Cor Pulmonale
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
What is cor pulmonale?
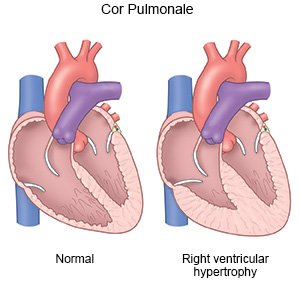
Cor pulmonale is a condition that occurs when the right ventricle of your heart cannot pump properly. The right side of your heart pumps blood from your body into your lungs to get oxygen. Cor pulmonale is caused by pulmonary hypertension (PH). PH is high blood pressure in the arteries of your lungs. Blood cannot flow through your lungs and backs up in the right ventricle of your heart. As the right ventricle tries to pump blood properly, it becomes thickened and deformed. Cor pulmonale can become life-threatening.
 |
What increases my risk for cor pulmonale?
- Acute lung diseases, such as acute respiratory distress syndrome or a blood clot in your lungs
- Chronic lung or heart disease, such as COPD or cardiomyopathy
- Conditions that decrease how much your chest expands, such as obesity or scoliosis
- Living at high altitude
- Mechanical ventilation (being on a ventilator)
- Sleep-related breathing disorders, such as obstructive sleep apnea
What are the signs and symptoms of cor pulmonale?
- Shortness of breath
- Weakness and feeling more tired than usual
- Chest pain
- Headaches
- Fainting or feeling lightheaded
- Loss of appetite
- Swelling in your abdomen, legs, and feet
How is cor pulmonale diagnosed?
Your healthcare provider will ask about your symptoms and any health problems you have. The provider will listen to your heart and lungs. The provider will check for swelling in your abdomen, ankles, and feet. You may need any of the following tests:
- An EKG checks your heart rhythm for problems, such as heart damage or disease.
- A chest x-ray is a picture of your heart and lungs. Healthcare providers use the x-ray to check the size of your heart. A chest x-ray can also show fluid around your heart and lungs.
- An echocardiogram (echo) uses sound waves to show pictures of the size and shape of your heart. An echo records how your heart moves when it is beating and how blood flows through your heart. These pictures are seen on a monitor.
- MRI or CT scan pictures may be used to check your heart and lungs. CT pictures can show conditions that may have caused cor pulmonale. MRI pictures may show the size and function of the right size of your heart. You may be given contrast liquid to help the pictures show up better. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell healthcare providers if you have any metal in or on your body.
- A VQ scan is a ventilation (V) and perfusion (Q) test. It shows the airways and blood vessels in your lungs. It will tell your healthcare provider how well your lungs are working. Radioactive liquid is put into your vein to show how blood flows in your lungs. You will then breathe in a gas. Pictures are taken to see how well your lungs breathe in oxygen.
How is cor pulmonale treated?
- Medicines:
- Diuretics are given to decrease excess fluid that collects in a part of your body, such as your legs. Diuretics can also remove excess fluid from around your heart or lungs and decrease your blood pressure. It is often called water pills. You will urinate more often when you take this medicine.
- Heart medicine may be given to strengthen or regulate your heartbeat. It also may help your heart in other ways. Talk with your healthcare provider to find out the name of your heart medicine.
- Vasodilators may improve your blood flow by making the blood vessels in your heart and lungs wider. This may decrease the pressure in your blood vessels and improve your symptoms.
- Bronchodilators are given to relax the airways in your lungs and help you breathe better.
- Blood thinners help prevent clots from forming in the blood. Blood thinners make it more likely for you to bleed or bruise. Use an electric razor and soft toothbrush to help prevent bleeding.
- Oxygen will help to decrease pressure in your lungs.
- Heart and lung transplant may be considered if other treatments do not work. Your healthcare provider will give you information if this surgery is possible.
How can I manage my cor pulmonale?
- Limit your liquids as directed. Ask your healthcare provider how much liquid you should drink each day. Too much liquid can increase your risk for swelling and make your cor pulmonale worse.
- Eat healthy foods. You may need to change what you eat to control your symptoms. Foods that are low in salt are best. Healthy foods include fruit, vegetables, whole-grain breads, low-fat dairy products, beans, lean meat, and fish.

- Maintain a healthy weight. Talk to your healthcare provider about the best plan for you. You may not be able to do certain exercises.
- Prevent pregnancy if you are a woman. During pregnancy, your heart needs to work harder than usual. Pregnancy may be life-threatening to both you and your baby. Talk with your healthcare provider about safe ways to prevent pregnancy.
- Do not drink alcohol. Alcohol can make it harder for you to breathe, and can worsen your cor pulmonale. Talk with your healthcare provider if you drink alcohol and need help to stop.
- Do not smoke. If you smoke, it is never too late to quit. Tobacco smoke can make your heart and lung symptoms worse. It can also cause heart and lung disease. Ask your healthcare provider for information if you need help to stop smoking.

Call your local emergency number (911 in the US) if:
- You cough up blood.
- You have chest pain.
- You have severe shortness of breath.
- Your hands or feet suddenly feel cold to the touch.
- Your heart is beating faster than normal for you.
When should I call my doctor?
- You are more tired than usual.
- You are urinating much less than usual.
- You feel dizzy, lightheaded, or confused.
- You have new or increased swelling in your abdomen, legs, or feet.
- You are more short of breath or wake from sleep gasping for air.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Cor Pulmonale
Treatment options
- Medications for Cor Pulmonale
- Medications for Pulmonary Arterial Hypertension
- Medications for Pulmonary Embolism
- Medications for Pulmonary Heart or Vascular Disease
- Medications for Pulmonary Thromboembolism
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
