Keppra Injection: Package Insert / Prescribing Info
Package insert / product label
Generic name: levetiracetam
Dosage form: injection, solution, concentrate
Drug class: Pyrrolidine anticonvulsants
J Code (medical billing code): J1953 (Per 10 mg, injection)
Medically reviewed by Drugs.com. Last updated on Jul 7, 2025.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
KEPPRA ®(levetiracetam) injection, for intravenous use
Initial U.S. Approval: 1999
Recent Major Changes
| Warnings and Precautions ( 5.5) | 3/2024 |
Indications and Usage for Keppra Injection
- KEPPRA is indicated for the treatment of partial-onset seizures in patients 1 month of age and older ( 1.1)
- KEPPRA is indicated for adjunctive therapy for the treatment of:
- KEPPRA injection is for intravenous use only as an alternative for patients when oral administration is temporarily not feasible ( 1.4)
Keppra Injection Dosage and Administration
KEPPRA injection is for intravenous use only ( 2.1)
Partial-Onset Seizures (monotherapy or adjunctive therapy)
- 1 Month to < 6 Months: 7 mg/kg twice daily; increase by 7 mg/kg twice daily every 2 weeks to recommended dose of 21 mg/kg twice daily ( 2.1)
- 6 Months to < 4 Years: 10 mg/kg twice daily; increase by 10 mg/kg twice daily every 2 weeks to recommended dose of 25 mg/kg twice daily ( 2.1)
- 4 Years to < 16 Years: 10 mg/kg twice daily; increase by 10 mg/kg twice daily every 2 weeks to recommended dose of 30 mg/kg twice daily ( 2.1)
- Adults 16 Years and Older: 500 mg twice daily; increase by 500 mg twice daily every 2 weeks to a recommended dose of 1500 mg twice daily ( 2.1)
Myoclonic Seizures in Adults and Pediatric Patients 12 Years and Older
- 500 mg twice daily; increase by 500 mg twice daily every 2 weeks to recommended dose of 1500 mg twice daily ( 2.2)
Primary Generalized Tonic-Clonic Seizures
- 6 Years to < 16 Years: 10 mg/kg twice daily; increase by 10 mg/kg twice daily every 2 weeks to recommended dose of 30 mg/kg twice daily ( 2.3)
- Adults 16 Years and Older: 500 mg twice daily; increase by 500 mg twice daily every 2 weeks to recommended dose of 1500 mg twice daily ( 2.3)
Switching From or To Oral KEPPRA
When switching from or to oral KEPPRA, the total daily dosage/frequency of KEPPRA injection should be equivalent to those of oral KEPPRA ( 2.4, 2.5)
See full prescribing information for preparation and administration instructions ( 2.6) and dosage adjustment in adults with renal impairment ( 2.7)
Dosage Forms and Strengths
Injection: 500 mg/5 mL single-use vial ( 3)
Contraindications
Warnings and Precautions
- Behavioral abnormalities including psychotic symptoms, suicidal ideation, irritability, and aggressive behavior have been observed; monitor patients for psychiatric signs and symptoms ( 5.1)
- Monitor for somnolence and fatigue; advise patients not to drive or operate machinery until they have sufficient experience on KEPPRA ( 5.2)
- Serious Dermatological Reactions: Discontinue KEPPRA at the first sign of rash unless clearly not drug related ( 5.4)
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity: Discontinue if no alternative etiology ( 5.5)
- Coordination Difficulties: Monitor for ataxia, abnormal gait, and incoordination ( 5.6)
- Withdrawal Seizures: KEPPRA must be gradually withdrawn ( 5.7)
Adverse Reactions/Side Effects
Most common adverse reactions (incidence ≥ 5% more than placebo) include:
- Adults: somnolence, asthenia, infection, and dizziness ( 6.1)
- Pediatric patients: fatigue, aggression, nasal congestion, decreased appetite, and irritability ( 6.1)
To report SUSPECTED ADVERSE REACTIONS, contact UCB, Inc. at (844) 599-CARE (2273) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
Pregnancy: Plasma levels of levetiracetam may be decreased; monitor closely during pregnancy. Based on animal data, may cause fetal harm ( 5.10, 8.1)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2024
Full Prescribing Information
1. Indications and Usage for Keppra Injection
1.1 Partial-Onset Seizures
KEPPRA is indicated for the treatment of partial-onset seizures in patients 1 month of age and older.
1.2 Myoclonic Seizures in Patients with Juvenile Myoclonic Epilepsy
KEPPRA is indicated as adjunctive therapy for the treatment of myoclonic seizures in patients 12 years of age and older with juvenile myoclonic epilepsy.
2. Keppra Injection Dosage and Administration
2.1 Dosing for Partial-Onset Seizures
The recommended dosing for monotherapy and adjunctive therapy is the same as outlined below.
There is no clinical study experience with administration of intravenous levetiracetam for a period longer than 4 days.
Adults 16 Years of Age and Older
Initiate treatment with a daily dose of 1000 mg/day, given as twice-daily dosing (500 mg twice daily). Additional dosing increments may be given (1000 mg/day additional every 2 weeks) to a maximum recommended daily dose of 3000 mg. There is no evidence that doses greater than 3000 mg/day confer additional benefit.
Pediatric Patients
1 Month to < 6 Months
Initiate treatment with a daily dose of 14 mg/kg in 2 divided doses (7 mg/kg twice daily). Increase the daily dose every 2 weeks by increments of 14 mg/kg to the recommended daily dose of 42 mg/kg (21 mg/kg twice daily). In the clinical trial, the mean daily dose was 35 mg/kg in this age group.
6 Months to < 4 Years
Initiate treatment with a daily dose of 20 mg/kg in 2 divided doses (10 mg/kg twice daily). Increase the daily dose in 2 weeks by an increment of 20 mg/kg to the recommended daily dose of 50 mg/kg (25 mg/kg twice daily). If a patient cannot tolerate a daily dose of 50 mg/kg, the daily dose may be reduced. In the clinical trial, the mean daily dose was 47 mg/kg in this age group.
4 Years to < 16 Years
Initiate treatment with a daily dose of 20 mg/kg in 2 divided doses (10 mg/kg twice daily). Increase the daily dose every 2 weeks by increments of 20 mg/kg to the recommended daily dose of 60 mg/kg (30 mg/kg twice daily). If a patient cannot tolerate a daily dose of 60 mg/kg, the daily dose may be reduced. In the clinical trial, the mean daily dose was 44 mg/kg. The maximum daily dose was 3000 mg/day.
2.2 Dosing for Myoclonic Seizures in Patients with Juvenile Myoclonic Epilepsy
Initiate treatment with a dose of 1000 mg/day, given as twice-daily dosing (500 mg twice daily). Increase the dosage by 1000 mg/day every 2 weeks to the recommended daily dose of 3000 mg. The effectiveness of doses lower than 3000 mg/day has not been studied.
2.3 Dosing for Primary Generalized Tonic-Clonic Seizures
Adults 16 Years of Age and Older
Initiate treatment with a dose of 1000 mg/day, given as twice-daily dosing (500 mg twice daily). Increase dosage by 1000 mg/day every 2 weeks to the recommended daily dose of 3000 mg. The effectiveness of doses lower than 3000 mg/day has not been adequately studied.
Pediatric Patients 6 to <16 Years of Age
Initiate treatment with a daily dose of 20 mg/kg in 2 divided doses (10 mg/kg twice daily). Increase the daily dose every 2 weeks by increments of 20 mg/kg (10 mg/kg twice daily) to the recommended daily dose of 60 mg/kg (30 mg/kg twice daily). The effectiveness of doses lower than 60 mg/kg/day has not been adequately studied.
2.4 Switching from Oral Dosing
When switching from oral KEPPRA, the initial total daily intravenous dosage of KEPPRA should be equivalent to the total daily dosage and frequency of oral KEPPRA.
2.5 Switching to Oral Dosing
At the end of the intravenous treatment period, the patient may be switched to KEPPRA oral administration at the equivalent daily dosage and frequency of the intravenous administration.
2.6 Preparation and Administration Instructions
KEPPRA injection is for intravenous use only and should be diluted in 100 mL of a compatible diluent prior to administration. If a smaller volume is required (e.g. pediatric patients), the amount of diluent should be calculated to not exceed a maximum levetiracetam concentration of 15 mg per mL of diluted solution. Consideration should also be given to the total daily fluid intake of the patient. KEPPRA injection should be administered as a 15-minute IV infusion. One vial of KEPPRA injection contains 500 mg levetiracetam (500 mg/5 mL).
KEPPRA injection may be mixed with the following diluents and antiepileptic drugs and may be stored in polyvinyl chloride (PVC) bags. The diluted solution should not be stored for more than 4 hours at controlled room temperature [15-30°C (59-86°F)].
Diluents:
Sodium chloride (0.9%) injection, USP
Lactated Ringer's injection
Dextrose 5% injection, USP
Other Antiepileptic Drugs:
Lorazepam
Diazepam
Valproate sodium
There are no data to support the physical compatibility of KEPPRA injection with antiepileptic drugs that are not listed above.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Product with particulate matter or discoloration should not be used.
Any unused portion of the KEPPRA injection vial contents should be discarded.
