and feet
Less common or rare side effects
- blurred vision
- constipation
See also:
For healthcare professionals
Applies to rofecoxib: oral suspension, oral tablet.
General adverse events
General side effects have included asthenia, fatigue, dizziness, influenza-like disease, lower extremity edema, sinusitis and upper respiratory infection. Other general side effects have included abscess, chest pain, chills, contusion, cyst, diaphragmatic hernia, fever, fluid retention, flushing, fungal infection, infection, laceration, pain, pelvic pain, peripheral edema, postoperative pain, syncope, trauma, upper extremity edema, viral syndrome, cerumen impaction, epistaxis, dry throat, otic pain, otitis, otitis media, pharyngitis, tinnitus, and tonsillitis.[Ref]
Gastrointestinal
Serious gastrointestinal toxicity such as bleeding, ulceration, and perforation of the stomach, small or large intestine, can occur at any time, with or without symptoms, in patients treated with nonsteroidal anti-inflammatories. The incidence of upper GI adverse events (perforations, ulcers, and bleed) was shown to be significantly lower (1.3% vs 1.8%) in patients with osteoarthritis receiving rofecoxib 12.5, 25, or 50 mg/day than in those receiving ibuprofen, diclofenac, or nabumetone. Risk factors for NSAID-induced GI bleeding include a prior history of peptic ulcer disease or gastrointestinal bleeding, treatment with oral corticosteroids, anticoagulation therapy, smoking, alcoholism, older age, poor general health status, and longer duration of NSAID therapy.
Rofecoxib (50 mg a day) has also been shown to have a lower incidence of serious upper gastrointestinal adverse events such as major bleeding, perforation, and obstruction compared to naproxen (1000 mg a day). The reduction in risk was about 50% in cumulative rates for rofecoxib (0.52%) compared to naproxen (1.22%) in the Vioxx Gastrointestinal Outcomes Research (VIGOR) study.[Ref]
Gastrointestinal side effects have included diarrhea, dyspepsia, epigastric discomfort, heartburn, and nausea. These were the most frequently reported gastrointestinal adverse events occurring in greater than 2% of patients. Other reported adverse events occurring in less than 2% of patients studied have included acid reflux, aphthous stomatitis, constipation, dental caries, dental pain, digestive gas symptoms, dry mouth, duodenal disorder, dysgeusia, esophagitis, flatulence, gastric disorder, gastritis, gastroenteritis, hematochezia, hemorrhoids, infectious gastroenteritis, oral infection, oral lesion, oral ulcer, vomiting, colitis, colonic malignant neoplasm, cholecystitis, duodenal ulcer, gastrointestinal bleeding, intestinal obstruction, and pancreatitis.
Rofecoxib 50 mg/day has been associated with a higher incidence of gastrointestinal symptoms (abdominal pain, epigastric pain, heartburn, nausea and vomiting) than that seen with either 12.5 or 25 mg/day dosage.[Ref]
Hepatic
In controlled clinical trials of rofecoxib, the incidence of borderline elevation of liver tests was comparable to the incidence observed with ibuprofen and lower than that observed with diclofenac. In placebo controlled trials, approximately 0.5% of patients taking rofecoxib and 0.1% of patients taking placebo had noticeable elevations of ALT or AST.[Ref]
Hepatic side effects have included borderline elevations of one or more liver tests that may occur in up to 15% of patients taking nonsteroidal anti-inflammatory drugs (NSAIDs). In addition, elevations of ALT or AST greater than three times normal have been reported in 1% of patients in clinical trials with NSAIDs. Patients with signs and/or symptoms of liver disease or with abnormal liver tests should be monitored carefully while on rofecoxib for evidence of worsening disease. If signs and symptoms consistent with liver disease develop, rofecoxib should be discontinued. Use of rofecoxib is not recommended in patients with severe hepatic insufficiency.[Ref]
Cardiovascular
Cardiovascular side effects have included hypertension in greater than 2% of patients. Other cardiovascular side effects have included angina pectoris, atrial fibrillation, bradycardia, hematoma, irregular heart beat, palpitation, premature ventricular contraction, tachycardia, cerebrovascular accident, congestive heart failure, deep venous thrombosis, myocardial infarction, pulmonary edema, pulmonary embolism, transient ischemic attack, unstable angina and venous insufficiency.[Ref]
The cumulative rate of serious cardiovascular thromboembolic adverse events (heart attacks, angina pectoris, and peripheral vascular events) was reported to occur in a higher percentage of patients receiving rofecoxib (1.8%) compared to patients receiving naproxen (0.6%) in the Vioxx Gastrointestinal Outcomes Research (VIGOR) study. The relationship of the cardiovascular findings to the use of rofecoxib is not known.
