Estradiol
Generic name: estradiol oral [ ess-tra-DYE-ole ]
Brand names: Estrace, Vivelle-Dot, Vivelle, Delestrogen, DepoEstradiol,
... show all 17 brands
Drug class: Estrogens
What is estradiol?
Estradiol is a form of estrogen, a female sex hormone that regulates many processes in the body. It is available as an oral tablet, a topical gel or patch, vaginal cream, or as an injection.
Estradiol is used to treat menopause symptoms such as hot flashes and vaginal changes, and to prevent osteoporosis (bone loss) in menopausal women. Estradiol is also used to treat low estrogen levels in women with ovarian failure. It is also indicated to treat certain types of breast cancer and prostate cancer.
Estradiol may also be used for purposes not listed in this medication guide.
Warnings
You should not use estradiol if you have: undiagnosed vaginal bleeding, liver disease, a bleeding disorder, or if you have ever had a heart attack, a stroke, a blood clot, or cancer of the breast, uterus/cervix, or vagina.
Do not use estradiol if you are pregnant.
Estradiol may increase your risk of developing uterine cancer. Report any unusual vaginal bleeding right away.
Using this medicine can increase your risk of blood clots, stroke, or heart attack, or cancer of the breast, uterus, or ovaries. Estradiol should not be used to prevent heart disease, stroke, or dementia.
Have regular physical exams and mammograms, and self-examine your breasts for lumps on a monthly basis while using this medicine.
Before taking this medicine
You should not use this medicine if you are allergic to estradiol, or if you have:
-
unusual vaginal bleeding that has not been checked by a doctor;
-
liver disease;
-
a history of heart attack, stroke, or blood clot;
-
an increased risk of having blood clots due to a heart problem or a hereditary blood disorder; or
-
a history of hormone-related cancer, or cancer of the breast, uterus/cervix, or vagina.
Do not use estradiol if you are pregnant. Tell your doctor right away if you become pregnant during treatment.
Using this medicine can increase your risk of blood clots, stroke, or heart attack. You are even more at risk if you have high blood pressure, diabetes, high cholesterol, if you are overweight, or if you smoke.
Estradiol should not be used to prevent heart disease, stroke, or dementia, because this medicine may actually increase your risk of developing these conditions.
To make sure this medicine is safe for you, tell your doctor if you have ever had:
-
heart disease;
-
liver problems, or prior jaundice caused by pregnancy or taking hormones;
-
kidney disease;
-
cancer;
-
epilepsy or other seizure disorder;
-
migraines;
-
endometriosis or uterine fibroid tumors;
-
porphyria (a genetic enzyme disorder that causes symptoms affecting the skin or nervous system);
-
a thyroid disorder; or
-
high levels of calcium in your blood.
Using estradiol may increase your risk of cancer of the breast, uterus, or ovaries. Talk with your doctor about this risk.
Estradiol lowers the hormone needed to produce breast milk and can slow breast milk production. Tell your doctor if you are breast-feeding.
Related/similar drugs
Gemtesa, Erleada, Lupron Depot, Botox, alendronate, finasteride, oxybutynin
How should I take estradiol?
Take estradiol exactly as it was prescribed for you. Follow all directions on your prescription label. Do not take this medicine in larger amounts or for longer than recommended.
Estradiol may increase your risk of developing uterine cancer. To help lower this risk, your doctor may also want you to take a progestin. Report any unusual vaginal bleeding to your doctor immediately.
Your doctor should check your progress on a regular basis (every 3 to 6 months) to determine whether you should continue this treatment. Self-examine your breasts for lumps on a monthly basis and have a mammogram every year while using estradiol.
If you need major surgery or will be on long-term bed rest, you may need to stop using this medicine for a short time. Any doctor or surgeon who treats you should know that you are using this medicine.
Store at room temperature away from moisture, heat, and light. Keep the bottle tightly closed when not in use.
If you are taking injectable estrogen, dispose of any needles and syringes in an appropriate sharps container per your state laws. Do not throw away used needles into the garbage.
If you are using estradiol spray, avoid fire, flame, or smoking until the spray has dried. Do not apply lotion or sunscreen over the area for at least one hour.
What happens if I miss a dose?
Take the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not take extra medicine to make up the missed dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. Overdose can result in nausea, vomiting and vaginal bleeding.
What to avoid
Avoid smoking. It can greatly increase your risk of blood clots, stroke, or heart attack while using this medicine.
Grapefruit and grapefruit juice may interact with estradiol and lead to unwanted side effects. Avoid the use of grapefruit products.
Estradiol side effects
Get emergency medical help if you have signs of an allergic reaction to estradiol: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Call your doctor at once if you have:
-
heart attack symptoms - chest pain or pressure, pain spreading to your jaw or shoulder, nausea, sweating;
-
signs of a stroke - sudden numbness or weakness (especially on one side of the body), sudden severe headache, slurred speech, problems with vision or balance;
-
signs of a blood clot - sudden vision loss, stabbing chest pain, feeling short of breath, coughing up blood, pain or warmth in one or both legs;
-
swelling or tenderness in your stomach;
-
jaundice (yellowing of the skin or eyes);
-
memory problems, confusion, unusual behavior;
-
unusual vaginal bleeding, pelvic pain;
-
a lump in your breast; or
-
nausea, vomiting, constipation, increased thirst or urination, muscle weakness, bone pain, lack of energy.
Common estradiol side effects may include:
-
nausea, vomiting, diarrhea, stomach cramps;
-
mood changes, sleep problems (insomnia);
-
cold symptoms such as stuffy nose, sinus pain, sore throat;
-
headache, back pain, dizziness;
-
breast pain;
-
darkening of the skin or skin rash;
-
thinning scalp hair; or
-
vaginal itching or discharge, changes in your menstrual periods, breakthrough bleeding.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
What other drugs will affect estradiol?
Sometimes it is not safe to use certain medications at the same time. Some drugs can affect your blood levels of other drugs you take, which may increase side effects or make the medications less effective.
Many drugs can interact with estradiol. This includes prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide. Tell your doctor about all your current medicines and any medicine you start or stop using.
More about estradiol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (576)
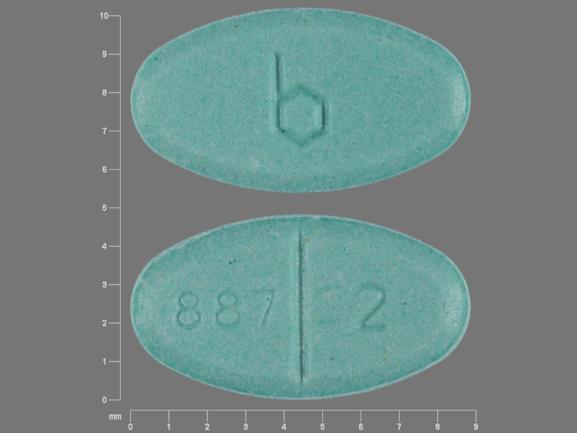
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: estrogens
- Breastfeeding
Patient resources
- Estradiol Oral Tablets patient information
- Estradiol Gel (Divigel)
- Estradiol Gel (Elestrin)
- Estradiol Gel (EstroGel)
- Estradiol Transdermal Biweekly Patch
Other brands
Estrace, Estrogel, Vivelle-Dot, Divigel, ... +14 more
Professional resources
Other brands
Estrace, Estradiol Patch, Dotti, Estrogel, ... +12 more
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use estradiol only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 12.05.