Adults
See Table 1for the recommended preparation and administration of KEPPRA injection for adults to achieve a dose of 500 mg, 1000 mg, or 1500 mg.
| Dose | Withdraw Volume | Volume of Diluent | Infusion Time |
|---|---|---|---|
| 500 mg | 5 mL (5 mL vial) | 100 mL | 15 minutes |
| 1000 mg | 10 mL (two 5 mL vials) | 100 mL | 15 minutes |
| 1500 mg | 15 mL (three 5 mL vials) | 100 mL | 15 minutes |
For example, to prepare a 1000 mg dose, dilute 10 mL of KEPPRA injection in 100 mL of a compatible diluent and administer intravenously as a 15-minute infusion.
Pediatric Patients
When using KEPPRA injection for pediatric patients, dosing is weight-based (mg per kg).
The following calculation should be used to determine the appropriate daily dose of KEPPRA injection for pediatric patients:
| Total daily dose (mL/day) = | Daily dose (mg/kg/day) × patient weight (kg)
------------------------------------------------ |
| 100 mg/mL |
2.7 Dosage Adjustments in Adult Patients with Renal Impairment
KEPPRA dosing must be individualized according to the patient's renal function status. Recommended dosage adjustments for adults with renal impairment are shown in Table 2. Information is unavailable for dosage adjustments in pediatric patients with renal impairment. In order to calculate the dose recommended for adult patients with renal impairment, creatinine clearance adjusted for body surface area must be calculated. To do this an estimate of the patient's creatinine clearance (CLcr) in mL/min must first be calculated using the following formula:
| CLcr= | [140-age (years)] × weight (kg)
----------------------------------- 72 × serum creatinine (mg/dL) | (× 0.85 for female patients) |
Then CLcr is adjusted for body surface area (BSA) as follows:
| CLcr (mL/min/1.73m 2)= | CLcr (mL/min)
---------------------------× 1.73 BSA subject (m 2) |
| Group | Creatinine Clearance
(mL/min/1.73m 2) | Dosage
(mg) | Frequency |
|---|---|---|---|
|
|||
| Normal | > 80 | 500 to 1,500 | Every 12 hours |
| Mild | 50 – 80 | 500 to 1,000 | Every 12 hours |
| Moderate | 30 – 50 | 250 to 750 | Every 12 hours |
| Severe | < 30 | 250 to 500 | Every 12 hours |
| ESRD patients using dialysis | ------- | 500 to 1,000 * | Every 24 hours * |
2.8 Discontinuation of KEPPRA
Avoid abrupt withdrawal from KEPPRA in order to reduce the risk of increased seizure frequency and status epilepticus [see Warnings and Precautions (5.7)] .
3. Dosage Forms and Strengths
One vial of KEPPRA injection contains 500 mg levetiracetam (500 mg/5 mL) as a clear, colorless solution.
4. Contraindications
KEPPRA is contraindicated in patients with a hypersensitivity to levetiracetam .Reactions have included anaphylaxis and angioedema [see Warnings and Precautions (5.3)] .
5. Warnings and Precautions
5.1 Behavioral Abnormalities and Psychotic Symptoms
KEPPRA may cause behavioral abnormalities and psychotic symptoms. Patients treated with KEPPRA should be monitored for psychiatric signs and symptoms.
Behavioral abnormalities
In clinical studies using an oral formulation of KEPPRA, 13% of adult KEPPRA-treated patients and 38% of pediatric KEPPRA-treated patients (4 to 16 years of age), compared to 6% and 19% of adult and pediatric placebo-treated patients, experienced non-psychotic behavioral symptoms (reported as aggression, agitation, anger, anxiety, apathy, depersonalization, depression, emotional lability, hostility, hyperkinesias, irritability, nervousness, neurosis, and personality disorder).
A randomized, double-blind, placebo-controlled study was performed to assess the neurocognitive and behavioral effects of an oral formulation of KEPPRA as adjunctive therapy in pediatric patients (4 to 16 years of age). The results from an exploratory analysis indicated a worsening in KEPPRA-treated patients on aggressive behavior (one of eight behavior dimensions), as measured in a standardized and systematic way using a validated instrument, the Achenbach Child Behavior Checklist (CBCL/6-18).
In clinical studies in pediatric patients 1 month to < 4 years of age, irritability was reported in 12% of the KEPPRA-treated patients compared to 0% of placebo-treated patients.
In clinical studies, 1.7% of adult KEPPRA-treated patients discontinued treatment due to behavioral adverse reactions, compared to 0.2% of placebo-treated patients. The treatment dose was reduced in 0.8% of adult KEPPRA-treated patients and in 0.5% of placebo-treated patients. Overall, 11% of KEPPRA-treated pediatric patients experienced behavioral symptoms associated with discontinuation or dose reduction, compared to 6% of placebo-treated patients.
Psychotic symptoms
In clinical studies using an oral formulation of KEPPRA, 1% of KEPPRA-treated adult patients, 2% of KEPPRA-treated pediatric patients 4 to 16 years of age, and 17% of KEPPRA-treated pediatric patients 1 month to <4 years of age experienced psychotic symptoms, compared to 0.2%, 2%, and 5% in the corresponding age groups treated with placebo. In a controlled study that assessed the neurocognitive and behavioral effects of an oral formulation of KEPPRA in pediatric patients 4 to 16 years of age, 1.6% of KEPPRA-treated patients experienced paranoia, compared to 0% of placebo-treated patients. In the same study, 3.1% of KEPPRA-treated patients experienced confusional state, compared to 0% of placebo-treated patients [see Use in Specific Populations (8.4)] .
In clinical studies, two (0.3%) KEPPRA-treated adult patients were hospitalized, and their treatment was discontinued due to psychosis. Both events, reported as psychosis, developed within the first week of treatment and resolved within 1 to 2 weeks following treatment discontinuation. There was no difference between drug- and placebo-treated patients in the incidence of the pediatric patients who discontinued treatment due to psychotic and non-psychotic adverse reactions.
5.2 Somnolence and Fatigue
KEPPRA may cause somnolence and fatigue. Patients should be monitored for somnolence and fatigue, and be advised not to drive or operate machinery until they have gained sufficient experience on KEPPRA to gauge whether it adversely affects their ability to drive or operate machinery.
Somnolence
In controlled clinical studies using an oral formulation of KEPPRA in adult patients with partial-onset seizures, 15% of KEPPRA-treated patients reported somnolence, compared to 8% of placebo-treated patients. There was no clear dose response up to 3000 mg/day. In a study in which there was no titration, about 45% of patients receiving KEPPRA 4000 mg/day reported somnolence. The somnolence was considered serious in 0.3% of KEPPRA-treated patients, compared to 0% in the placebo group. About 3% of KEPPRA-treated patients discontinued treatment due to somnolence, compared to 0.7% of placebo-treated patients. In 1.4% of KEPPRA-treated patients and 0.9% of placebo-treated patients, the dose was reduced, while 0.3% of the KEPPRA-treated patients were hospitalized due to somnolence.
Asthenia
In controlled clinical studies using an oral formulation of KEPPRA in adult patients with partial-onset seizures, 15% of KEPPRA-treated patients reported asthenia, compared to 9% of placebo-treated patients. Treatment was discontinued due to asthenia in 0.8% of KEPPRA-treated patients as compared to 0.5% of placebo-treated patients. In 0.5% of KEPPRA-treated patients and in 0.2% of placebo-treated patients, the dose was reduced due to asthenia.
Somnolence and asthenia occurred most frequently within the first 4 weeks of treatment. In general, the incidences of somnolence and fatigue in the pediatric partial-onset seizure studies, and in pediatric and adult myoclonic and primary generalized tonic-clonic studies were comparable to those of the adult partial-onset seizure studies.
5.3 Anaphylaxis and Angioedema
KEPPRA can cause anaphylaxis or angioedema after the first dose or at any time during treatment. Signs and symptoms in cases reported in the postmarketing setting have included hypotension, hives, rash, respiratory distress, and swelling of the face, lip, mouth, eye, tongue, throat, and feet. In some reported cases, reactions were life-threatening and required emergency treatment. If a patient develops signs or symptoms of anaphylaxis or angioedema, KEPPRA should be discontinued and the patient should seek immediate medical attention. KEPPRA should be discontinued permanently if a clear alternative etiology for the reaction cannot be established [see Contraindications (4)] .
5.4 Serious Dermatological Reactions
Serious dermatological reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported in both pediatric and adult patients treated with KEPPRA. The median time of onset is reported to be 14 to 17 days, but cases have been reported at least four months after initiation of treatment. Recurrence of the serious skin reactions following rechallenge with KEPPRA has also been reported. KEPPRA should be discontinued at the first sign of a rash, unless the rash is clearly not drug-related. If signs or symptoms suggest SJS/TEN, use of this drug should not be resumed and alternative therapy should be considered.