Patients being treated for rheumatoid arthritis with rofecoxib at a dose of 25 mg a day have been reported to have a higher incidence of hypertension compared to patients treated with naproxen at a dose of 1000 mg a day.
Lower extremity edema and hypertension have been reported to occur less often with the 12.5 and 25 mg/day dosage than with the 50 mg/day dosage.[Ref]
Ocular
Ocular side effects have included blurred vision, ocular injection and conjunctivitis.[Ref]
Metabolic
Metabolic side effects have included appetite change, hypercholesterolemia, and weight gain. Hyponatremia has been reported in less than 1% of patients.[Ref]
Renal
In two separate studies, a similar reduction in glomerular filtration rate to nonselective nonsteroidal anti-inflammatory drugs was observed.
Sudden reduction in urine output and rise in serum creatinine levels were observed in a 65-year-old woman, with a history of mild renal failure (Clcr = 57 mL/min), hyperuricemia, mitral valve regurgitation and heart failure, after receiving a single dose of rofecoxib 25 mg because of lower back pain. Over the course of her hospital stay, her renal laboratory parameters slowly returned to her baseline levels.
Acute interstitial nephritis has been reported in a 63-year-old man diagnosed with third-degree burns, on 70% of body surface area, that had been receiving for 3 weeks rofecoxib 25 mg daily for arthritis. Patient underwent one hemodialysis treatment. Creatinine and potassium levels returned to baseline levels a month later.[Ref]
Renal side effects have included a decrease in glomerular filtration rate. Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Acute renal failure after a single dose of rofecoxib has been reported. Interstitial nephritis has been diagnosed in a patient 3 weeks after the start of treatment with rofecoxib.[Ref]
Immunologic
Immunologic, nonspecific, side effects have included allergic reactions and insect bite reactions in less than 2% of patients receiving rofecoxib.[Ref]
Dermatologic
Cases of neutrophilic dermatosis have been reported to occur within one to two weeks of initiation of rofecoxib treatment for joint pains. Patients presented with multiple subcutaneous nodules over both legs, anterior and posterior areas, and areas of ulceration. The patient's leg lesions disappeared after discontinuation of rofecoxib.
A 46-year-old woman who had previously developed psoriasis after exposure to a nonselective NSAID developed a severe case of psoriasis 5 days after she started taking rofecoxib for neck strain. It took several months for symptoms to abate.[Ref]
Dermatologic side effects have included alopecia, atopic dermatitis, basal cell carcinoma, contact dermatitis, herpes simplex, herpes zoster, nail unit disorder, perspiration, pruritus, rash, skin erythema, urticaria, and xerosis. Acute onset of neutrophilic dermatosis has been reported shortly after initiation of rofecoxib therapy. A severe case of psoriasis has been reported to have developed 5 days after the start of treatment with rofecoxib.
Pseudoporphyria has been reported in a 60-year-old woman 2 weeks after the start of rofecoxib treatment for pain control. The skin lesions cleared within 1 month after discontinuation of therapy.[Ref]
Nervous system
Nervous system side effects have included headache, hypesthesia, insomnia, median nerve neuropathy, migraine, muscular spasm, paresthesia, sciatica, somnolence, and vertigo. In the postmarketing phase of rofecoxib, aseptic meningitis has been reported to the Spontaneous Reporting System of the FDA.[Ref]
Psychiatric
Psychiatric side effects have included anxiety, depression, and decreased mental acuity.[Ref]
Respiratory
Respiratory side effects have included bronchitis, asthma, cough, dyspnea, pneumonia, pulmonary congestion, laryngitis, pharyngitis, allergic rhinitis, and nasal congestion.[Ref]
Musculoskeletal
Musculoskeletal side effects have included back pain, arm pain, arthralgia, bursitis, cartilage trauma, joint swelling, muscle cramps, muscle weakness, musculoskeletal pain, musculoskeletal stiffness, myalgia, osteoarthritis, tendonitis, traumatic arthropathy, and wrist fracture.[Ref]
Genitourinary
Breast malignant neoplasm, prostate malignant neoplasm and urolithiasis have been reported in less than 0.1% of patients.[Ref]
