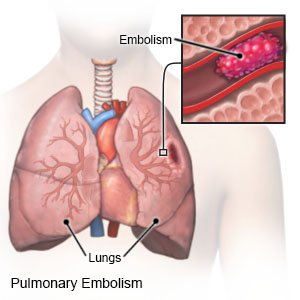
Pulmonary Embolism
Medically reviewed by Drugs.com. Last updated on Apr 6, 2025.
What is a pulmonary embolism (PE)?
A PE is the sudden blockage of a blood vessel in the lungs by an embolus. An embolus is a small piece of blood clot, fat, air, or tumor cells. The embolus cuts off the blood supply to your lungs. A PE can become life-threatening.
 |
What increases my risk for a PE?
- A deep vein thrombosis (DVT) in your leg
- Obesity
- Smoking cigarettes
- A blood disorder that makes your blood clot faster than normal, such as factor V Leiden mutation
- In women, birth control pills, especially if you are older than 35 or smoke cigarettes
- Certain blood diseases, such as cancer, thrombophilia, or hyperhomocysteinemia
- Pregnancy and childbirth
- Recent surgery
- Sitting or lying in one position for a long time, such as when you travel by plane
What are the signs and symptoms of a PE?
- Sudden shortness of breath or fast breathing
- Sudden chest pain that is worse when you take a deep breath
- A fast or irregular heartbeat
- Fever
- Coughing up blood, or coughing that does not go away
- Sweating at rest
- Bluish nails
- Cold, pale, clammy skin
- Fainting
How is a PE diagnosed?
Ask your healthcare provider about these and other tests you may need:
- Blood tests may show signs of the PE or how well your organs are working.
- An EKG test records your heart rhythm and how fast your heart beats. It is used to check for abnormal heart function.
- A chest x-ray may show signs of a lung infection or other damage.
- A CT scan may show the PE. You may be given contrast liquid to help your lungs show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
- A lung scan , or V/Q scan, may show how well blood and oxygen flow in your lungs. A small amount of contrast liquid is used to study your airflow (V) and blood flow (Q). First, you breathe in medical gas. Then, contrast liquid is injected into a vein. Pictures are taken to see how well your lungs take in oxygen.
How is a PE treated?
Treatment depends on what the embolus is made of and where the PE is located in your lung. You may need any of the following:
- Clot busters are emergency medicines that work to dissolve blood clots.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- A vena cava filter may be placed inside your vena cava to prevent another PE. The vena cava is a large vein that brings blood from your lower body up to your heart. The filter may help trap an embolus and prevent it from going into your lungs.
- Surgery called a thrombectomy may be done to remove the PE. A procedure called thrombolysis may instead be done to inject a clot buster that helps dissolve or break the clot apart.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What can I do to prevent a PE?
- Change your body position or move around often. Move and stretch in your seat several times each hour if you travel by car or work at a desk. In an airplane, get up and walk every hour.
- Exercise regularly to help increase your blood flow. Walking is a good low-impact exercise. Talk to your healthcare provider about the best exercise plan for you.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a weight loss plan, if needed.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can damage blood vessels and increase your risk for another PE. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Ask about birth control if you are a woman who takes the pill. A birth control pill increases the risk for blood clots in certain women. The risk is higher if you are also older than 35, smoke cigarettes, or have a blood clotting disorder. Talk to your healthcare provider about other ways to prevent pregnancy, such as a cervical cap or intrauterine device (IUD).
Call your local emergency number (911 in the US) if:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
When should I seek immediate care?
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
When should I call my doctor?
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Pulmonary Embolism
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