5.5 Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity
Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), also known as multiorgan hypersensitivity, has been reported in patients taking antiepileptic drugs, including KEPPRA. These events can be fatal or life-threatening, particularly if diagnosis and treatment do not occur as early as possible. DRESS typically, although not exclusively, presents with fever, rash, lymphadenopathy, and/or facial swelling, in association with other organ system involvement, such as hepatitis, nephritis, hematological abnormalities, myocarditis, or myositis, sometimes resembling an acute viral infection. Eosinophilia is often present. Because this disorder is variable in its expression, other organ systems not noted here may be involved. It is important to note that early manifestations of hypersensitivity, such as fever or lymphadenopathy, may be present even though rash is not evident. If such signs or symptoms are present, the patient should be evaluated immediately. KEPPRA should be discontinued if an alternative etiology for the signs or symptoms cannot be established [see Contraindications (4)] .
5.6 Coordination Difficulties
KEPPRA may cause coordination difficulties.
In controlled clinical studies using an oral formulation of KEPPRA in adult patients with partial-onset seizures, 3.4% of KEPPRA-treated patients experienced coordination difficulties, (reported as ataxia, abnormal gait, or incoordination) compared to 1.6% of placebo-treated patients. A total of 0.4% of patients in controlled clinical studies discontinued KEPPRA treatment due to ataxia, compared to 0% of placebo-treated patients. In 0.7% of KEPPRA-treated patients and in 0.2% of placebo-treated patients, the dose was reduced due to coordination difficulties, while one of the treated patients was hospitalized due to worsening of pre-existing ataxia. These events occurred most frequently within the first 4 weeks of treatment.
Patients should be monitored for signs and symptoms of coordination difficulties and advised not to drive or operate machinery until they have gained sufficient experience on KEPPRA to gauge whether it could adversely affect their ability to drive or operate machinery.
5.7 Withdrawal Seizures
As with most antiepileptic drugs, KEPPRA should generally be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus. But if withdrawal is needed because of a serious adverse reaction, rapid discontinuation can be considered.
5.8 Hematologic Abnormalities
KEPPRA can cause hematologic abnormalities. Hematologic abnormalities occurred in clinical trials and included decreases in white blood cell (WBC), neutrophil, and red blood cells counts (RBC); decreases in hemoglobin and hematocrit; and increases in eosinophil counts. Cases of agranulocytosis, pancytopenia, and thrombocytopenia have been reported in the postmarketing setting. A complete blood count is recommended in patients experiencing significant weakness, pyrexia, recurrent infections, or coagulation disorders.
Partial-Onset Seizures
Adults
In controlled clinical studies using an oral formulation of KEPPRA in adult patients with partial-onset seizures, minor but statistically significant decreases compared to placebo in total mean RBC (0.03 × 10 6/mm 3), mean hemoglobin (0.09 g/dL), and mean hematocrit (0.38%), were seen in KEPPRA-treated patients.
A total of 3.2% of KEPPRA-treated and 1.8% of placebo-treated patients had at least one possibly significant (≤2.8 × 10 9/L) decreased WBC, and 2.4% of KEPPRA-treated and 1.4% of placebo-treated patients had at least one possibly significant (≤1.0 × 10 9/L) decreased neutrophil count. Of the KEPPRA-treated patients with a low neutrophil count, all but one rose towards or to baseline with continued treatment. No patient was discontinued secondary to low neutrophil counts.
Pediatric Patients 4 Years to < 16 Years
In a controlled study in pediatric patients age 4 years to <16 years, statistically significant decreases in WBC and neutrophil counts were seen in KEPPRA-treated patients, as compared to placebo. The mean decreases from baseline in the KEPPRA-treated group were -0.4 × 10 9/L and -0.3 × 10 9/L, respectively, whereas there were small increases in the placebo group. Mean relative lymphocyte counts increased by 1.7% in KEPPRA-treated patients, compared to a decrease of 4% in placebo-treated patients (statistically significant).
More KEPPRA-treated patients had a possibly clinically significant abnormally low WBC value (3% of KEPPRA-treated patients versus 0% of placebo-treated patients); however, there was no apparent difference between treatment groups with respect to neutrophil count (5% on KEPPRA versus 4.2% on placebo). No patient was discontinued because of low WBC or neutrophil count.
In a randomized, double-blind, placebo-controlled study to assess the neurocognitive and behavioral effects of an oral formulation of KEPPRA as adjunctive therapy in pediatric patients (4 to 16 years of age), 5 patients (8.6%) in the KEPPRA-treated group and two patients (6.1%) in the placebo-treated group had high eosinophil count values that were possibly clinically significant (≥10% or ≥0.7 × 10 9/L).
5.9 Increase in Blood Pressure
In a randomized, placebo-controlled study in patients 1 month to <4 years of age using an oral formulation of KEPPRA, a significantly higher risk of increased diastolic blood pressure was observed in the KEPPRA-treated patients (17%), compared to placebo-treated patients (2%). There was no overall difference in mean diastolic blood pressure between the treatment groups. This disparity between the KEPPRA and placebo treatment groups was not observed in the studies of older children or in adults.
Monitor patients 1 month to <4 years of age for increases in diastolic blood pressure.
5.10 Seizure Control During Pregnancy
Physiological changes may gradually decrease plasma levels of levetiracetam throughout pregnancy. This decrease is more pronounced during the third trimester. It is recommended that patients be monitored carefully during pregnancy. Close monitoring should continue through the postpartum period especially if the dose was changed during pregnancy.
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed in more details in other sections of labeling:
- Behavioral Abnormalities and Psychotic Symptoms [see Warnings and Precautions (5.1)]
- Somnolence and Fatigue [see Warnings and Precautions (5.2)]
- Anaphylaxis and Angioedema [see Warnings and Precautions (5.3)]
- Serious Dermatological Reactions [see Warnings and Precautions (5.4)]
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity [see Warnings and Precautions (5.5)]
- Coordination Difficulties [see Warnings and Precautions (5.6)]
- Hematologic Abnormalities [see Warnings and Precautions (5.8)]
- Increase in Blood Pressure [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The adverse reactions that result from KEPPRA injection use include all of those reported for KEPPRA tablets and oral solution. Equivalent doses of intravenous (IV) levetiracetam and oral levetiracetam result in equivalent C max, C min, and total systemic exposure to levetiracetam when the IV levetiracetam is administered as a 15-minute infusion.
Partial-Onset Seizures
Adults
In controlled clinical studies using KEPPRA tablets in adults with partial-onset seizures [see Clinical Studies (14.1)], the most common adverse reactions in adult patients receiving KEPPRA in combination with other AEDs, for events with rates greater than placebo, were somnolence, asthenia, infection, and dizziness. Of the most common adverse reactions in adults experiencing partial-onset seizures, asthenia, somnolence, and dizziness occurred predominantly during the first 4 weeks of treatment with KEPPRA.
Table 3 lists adverse reactions that occurred in at least 1% of adult epilepsy patients receiving KEPPRA tablets in placebo-controlled studies and were numerically more common than in patients treated with placebo. In these studies, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA
(N=769) % | Placebo
(N=439) % |
|
|---|---|---|
|
||
| Asthenia | 15 | 9 |
| Somnolence | 15 | 8 |
| Headache | 14 | 13 |
| Infection | 13 | 8 |
| Dizziness | 9 | 4 |
| Pain | 7 | 6 |
| Pharyngitis | 6 | 4 |
| Depression | 4 | 2 |
| Nervousness | 4 | 2 |
| Rhinitis | 4 | 3 |
| Anorexia | 3 | 2 |
| Ataxia | 3 | 1 |
| Vertigo | 3 | 1 |
| Amnesia | 2 | 1 |
| Anxiety | 2 | 1 |
| Cough Increased | 2 | 1 |
| Diplopia | 2 | 1 |
| Emotional Lability | 2 | 0 |
| Hostility | 2 | 1 |
| Paresthesia | 2 | 1 |
| Sinusitis | 2 | 1 |
In controlled adult clinical studies using KEPPRA tablets, 15% of patients receiving KEPPRA and 12% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. Table 4 lists the most common (>1%) adverse reactions that resulted in discontinuation or dose reduction and that occurred more frequently in KEPPRA-treated patients than in placebo-treated patients.
| Adverse Reaction | KEPPRA
(N=769) % | Placebo
(N=439) % |
|---|---|---|
| Somnolence | 4 | 2 |
| Dizziness | 1 | 0 |
Pediatric Patients 4 Years to <16 Years
The adverse reaction data presented below was obtained from a pooled analysis of two controlled pediatric clinical studies using an oral formulation in pediatric patients 4 to 16 years of age with partial-onset seizures. The most common adverse reactions in pediatric patients receiving KEPPRA in combination with other AEDs, for events with rates greater than placebo, were fatigue, aggression, nasal congestion, decreased appetite, and irritability.