Genitourinary side effects have included urinary tract infections, cystitis, dysuria, menopausal symptoms, menstrual disorder, nocturia, urinary retention, vaginitis, breast mass, and urolithiasis.[Ref]
Hematologic
Hematologic side effects have included reports of lymphoma in less than 0.1% of patients.[Ref]
References
1. (2001) "Product Information. Vioxx (rofecoxib)." Merck & Co., Inc
2. Laine L, Harper S, Simon T, Bath R, Johanson J, Schwartz H, Stern S, Quan H, Bolognese J (1999) "A randomized trial comparing the effect of rofecoxib, a cyclooxygenase 2-specific inhibitor, with that of ibuprofen on the gastroduodenal mucosa of patients with osteoarthritis." Gastroenterology, 117, p. 776-83
3. Langman MJ, Jensen DM, Watson DJ, et al. (1999) "Adverse upper gastrointestinal effects of rofecoxib compared with NSAIDs." JAMA, 282, p. 1929-33
4. Schnitzer TJ, Truitt K, Fleischmann R, Dalgin P, Block J, Zeng Q, Bolognese J, Seidenberg B, Ehrich EW (1999) "The safety profile, tolerability, and effective dose range of rofecoxib in the treatment of rheumatoid arthritis." Clin Ther, 21, p. 1688-702
5. Ehrich EW, Schnitzer TJ, McIlwain H, Levy R, Wolfe F, Weisman M, Zeng Q, Morrison B, Bolognese J, Seidenberg B, Gertz BJ (1999) "Effect of specific COX-2 inhibition in osteoarthritis of the knee: A 6 week double blind, placebo controlled pilot study of rofecoxib." J Rheumatol, 26, p. 2438-47
6. Cannon GW, Caldwell JR, Holt P, McLean B, Seidenberg B, Bolognese J, Ehrich E, Mukhopadhyay S, Daniels B (2000) "Rofecoxib, a specific inhibitor of cyclooxygenase 2, with clinical efficacy comparable with that of diclofenac sodium - Results of a one-year, randomized, clinical trial in patients with osteoarthritis of the knee and hip." Arthritis Rheum, 43, p. 978-87
7. Hunt RH, Bowen B, Mortensen ER, Simon TJ, James C, Cagliola A, Quan H, Bolognese JA (2000) "A randomized trial measuring fecal blood loss after treatment with rofecoxib, ibuprofen, or placebo in healthy subjects." Am J Med, 109, p. 201-6
8. Bombardier C, Laine L, Reicin A, et al. (2000) "Comparison of upper gastrointestinal toxicity of refecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group." N Engl J Med, 343, p. 1520-8
9. Caroli A, Monica F (2001) "Severe upper gastrointestinal bleeding during treatment with rofecoxib for osteoarthritis." Am J Gastroenterol, 96, p. 1663-5
10. Bombardier C (2002) "An evidence-based evaluation of the gastrointestinal safety of coxibs." Am J Cardiol, 89(6 Suppl 1), p. 3-9
11. Mamdani M, Rochon PA, Juurlink DN, et al. (2002) "Observational study of upper gastrointestinal haemorrhage in elderly patients given selective cyclo-oxygenase-2 inhibitors or conventional non-steroidal anti-inflammatory drugs." BMJ, 325, p. 624
12. Laine L, Bombardier C, Hawkey CJ, et al. (2002) "Stratifying the risk of NSAID-related upper gastrointestinal clinical events: Results of a double-blind outcomes study in patients with rheumatoid arthritis." Gastroenterology, 123, p. 1006-12
13. Gornet JM, Hassani Z, Modiglian R, Lemann M (2002) "Exacerbation of Crohn's colitis with severe colonic hemorrhage in a patient on rofecoxib." Am J Gastroenterol, 97, p. 3209-10
14. Simon LS, Smolen JS, Abramson SB, et al. (2002) "Controversies in COX-2 selective inhibition." J Rheumatol, 29, p. 1501-10
15. Hawkey CJ, Langman MJ (2003) "Non-steroidal anti-inflammatory drugs: overall risks and management. Complementary roles for COX-2 inhibitors and proton pump inhibitors." Gut, 52, p. 600-8
16. Mukherjee D, Nissen SE, Topol EJ (2001) "Risk of cardiovascular events associated with selective COX-2 inhibitors." JAMA, 286, p. 954-9
17. Reicin AS, Shapiro D, Sperling RS, Barr E, Yu Q (2002) "Comparison of cardiovascular thrombotic events in patients with osteoarthritis treated with Rofecoxib versus nonselective nonsteroidal anti-inflammatory drugs (Ibuprofen, Diclofenac, and Nabumetone)." Am J Cardiol, 89, p. 204-9
18. Ray WA, Michael Stein C, Hall K, Daugherty JR, Griffin MR (2002) "Non-steroidal anti-inflammatory drugs and risk of serious coronary heart disease: an observational cohort study." Lancet, 359, p. 118-23
19. Whelton A, White WB, Bello AE, Puma JA, Fort JG (2002) "Effects of celecoxib and rofecoxib on blood pressure and edema in patients >/=65 years of age with systemic hypertension and osteoarthritis." Am J Cardiol, 90, p. 959-63