Table 5 lists adverse reactions from the pooled pediatric controlled studies (4 to 16 years of age) that occurred in at least 2% of pediatric KEPPRA-treated patients and were numerically more common than in pediatric patients treated with placebo. In these studies, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA
(N=165) % | Placebo
(N=131) % |
|
|---|---|---|
|
||
| Headache | 19 | 15 |
| Nasopharyngitis | 15 | 12 |
| Vomiting | 15 | 12 |
| Somnolence | 13 | 9 |
| Fatigue | 11 | 5 |
| Aggression | 10 | 5 |
| Upper Abdominal Pain | 9 | 8 |
| Cough | 9 | 5 |
| Nasal Congestion | 9 | 2 |
| Decreased Appetite | 8 | 2 |
| Abnormal Behavior | 7 | 4 |
| Dizziness | 7 | 5 |
| Irritability | 7 | 1 |
| Pharyngolaryngeal Pain | 7 | 4 |
| Diarrhea | 6 | 2 |
| Lethargy | 6 | 5 |
| Insomnia | 5 | 3 |
| Agitation | 4 | 1 |
| Anorexia | 4 | 3 |
| Head Injury | 4 | 0 |
| Constipation | 3 | 1 |
| Contusion | 3 | 1 |
| Depression | 3 | 1 |
| Fall | 3 | 2 |
| Influenza | 3 | 1 |
| Mood Altered | 3 | 1 |
| Affect Lability | 2 | 1 |
| Anxiety | 2 | 1 |
| Arthralgia | 2 | 0 |
| Confusional State | 2 | 0 |
| Conjunctivitis | 2 | 0 |
| Ear Pain | 2 | 1 |
| Gastroenteritis | 2 | 0 |
| Joint Sprain | 2 | 1 |
| Mood Swings | 2 | 1 |
| Neck Pain | 2 | 1 |
| Rhinitis | 2 | 0 |
| Sedation | 2 | 1 |
In the controlled pooled pediatric clinical studies in patients 4-16 years of age, 7% of patients receiving KEPPRA and 9% receiving placebo discontinued as a result of an adverse reaction.
Pediatric Patients 1 Month to < 4 Years
In the 7-day controlled pediatric clinical study using an oral formulation of KEPPRA in children 1 month to less than 4 years of age with partial-onset seizures, the most common adverse reactions in patients receiving KEPPRA in combination with other AEDs, for events with rates greater than placebo, were somnolence and irritability. Because of the shorter exposure period, incidences of adverse reactions are expected to be lower than in other pediatric studies in older patients. Therefore, other controlled pediatric data, presented above, should also be considered to apply to this age group.
Table 6 lists adverse reactions that occurred in at least 5% of pediatric epilepsy patients (ages 1 month to < 4 years) treated with KEPPRA in the placebo-controlled study and were numerically more common than in patients treated with placebo. In this study, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA
(N=60) % | Placebo
(N=56) % |
|
|---|---|---|
|
||
| Somnolence | 13 | 2 |
| Irritability | 12 | 0 |
In the 7-day controlled pediatric clinical study in patients 1 month to < 4 years of age, 3% of patients receiving KEPPRA and 2% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. There was no adverse reaction that resulted in discontinuation for more than one patient.
Myoclonic Seizures
Although the pattern of adverse reactions in this study seems somewhat different from that seen in patients with partial-onset seizures, this is likely due to the much smaller number of patients in this study compared to partial seizure studies. The adverse reaction pattern for patients with JME is expected to be essentially the same as for patients with partial seizures.
In the controlled clinical study using KEPPRA tablets in patients with myoclonic seizures [see Clinical Studies (14.2)] , the most common adverse reactions in patients receiving KEPPRA in combination with other AEDs, for events with rates greater than placebo, were somnolence, neck pain, and pharyngitis.
Table 7 lists adverse reactions that occurred in at least 5% of juvenile myoclonic epilepsy patients experiencing myoclonic seizures treated with KEPPRA tablets and were numerically more common than in patients treated with placebo. In this study, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA
(N=60) % | Placebo
(N=60) % |
|
|---|---|---|
|
||
| Somnolence | 12 | 2 |
| Neck pain | 8 | 2 |
| Pharyngitis | 7 | 0 |
| Depression | 5 | 2 |
| Influenza | 5 | 2 |
| Vertigo | 5 | 3 |
In the placebo-controlled study using KEPPRA tablets in patients with JME, 8% of patients receiving KEPPRA and 2% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. The adverse reactions that led to discontinuation or dose reduction and that occurred more frequently in KEPPRA-treated patients than in placebo-treated patients are presented in Table 8.
| Adverse Reaction | KEPPRA
(N=60) % | Placebo
(N=60) % |
|---|---|---|
| Anxiety | 3 | 2 |
| Depressed mood | 2 | 0 |
| Depression | 2 | 0 |
| Diplopia | 2 | 0 |
| Hypersomnia | 2 | 0 |
| Insomnia | 2 | 0 |
| Irritability | 2 | 0 |
| Nervousness | 2 | 0 |
| Somnolence | 2 | 0 |
Primary Generalized Tonic-Clonic Seizures
Although the pattern of adverse reactions in this study seems somewhat different from that seen in patients with partial seizures, this is likely due to the much smaller number of patients in this study compared to partial seizure studies. The adverse reaction pattern for patients with primary generalized tonic-clonic (PGTC) seizures is expected to be essentially the same as for patients with partial seizures.
In the controlled clinical study that included patients 4 years of age and older with PGTC seizures, the most common adverse reaction in patients receiving KEPPRA oral formulation in combination with other AEDs, for events with rates greater than placebo was nasopharyngitis.
Table 9 lists adverse reactions that occurred in at least 5% of idiopathic generalized epilepsy patients experiencing PGTC seizures treated with KEPPRA and were numerically more common than in patients treated with placebo. In this study, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA
(N=79) % | Placebo
(N=84) % |
|
|---|---|---|
|
||
| Nasopharyngitis | 14 | 5 |
| Fatigue | 10 | 8 |
| Diarrhea | 8 | 7 |
| Irritability | 6 | 2 |
| Mood swings | 5 | 1 |
In the placebo-controlled study, 5% of patients receiving KEPPRA and 8% receiving placebo either discontinued or had a dose reduction during the treatment period as a result of an adverse reaction.
This study was too small to adequately characterize the adverse reactions that could be expected to result in discontinuation of treatment in this population. It is expected that the adverse reactions that would lead to discontinuation in this population would be similar to those resulting in discontinuation in other epilepsy trials (see tables 4and 8).
In addition, the following adverse reactions were seen in other controlled adult studies of KEPPRA: balance disorder, disturbance in attention, eczema, memory impairment, myalgia, and blurred vision.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of KEPPRA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been reported in patients receiving KEPPRA worldwide. The listing is alphabetized: abnormal liver function test, acute kidney injury, anaphylaxis, angioedema, agranulocytosis, choreoathetosis, drug reaction with eosinophilia and systemic symptoms (DRESS), dyskinesia, erythema multiforme, hepatic failure, hepatitis, hyponatremia, muscular weakness, obsessive-compulsive disorders (OCD), pancreatitis, pancytopenia (with bone marrow suppression identified in some of these cases), panic attack, thrombocytopenia, weight loss, and worsening of seizures including in patients with SCN8A mutations. Alopecia has been reported with KEPPRA use; recovery was observed in majority of cases where KEPPRA was discontinued.
Related/similar drugs
8. Use In Specific Populations
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to antiepileptic drugs (AEDs), including KEPPRA, during pregnancy. Encourage women who are taking KEPPRA during pregnancy to enroll in the North American Antiepileptic Drug (NAAED) pregnancy registry by calling 1-888-233-2334 or visiting http://www.aedpregnancyregistry.org/.
Risk Summary
Prolonged experience with KEPPRA in pregnant women has not identified a drug-associated risk of major birth defects or miscarriage, based on published literature, which includes data from pregnancy registries, and reflects experience over two decades [see Human Data] . In animal studies, levetiracetam produced developmental toxicity (increased embryofetal and offspring mortality, increased incidences of fetal structural abnormalities, decreased embryofetal and offspring growth, neurobehavioral alterations in offspring) at doses similar to human therapeutic doses [see Animal Data] .
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown.
Clinical Considerations
Levetiracetam blood levels may decrease during pregnancy [see Warnings and Precautions (5.10)].
Physiological changes during pregnancy may affect levetiracetam concentration. Decrease in levetiracetam plasma concentrations has been observed during pregnancy. This decrease is more pronounced during the third trimester. Dose adjustments may be necessary to maintain clinical response.
Data
Human Data
While available studies cannot definitively establish the absence of risk, data from the published literature and pregnancy registries have not established an association with levetiracetam use during pregnancy and major birth defects or miscarriage.
Animal Data
When levetiracetam (0, 400, 1200, or 3600 mg/kg/day) was administered orally to pregnant rats during the period of organogenesis, reduced fetal weights and increased incidence of fetal skeletal variations were observed at the highest dose tested. There was no evidence of maternal toxicity. The no-effect dose for adverse effects on embryofetal developmental in rats (1200 mg/kg/day) is approximately 4 times the maximum recommended human dose (MRHD) of 3000 mg on a body surface area (mg/m 2) basis.
Oral administration of levetiracetam (0, 200, 600, or 1800 mg/kg/day) to pregnant rabbits during the period of organogenesis resulted in increased embryofetal mortality and incidence of fetal skeletal variations at the mid and high dose and decreased fetal weights and increased incidence of fetal malformations at the high dose, which was associated with maternal toxicity. The no-effect dose for adverse effects on embryofetal development in rabbits (200 mg/kg/day) is approximately equivalent to the MRHD on a mg/m2 basis.
Oral administration of levetiracetam (0, 70, 350, or 1800 mg/kg/day) to female rats throughout pregnancy and lactation led to an increased incidence of fetal skeletal variations, reduced fetal body weight, and decreased growth in offspring at the mid and high doses and increased pup mortality and neurobehavioral alterations in offspring at the highest dose tested. There was no evidence of maternal toxicity. The no-effect dose for adverse effects on pre- and postnatal development in rats (70 mg/kg/day) is less than the MRHD on a mg/m2 basis.
Oral administration of levetiracetam to rats during the latter part of gestation and throughout lactation produced no adverse developmental or maternal effects at doses of up to 1800 mg/kg/day (6 times the MRHD on a mg/m2 basis).
8.2 Lactation
Risk Summary
Levetiracetam is excreted in human milk. There are no data on the effects of KEPPRA on the breastfed infant, or the effects on milk production.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for KEPPRA and any potential adverse effects on the breastfed infant from KEPPRA or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of KEPPRA for the treatment of partial-onset seizures in patients 1 month to 16 years of age have been established [see Clinical Pharmacology (12.3)and Clinical Studies (14.1)] . The dosing recommendation in these pediatric patients varies according to age group and is weight-based [see Dosage and Administration (2.6)] .
The safety and effectiveness of KEPPRA as adjunctive therapy for the treatment of myoclonic seizures in adolescents 12 years of age and older with juvenile myoclonic epilepsy have been established [see Clinical Studies (14.2)] .
The safety and effectiveness of KEPPRA as adjunctive therapy for the treatment of primary generalized tonic-clonic seizures in pediatric patients 6 years of age and older with idiopathic generalized epilepsy have been established [see Clinical Studies (14.3)] .
Safety and effectiveness for the treatment of partial-onset seizures in pediatric patients below the age of 1 month; adjunctive therapy for the treatment of myoclonic seizures in pediatric patients below the age of 12 years; and adjunctive therapy for the treatment of primary generalized tonic-clonic seizures in pediatric patients below the age of 6 years have not been established.
A 3-month, randomized, double-blind, placebo-controlled study was performed to assess the neurocognitive and behavioral effects of KEPPRA as adjunctive therapy in 98 (KEPPRA N=64, placebo N=34) pediatric patients, ages 4 years to 16 years, with partial seizures that were inadequately controlled. The target dose was 60 mg/kg/day .Neurocognitive effects were measured by the Leiter-R Attention and Memory (AM) Battery, which measures various aspects of a child's memory and attention. Although no substantive differences were observed between the placebo and drug treated groups in the median change from baseline in this battery, the study was not adequate to assess formal statistical non-inferiority of the drug and placebo. The Achenbach Child Behavior Checklist (CBCL/6-18), a standardized validated tool used to assess a child's competencies and behavioral/emotional problems, was also assessed in this study. An analysis of the CBCL/6-18 indicated, on average, a worsening in KEPPRA-treated patients in aggressive behavior, one of the eight syndrome scores [see Warnings and Precautions (5.1)] .
Juvenile Animal Toxicity Data
Studies of levetiracetam in juvenile rats (dosed on postnatal days 4 through 52) and dogs (dosed from postnatal weeks 3 through 7) at doses of up to 1800 mg/kg/day (approximately 7 and 24 times, respectively, the maximum recommended pediatric dose of 60 mg/kg/day on a mg/m 2basis) did not demonstrate adverse effects on postnatal development.
8.5 Geriatric Use
There were 347 subjects in clinical studies of levetiracetam that were 65 years old and over. No overall differences in safety were observed between these subjects and younger subjects. There were insufficient numbers of elderly subjects in controlled trials of epilepsy to adequately assess the effectiveness of KEPPRA in these patients.
Levetiracetam is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Clinical Pharmacology (12.3)] .
8.6 Renal Impairment
Clearance of levetiracetam is decreased in patients with renal impairment and is correlated with creatinine clearance [see Clinical Pharmacology (12.3)] . Dosage adjustment is recommended for patients with impaired renal function and supplemental doses should be given to patients after dialysis [see Dosage and Administration (2.7)] .
10. Overdosage
10.1 Signs, Symptoms and Laboratory Findings of Acute Overdosage in Humans
The highest known dose of oral KEPPRA received in the clinical development program was 6000 mg/day. Other than drowsiness, there were no adverse reactions in the few known cases of overdose in clinical trials. Cases of somnolence, agitation, aggression, depressed level of consciousness, respiratory depression, and coma were observed with KEPPRA overdoses in postmarketing use.
10.2 Management of Overdose
There is no specific antidote for overdose with KEPPRA. If indicated, elimination of unabsorbed drug should be attempted by emesis or gastric lavage; usual precautions should be observed to maintain airway. General supportive care of the patient is indicated including monitoring of vital signs and observation of the patient's clinical status. A Certified Poison Control Center should be contacted for up to date information on the management of overdose with KEPPRA.
10.3 Hemodialysis
Standard hemodialysis procedures result in significant clearance of levetiracetam (approximately 50% in 4 hours) and should be considered in cases of overdose. Although hemodialysis has not been performed in the few known cases of overdose, it may be indicated by the patient's clinical state or in patients with significant renal impairment.
11. Keppra Injection Description
KEPPRA injection is an antiepileptic drug available as a clear, colorless, sterile solution (100 mg/mL) for intravenous administration.
The chemical name of levetiracetam, a single enantiomer, is (-)-(S)-α-ethyl-2-oxo-1-pyrrolidine acetamide, its molecular formula is C8H14N2O2 and its molecular weight is 170.21. Levetiracetam is chemically unrelated to existing antiepileptic drugs (AEDs). It has the following structural formula:
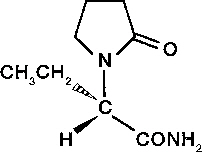
Levetiracetam is a white to off-white crystalline powder with a faint odor and a bitter taste. It is very soluble in water (104.0 g/100 mL). It is freely soluble in chloroform (65.3 g/100 mL) and in methanol (53.6 g/100 mL), soluble in ethanol (16.5 g/100 mL), sparingly soluble in acetonitrile (5.7 g/100 mL) and practically insoluble in n-hexane. (Solubility limits are expressed as g/100 mL solvent.)
KEPPRA injection contains 100 mg of levetiracetam per mL. It is supplied in single-use 5 mL vials containing 500 mg levetiracetam, water for injection, 45 mg sodium chloride, and buffered at approximately pH 5.5 with glacial acetic acid and 8.2 mg sodium acetate trihydrate. KEPPRA injection must be diluted prior to intravenous infusion [see Dosage and Administration (2.6)] .
12. Keppra Injection - Clinical Pharmacology
12.1 Mechanism of Action
The precise mechanism(s) by which levetiracetam exerts its antiepileptic effect is unknown.
A saturable and stereoselective neuronal binding site in rat brain tissue has been described for levetiracetam. Experimental data indicate that this binding site is the synaptic vesicle protein SV2A, thought to be involved in the regulation of vesicle exocytosis. Although the molecular significance of levetiracetam binding to synaptic vesicle protein SV2A is not understood, levetiracetam and related analogs showed a rank order of affinity for SV2A which correlated with the potency of their antiseizure activity in audiogenic seizure-prone mice. These findings suggest that the interaction of levetiracetam with the SV2A protein may contribute to the antiepileptic mechanism of action of the drug.
12.2 Pharmacodynamics
Effects on QTc Interval
The effect of KEPPRA on QTc prolongation was evaluated in a randomized, double-blind, positive-controlled (moxifloxacin 400 mg) and placebo-controlled crossover study of KEPPRA (1000 mg or 5000 mg) in 52 healthy subjects. The upper bound of the 90% confidence interval for the largest placebo-adjusted, baseline-corrected QTc was below 10 milliseconds. Therefore, there was no evidence of significant QTc prolongation in this study.
12.3 Pharmacokinetics
Equivalent doses of intravenous (IV) levetiracetam and oral levetiracetam result in equivalent C max, C min, and total systemic exposure to levetiracetam when the IV levetiracetam is administered as a 15-minute infusion.
Overview
Levetiracetam is rapidly and almost completely absorbed after oral administration. Levetiracetam injection and tablets are bioequivalent. The pharmacokinetics of levetiracetam are linear and time-invariant, with low intra- and inter-subject variability. Levetiracetam is not significantly protein-bound (<10% bound) and its volume of distribution is close to the volume of intracellular and extracellular water. Sixty-six percent (66%) of the dose is renally excreted unchanged. The major metabolic pathway of levetiracetam (24% of dose) is an enzymatic hydrolysis of the acetamide group. It is not liver cytochrome P450 dependent. The metabolites have no known pharmacological activity and are renally excreted. Plasma half-life of levetiracetam across studies is approximately 6-8 hours. It is increased in the elderly (primarily due to impaired renal clearance) and in subjects with renal impairment.
The pharmacokinetics of levetiracetam are similar when used as monotherapy or as adjunctive therapy for the treatment of partial-onset seizures.
Distribution
The equivalence of levetiracetam injection and the oral formulation was demonstrated in a bioavailability study of 17 healthy volunteers. In this study, levetiracetam 1500 mg was diluted in 100 mL 0.9% sterile saline solution and was infused over 15 minutes. The selected infusion rate provided plasma concentrations of levetiracetam at the end of the infusion period similar to those achieved at T maxafter an equivalent oral dose. It is demonstrated that levetiracetam 1500 mg intravenous infusion is equivalent to levetiracetam 3 × 500 mg oral tablets. The time independent pharmacokinetic profile of levetiracetam was demonstrated following 1500 mg intravenous infusion for 4 days with BID dosing. The AUC (0-12)at steady-state was equivalent to AUC inffollowing an equivalent single dose.