20. Juni P, Dieppe P, Egger M (2002) "Risk of myocardial infarction associated with selective COX-2 inhibitors: questions remain." Arch Intern Med, 162, 2639-40; author reply 2640-2
21. Bannwarth B, Dougados M (2003) "Cardiovascular thrombotic events and COX-2 inhibitors: results in patients with osteoarthritis receiving rofecoxib." J Rheumatol, 30, p. 421-2
22. Whelton A (2002) "COX-2-specific inhibitors and the kidney: effect on hypertension and oedema." J Hypertens, 20 Suppl 6, S31-5
23. Gibofsky A (2002) "Clinical profiles of celecoxib and rofecoxib in the rheumatic diseases." J Hypertens, 20 Suppl 6, S25-30
24. Mamdani M, Juurlink DN, Lee DS, et al. (2004) "Cyclo-oxygenase-2 inhibitors versus non-selective non-steroidal anti-inflammatory drugs and congestive heart failure outcomes in elderly patients: a population-based cohort study." Lancet, 363, p. 1751-6
25. Wolfe F, Zhao S, Pettitt D (2004) "Blood pressure destabilization and edema among 8538 users of celecoxib, rofecoxib, and nonselective nonsteroidal antiinflammatory drugs (NSAID) and nonusers of NSAID receiving ordinary clinical care." J Rheumatol, 31, p. 1143-51
26. Levesque LE, Brophy JM, Zhang B (2005) "The risk for myocardial infarction with cyclooxygenase-2 inhibitors: a population study of elderly adults." Ann Intern Med, 142, p. 481-9
27. Graham DJ, Campen D, Hui R, et al. (2005) "Risk of acute myocardial infarction and sudden cardiac death in patients treated with cyclo-oxygenase 2 selective and non-selective non-steroidal anti-inflammatory drugs: nested case-control study." Lancet, 365, p. 475-81
28. Aw TJ, Haas SJ, Liew D, Krum H (2005) "Meta-analysis of cyclooxygenase-2 inhibitors and their effects on blood pressure." Arch Intern Med, 165, p. 490-6
29. (2005) "Summaries for patients. Risk for heart attacks with different NSAIDs." Ann Intern Med, 142, I45
30. Perazella MA, Eras J (2000) "Are selective COX-2 inhibitors nephrotoxic?." Am J Kidney Dis, 35, p. 937-40
31. Swan SK, Rudy DW, Lasseter KC, et al. (2000) "Effect of cyclooxygenase-2 inhibition on renal function in elderly persons receiving a low-salt diet." Ann Intern Med, 133, p. 1-9
32. Ofran Y, Bursztyn M, Ackerman Z (2001) "Rofecoxib-induced renal dysfunction in a patient with compensated cirrhosis and heart failure." Am J Gastroenterol, 96, p. 1941
33. Alim N, Peterson L, Zimmerman SW, Updike S (2003) "Rofecoxib-induced acute interstitial nephritis." Am J Kidney Dis, 41, p. 720-1
34. Reinhold SW, Fischereder M, Riegger GA, Kramer BK (2003) "Acute renal failure after administration of a single dose of a highly selective COX-2 inhibitor." Clin Nephrol, 60, p. 295-6
35. Smith KJ, Skelton H (2003) "Acute onset of neutrophilic dermatosis in patients after therapy with a COX-2-specific inhibitor." Int J Dermatol, 42, p. 389-93
36. Clark DW, Coulter DM (2003) "Psoriasis associated with rofecoxib." Arch Dermatol, 139, p. 1223
37. Palop-Larrea V, Melchor-Penella MA, Ortega-Monzo C, Martinez-Mir I (2003) "Leukocytoclastic vasculitis related to rofecoxib." Ann Pharmacother, 37, p. 1731-2
38. Markus R, Reddick ME, Rubenstein MC (2004) "Rofecoxib-induced pseudoporphyria." J Am Acad Dermatol, 50, p. 647-8
39. Daugherty KK, Gora-Harper ML (2002) "Idiopathic paresthesia reaction associated with rofecoxib." Ann Pharmacother, 36, p. 264-6
40. Bonnel RA, Villalba ML, Karwoski CB, Beitz J (2002) "Aseptic meningitis associated with rofecoxib." Arch Intern Med, 162, p. 713-5
41. Ashwath ML, Katner HP (2003) "Recurrent aseptic meningitis due to different non-steroidal anti-inflammatory drugs including rofecoxib." Postgrad Med J, 79, p. 295-6
42. Crofford LJ (2003) "COX-2: Where are we in 2003? - Specific cyclooxygenase-2 inhibitors and aspirin-exacerbated respiratory disease." Arthritis Res Ther, 5, p. 25-7
43. Meyer C, Gahler R (2002) "Central retinal vein occlusion in a patient with rheumatoid arthritis taking rofecoxib." Lancet, 360, p. 1100
More about rofecoxib
- Check interactions
- Compare alternatives
- Reviews (56)
- Dosage information
- During pregnancy
- Drug class: cox-2 inhibitors
Patient resources
Other brands
Related treatment guides
Further information
Rofecoxib side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.