Levetiracetam and its major metabolite are less than 10% bound to plasma proteins; clinically significant interactions with other drugs through competition for protein binding sites are therefore unlikely.
Metabolism
Levetiracetam is not extensively metabolized in humans. The major metabolic pathway is the enzymatic hydrolysis of the acetamide group, which produces the carboxylic acid metabolite, ucb L057 (24% of dose) and is not dependent on any liver cytochrome P450 isoenzymes. The major metabolite is inactive in animal seizure models. Two minor metabolites were identified as the product of hydroxylation of the 2-oxo-pyrrolidine ring (2% of dose) and opening of the 2-oxo-pyrrolidine ring in position 5 (1% of dose). There is no enantiomeric interconversion of levetiracetam or its major metabolite.
Elimination
Levetiracetam plasma half-life in adults is 7 ± 1 hour and is unaffected by either dose, route of administration or repeated administration. Levetiracetam is eliminated from the systemic circulation by renal excretion as unchanged drug which represents 66% of administered dose. The total body clearance is 0.96 mL/min/kg and the renal clearance is 0.6 mL/min/kg. The mechanism of excretion is glomerular filtration with subsequent partial tubular reabsorption. The metabolite ucb L057 is excreted by glomerular filtration and active tubular secretion with a renal clearance of 4 mL/min/kg. Levetiracetam elimination is correlated to creatinine clearance. Levetiracetam clearance is reduced in patients with renal impairment [see Dosage and Administration (2.6)and Use in Specific Populations (8.6)] .
Specific Populations
Elderly
Pharmacokinetics of levetiracetam were evaluated in 16 elderly subjects (age 61-88 years) with creatinine clearance ranging from 30 to 74 mL/min. Following oral administration of twice-daily dosing for 10 days, total body clearance decreased by 38% and the half-life was 2.5 hours longer in the elderly compared to healthy adults. This is most likely due to the decrease in renal function in these subjects.
Pediatric Patients
- Intravenous Formulation
A population pharmacokinetic analysis for the intravenous formulation was conducted in 49 pediatric patients (1 month to < 16 years of age) weighing 3-79 kg. Patients received levetiracetam as a 15-minute IV infusion at doses between 14 mg/kg/day and 60 mg/kg/day twice daily. Plasma concentrations and model derived steady-state exposure AUC (0-12) were within the range of the exposure observed in pediatric patients receiving equivalent doses of the oral solution.
- Oral Formulations
Pharmacokinetics of levetiracetam were evaluated in 24 pediatric patients (age 6-12 years) after single oral dose (20 mg/kg) of the immediate release formulation of KEPPRA. The body weight adjusted apparent clearance of levetiracetam was approximately 40% higher than in adults.
A repeat dose pharmacokinetic study was conducted in pediatric patients (age 4-12 years) at doses of 20 mg/kg/day, 40 mg/kg/day, and 60 mg/kg/day of the immediate release formulation of KEPPRA. The evaluation of the pharmacokinetic profile of levetiracetam and its metabolite (ucb L057) in 14 pediatric patients demonstrated rapid absorption of levetiracetam at all doses, with a T maxof about 1 hour and a t 1/2of 5 hours across all dosing levels. The pharmacokinetics of levetiracetam in pediatric patients was linear between 20 to 60 mg/kg/day. The potential interaction of levetiracetam with other AEDs was also evaluated in these patients. Levetiracetam had no significant effect on the plasma concentrations of carbamazepine, valproic acid, topiramate or lamotrigine. However, there was about a 22% increase of apparent clearance of levetiracetam when it was co-administered with an enzyme-inducing AED (e.g., carbamazepine).
Following single dose administration (20 mg/kg) of a 10% oral solution to pediatric patients with epilepsy (1 month to < 4 years), levetiracetam was rapidly absorbed and peak plasma concentrations were observed approximately 1 hour after dosing. Levetiracetam half-life in pediatric patients 1 month to < 4 years with epilepsy was shorter (5.3 h) than in adults (7.2 h), and apparent clearance (1.5 mL/min/kg) was faster than in adults (0.96 mL/min/kg).
Population pharmacokinetic analysis showed that body weight was significantly correlated to the clearance of levetiracetam in pediatric patients; clearance increased with an increase in body weight.
Pregnancy
Levetiracetam levels may decrease during pregnancy [see Warnings and Precautions (5.10)and Use in Specific Populations (8.1)] .
Gender
Levetiracetam C maxand AUC were 20% higher in women (N=11) compared to men (N=12). However, clearances adjusted for body weight were comparable.
Race
Formal pharmacokinetic studies of the effects of race have not been conducted. Cross-study comparisons involving Caucasians (N=12) and Asians (N=12), however, show that pharmacokinetics of levetiracetam were comparable between the two races. Because levetiracetam is primarily renally excreted and there are no important racial differences in creatinine clearance, pharmacokinetic differences due to race are not expected.
Renal Impairment
The disposition of levetiracetam was studied in adult subjects with varying degrees of renal function. Total body clearance of levetiracetam is reduced in patients with impaired renal function by 40% in the mild group (CLcr = 50-80 mL/min), 50% in the moderate group (CLcr = 30-50 mL/min) and 60% in the severe renal impairment group (CLcr <30 mL/min). Clearance of levetiracetam is correlated with creatinine clearance.
In anuric (end stage renal disease) patients, the total body clearance decreased 70% compared to normal subjects (CLcr >80mL/min). Approximately 50% of the pool of levetiracetam in the body is removed during a standard 4 hour hemodialysis procedure [see Dosage and Administration (2.7)] .
Hepatic Impairment
In subjects with mild (Child-Pugh A) to moderate (Child-Pugh B) hepatic impairment, the pharmacokinetics of levetiracetam were unchanged. In patients with severe hepatic impairment (Child-Pugh C), total body clearance was 50% that of normal subjects, but decreased renal clearance accounted for most of the decrease. No dose adjustment is needed for patients with hepatic impairment.
Drug Interactions
In vitrodata on metabolic interactions indicate that levetiracetam is unlikely to produce, or be subject to, pharmacokinetic interactions. Levetiracetam and its major metabolite, at concentrations well above C maxlevels achieved within the therapeutic dose range, are neither inhibitors of, nor high affinity substrates for, human liver cytochrome P450 isoforms, epoxide hydrolase or UDP-glucuronidation enzymes. In addition, levetiracetam does not affect the in vitroglucuronidation of valproic acid.
Potential pharmacokinetic interactions of or with levetiracetam were assessed in clinical pharmacokinetic studies (phenytoin, valproate, warfarin, digoxin, oral contraceptive, probenecid) and through pharmacokinetic screening in the placebo-controlled clinical studies in epilepsy patients.
Phenytoin
KEPPRA (3000 mg daily) had no effect on the pharmacokinetic disposition of phenytoin in patients with refractory epilepsy. Pharmacokinetics of levetiracetam were also not affected by phenytoin.
Valproate
KEPPRA (1500 mg twice daily) did not alter the pharmacokinetics of valproate in healthy volunteers. Valproate 500 mg twice daily did not modify the rate or extent of levetiracetam absorption or its plasma clearance or urinary excretion. There also was no effect on exposure to and the excretion of the primary metabolite, ucb L057.
Other Antiepileptic Drugs
Potential drug interactions between KEPPRA and other AEDs (carbamazepine, gabapentin, lamotrigine, phenobarbital, phenytoin, primidone and valproate) were also assessed by evaluating the serum concentrations of levetiracetam and these AEDs during placebo-controlled clinical studies. These data indicate that levetiracetam does not influence the plasma concentration of other AEDs and that these AEDs do not influence the pharmacokinetics of levetiracetam.
Effect of AEDs in Pediatric Patients
There was about a 22% increase of apparent total body clearance of levetiracetam when it was co-administered with enzyme-inducing AEDs. Dose adjustment is not recommended. Levetiracetam had no effect on plasma concentrations of carbamazepine, valproate, topiramate, or lamotrigine.
Oral Contraceptives
KEPPRA (500 mg twice daily) did not influence the pharmacokinetics of an oral contraceptive containing 0.03 mg ethinyl estradiol and 0.15 mg levonorgestrel, or of the luteinizing hormone and progesterone levels, indicating that impairment of contraceptive efficacy is unlikely. Coadministration of this oral contraceptive did not influence the pharmacokinetics of levetiracetam.
Digoxin
KEPPRA (1000 mg twice daily) did not influence the pharmacokinetics and pharmacodynamics (ECG) of digoxin given as a 0.25 mg dose every day. Coadministration of digoxin did not influence the pharmacokinetics of levetiracetam.
Warfarin
KEPPRA (1000 mg twice daily) did not influence the pharmacokinetics of R and S warfarin. Prothrombin time was not affected by levetiracetam. Coadministration of warfarin did not affect the pharmacokinetics of levetiracetam.
Probenecid
Probenecid, a renal tubular secretion blocking agent, administered at a dose of 500 mg four times a day, did not change the pharmacokinetics of levetiracetam 1000 mg twice daily. C ssmaxof the metabolite, ucb L057, was approximately doubled in the presence of probenecid while the fraction of drug excreted unchanged in the urine remained the same. Renal clearance of ucb L057 in the presence of probenecid decreased 60%, probably related to competitive inhibition of tubular secretion of ucb L057. The effect of KEPPRA on probenecid was not studied.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Rats were dosed with levetiracetam in the diet for 104 weeks at doses of 50, 300, and 1800 mg/kg/day. Plasma exposure (AUC) at the highest dose was approximately 6 times that in humans at the maximum recommended human dose (MRHD) of 3000 mg. There was no evidence of carcinogenicity. In mice, oral administration of levetiracetam for 80 weeks (doses up to 960 mg/kg/day) or 2 years (doses up to 4000 mg/kg/day, lowered to 3000 mg/kg/day after 45 weeks due to intolerability) was not associated with an increase in tumors. The highest dose tested in mice for 2 years (3000 mg/kg/day) is approximately 5 times the MRHD on a body surface area (mg/m 2) basis.
14. Clinical Studies
All clinical studies supporting the efficacy of KEPPRA utilized oral formulations. The finding of efficacy of KEPPRA injection is based on the results of studies using an oral formulation of KEPPRA, and on the demonstration of comparable bioavailability of the oral and parenteral formulations [see Clinical Pharmacology (12.3)] .
14.1 Partial-Onset Seizures
Effectiveness in Partial-Onset Seizures in Adults
The effectiveness of KEPPRA for the treatment of partial-onset seizures in adults was established in three multicenter, randomized, double-blind, placebo-controlled clinical studies in patients who had refractory partial-onset seizures with or without secondary generalization. The tablet formulation was used in all these studies. In these studies, 904 patients were randomized to placebo, 1000 mg, 2000 mg, or 3000 mg/day. Patients enrolled in Study 1 or Study 2 had refractory partial-onset seizures for at least two years and had taken two or more classical AEDs. Patients enrolled in Study 3 had refractory partial-onset seizures for at least 1 year and had taken one classical AED. At the time of the study, patients were taking a stable dose regimen of at least one and could take a maximum of two AEDs. During the baseline period, patients had to have experienced at least two partial-onset seizures during each 4-week period.
Study 1
Study 1 was a double-blind, placebo-controlled, parallel-group study conducted at 41 sites in the United States comparing KEPPRA 1000 mg/day (N=97), KEPPRA 3000 mg/day (N=101), and placebo (N=95) given in equally divided doses twice daily. After a prospective baseline period of 12 weeks, patients were randomized to one of the three treatment groups described above. The 18-week treatment period consisted of a 6-week titration period, followed by a 12-week fixed dose evaluation period, during which concomitant AED regimens were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). The results of the analysis of Study 1 are displayed in Table 10.
| Placebo
(N=95) | KEPPRA
1000 mg/day (N=97) | KEPPRA
3000 mg/day (N=101) |
|
|---|---|---|---|
|
|||
| Percent reduction in partial seizure frequency over placebo | – | 26.1% * | 30.1% * |
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the three treatment groups (x-axis) is presented in Figure 1.
Figure 1: Responder Rate (≥50% Reduction from Baseline) in Study 1
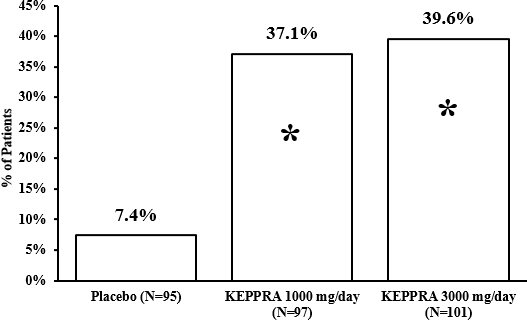
* statistically significant versus placebo
Study 2
Study 2 was a double-blind, placebo-controlled, crossover study conducted at 62 centers in Europe comparing KEPPRA 1000 mg/day (N=106), KEPPRA 2000 mg/day (N=105), and placebo (N=111) given in equally divided doses twice daily.
The first period of the study (Period A) was designed to be analyzed as a parallel-group study. After a prospective baseline period of up to 12 weeks, patients were randomized to one of the three treatment groups described above. The 16-week treatment period consisted of the 4-week titration period followed by a 12-week fixed dose evaluation period, during which concomitant AED regimens were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). The results of the analysis of Period A are displayed in Table 11.
| Placebo
(N=111) | KEPPRA
1000 mg/day (N=106) | KEPPRA
2000 mg/day (N=105) |
|
|---|---|---|---|
|
|||
| Percent reduction in partial seizure frequency over placebo | – | 17.1% * | 21.4% * |
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the three treatment groups (x-axis) is presented in Figure 2.
Figure 2: Responder Rate (≥50% Reduction from Baseline) in Study 2: Period A
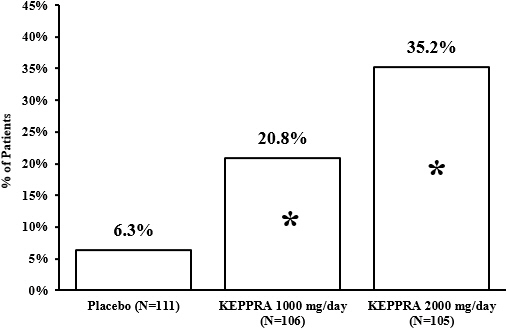
* statistically significant versus placebo
The comparison of KEPPRA 2000 mg/day to KEPPRA 1000 mg/day for responder rate was statistically significant ( P=0.02). Analysis of the trial as a cross-over yielded similar results.
Study 3
Study 3 was a double-blind, placebo-controlled, parallel-group study conducted at 47 centers in Europe comparing KEPPRA 3000 mg/day (N=180) and placebo (N=104) in patients with refractory partial-onset seizures, with or without secondary generalization, receiving only one concomitant AED. Study drug was given in two divided doses. After a prospective baseline period of 12 weeks, patients were randomized to one of two treatment groups described above. The 16-week treatment period consisted of a 4-week titration period, followed by a 12-week fixed dose evaluation period, during which concomitant AED doses were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). Table 12 displays the results of the analysis of Study 3.
| Placebo
(N=104) | KEPPRA
3000 mg/day (N=180) |
|
|---|---|---|
|
||
| Percent reduction in partial seizure frequency over placebo | – | 23.0% * |
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 3.
Figure 3: Responder Rate (≥50% Reduction from Baseline) in Study 3
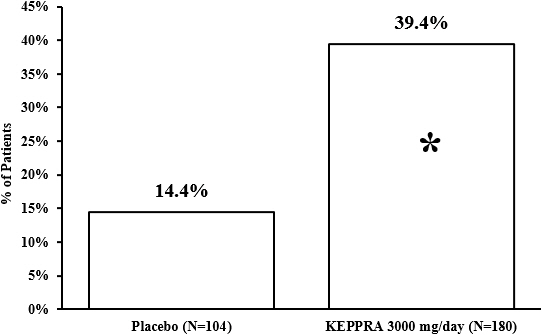
* statistically significant versus placebo
Effectiveness in Partial-Onset Seizures in Pediatric Patients 4 Years to 16 Years of Age
Study 4 was a multicenter, randomized double-blind, placebo-controlled study, in pediatric patients 4 to 16 years of age with partial seizures uncontrolled by standard antiepileptic drugs (AEDs). Study 4 was conducted at 60 sites in North America. The study consisted of an 8-week baseline period and 4-week titration period followed by a 10-week evaluation period. Eligible patients who still experienced, on a stable dose of 1-2 AEDs, at least 4 partial-onset seizures during the 4 weeks prior to screening, as well as at least 4 partial-onset seizures in each of the two 4-week baseline periods, were randomized to receive either KEPPRA or placebo. Dosing was initiated at a dose of 20 mg/kg/day in two divided doses. During the treatment period, KEPPRA doses were adjusted in 20 mg/kg/day increments, at 2-week intervals to the target dose of 60 mg/kg/day. The primary measure of efficacy was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire 14-week randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥ 50% reduction from baseline in partial-onset seizure frequency per week). The enrolled population included 198 patients (KEPPRA N=101, placebo N=97) with refractory partial-onset seizures, whether or not secondarily generalized. Table 13 displays the results of Study 4.
| Placebo
(N=97) | KEPPRA
(N=101) |
|
|---|---|---|
|
||
| Percent reduction in partial seizure frequency over placebo | - | 26.8% * |
The percentage of patients (y-axis) who achieved ≥ 50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 4.
Figure 4: Responder Rate (≥ 50% Reduction from Baseline) in Study 4
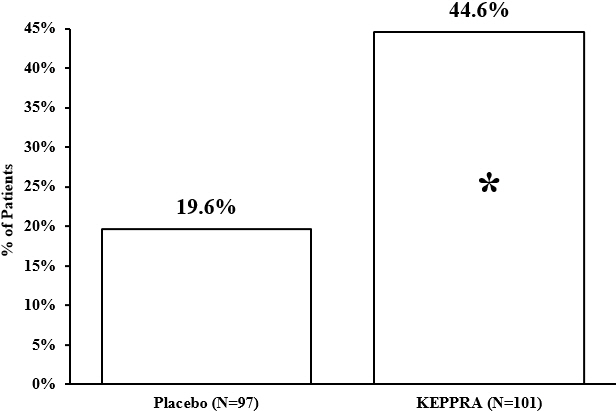
*statistically significant versus placebo
Effectiveness in Partial-Onset Seizures in Pediatric Patients 1 Month to <4 Years of Age
Study 5 was a multicenter, randomized double-blind, placebo-controlled study, in pediatric patients 1 month to less than 4 years of age with partial seizures, uncontrolled by standard epileptic drugs (AEDs). Study 5 was conducted at 62 sites in North America, South America, and Europe. Study 5 consisted of a 5-day evaluation period, which included a 1-day titration period followed by a 4-day maintenance period. Eligible patients who experienced, on a stable dose of 1-2 AEDs, at least 2 partial-onset seizures during the 48-hour baseline video EEG were randomized to receive either KEPPRA or placebo. Randomization was stratified by age range as follows: 1 month to less than 6 months of age (N=4 treated with KEPPRA), 6 months to less than 1 year of age (N=8 treated with KEPPRA), 1 year to less than 2 years of age (N=20 treated with KEPPRA), and 2 years to less than 4 years of age (N=28 treated with KEPPRA). KEPPRA dosing was determined by age and weight as follows: children 1 month to less than 6 months old were randomized to a target dose of 40 mg/kg/day, and children 6 months to less than 4 years old were randomized to a target dose of 50 mg/kg/day. The primary measure of efficacy was the responder rate (percent of patients with ≥ 50% reduction from baseline in average daily partial-onset seizure frequency) assessed by a blinded central reader using a 48-hour video EEG performed during the last two days of the 4-day maintenance period. The enrolled population included 116 patients (KEPPRA N=60, placebo N=56) with refractory partial-onset seizures, whether or not secondarily generalized. A total of 109 patients were included in the efficacy analysis. A statistically significant difference between KEPPRA and placebo was observed in Study 5 (see Figure 5). The treatment effect associated with KEPPRA was consistent across age groups.
Figure 5: Responder Rate for All Patients Ages 1 Month to < 4 Years (≥ 50% Reduction from Baseline) in Study 5
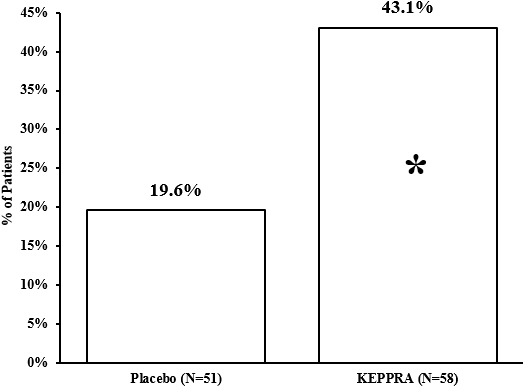
*statistically significant versus placebo
14.2 Myoclonic Seizures in Patients with Juvenile Myoclonic Epilepsy
The effectiveness of KEPPRA as adjunctive therapy in patients 12 years of age and older with juvenile myoclonic epilepsy (JME) experiencing myoclonic seizures was established in one multicenter, randomized, double-blind, placebo-controlled study (study 6), conducted at 37 sites in 14 countries. Eligible patients on a stable dose of 1 antiepileptic drug (AED) experiencing one or more myoclonic seizures per day for at least 8 days during the prospective 8-week baseline period were randomized to either KEPPRA or placebo (KEPPRA N=60, placebo N=60). Patients were titrated over 4 weeks to a target dose of 3000 mg/day and treated at a stable dose of 3000 mg/day over 12 weeks (evaluation period). Study drug was given in 2 divided doses. The primary measure of efficacy was the proportion of patients with at least 50% reduction in the number of days per week with one or more myoclonic seizures during the treatment period (titration + evaluation periods) as compared to baseline. Table 14 displays the results for the 113 patients with JME in this study.
14.3 Primary Generalized Tonic-Clonic Seizures
The effectiveness of KEPPRA as adjunctive therapy in patients 6 years of age and older with idiopathic generalized epilepsy experiencing primary generalized tonic-clonic (PGTC) seizures was established in one multicenter, randomized, double-blind, placebo-controlled study (study 7), conducted at 50 sites in 8 countries. Eligible patients on a stable dose of 1 or 2 antiepileptic drugs (AEDs) experiencing at least 3 PGTC seizures during the 8-week combined baseline period (at least one PGTC seizure during the 4 weeks prior to the prospective baseline period and at least one PGTC seizure during the 4-week prospective baseline period) were randomized to either KEPPRA or placebo. The 8-week combined baseline period is referred to as "baseline" in the remainder of this section. Patients were titrated over 4 weeks to a target dose of 3000 mg/day for adults or a pediatric target dose of 60 mg/kg/day and treated at a stable dose of 3000 mg/day (or 60 mg/kg/day for children) over 20 weeks (evaluation period). Study drug was given in 2 equally divided doses per day. The primary measure of efficacy was the percent reduction from baseline in weekly PGTC seizure frequency for KEPPRA and placebo treatment groups over the treatment period (titration + evaluation periods). The population included 164 patients (KEPPRA N=80, placebo N=84) with idiopathic generalized epilepsy (predominately juvenile myoclonic epilepsy, juvenile absence epilepsy, childhood absence epilepsy, or epilepsy with Grand Mal seizures on awakening) experiencing primary generalized tonic-clonic seizures. Each of these syndromes of idiopathic generalized epilepsy was well represented in this patient population.
There was a statistically significant decrease from baseline in PGTC frequency in the KEPPRA-treated patients compared to the placebo-treated patients in Study 7 (see Table 15).
| Placebo
(N=84) | KEPPRA
(N=78) |
|
|---|---|---|
|
||
| Percentage reduction in PGTC seizure frequency | 44.6% | 77.6% * |
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in PGTC seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 6.
Figure 6: Responder Rate (≥50% Reduction from Baseline) in PGTC Seizure Frequency per Week in Study 7
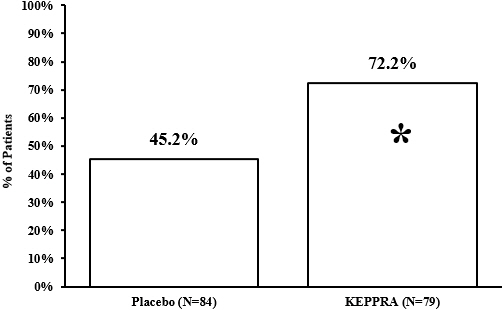
* statistically significant versus placebo
16. How is Keppra Injection supplied
17. Patient Counseling Information
Psychiatric Reactions and Changes in Behavior
Advise patients and their caregivers that KEPPRA may cause changes in behavior (e.g., aggression, agitation, anger, anxiety, apathy, depression, hostility, and irritability) and psychotic symptoms [see Warnings and Precautions (5.1)] .
Effects on Driving or Operating Machinery
Inform patients that KEPPRA may cause dizziness and somnolence. Inform patients not to drive or operate machinery until they have gained sufficient experience on KEPPRA to gauge whether it adversely affects their ability to drive or operate machinery [see Warnings and Precautions (5.2)] .
Anaphylaxis and Angioedema
Advise patients to discontinue KEPPRA and seek medical care if they develop signs and symptoms of anaphylaxis or angioedema [see Warnings and Precautions (5.3)].
Dermatological Adverse Reactions
Advise patients that serious dermatological adverse reactions have occurred in patients treated with KEPPRA and instruct them to call their physician immediately if a rash develops [see Warnings and Precautions (5.4)] .
DRESS/Multiorgan Hypersensitivity
Instruct patients and caregivers that a fever or rash associated with signs of other organ system involvement (e.g., lymphadenopathy, hepatic dysfunction) may be drug-related and should be reported to their healthcare provider immediately. KEPPRA should be discontinued immediately if a serious hypersensitivity reaction is suspected [see Warnings and Precautions (5.5)].
Withdrawal of KEPPRA
Advise patients and caregivers not to discontinue use of KEPPRA without consulting with their healthcare provider. KEPPRA should normally be gradually withdrawn to reduce the potential of increased seizure frequency and status epilepticus [seeWarnings and Precautions (5.7)].
Pregnancy
Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during KEPPRA therapy. Encourage patients to enroll in the North American Antiepileptic Drug (NAAED) pregnancy registry if they become pregnant [see Use in Specific Populations (8.1)] .
| KEPPRA
levetiracetam injection, solution, concentrate |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - UCB, Inc. (028526403) |
More about levetiracetam
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (434)
- Drug images
- Latest FDA alerts (6)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: pyrrolidine anticonvulsants
- Breastfeeding
- En español
Patient resources
Professional resources
- Levetiracetam monograph
- Levetiracetam (FDA)
- Levetiracetam Extended Release Tablets (FDA)
- Levetiracetam Injection (FDA)
- Levetiracetam Injection, Concentrate (FDA)
- Levetiracetam Solution (FDA)
Other brands
Keppra, Keppra XR, Spritam, Elepsia XR, ... +2 more