Atazanavir Side Effects
Medically reviewed by Drugs.com. Last updated on Jul 28, 2025.
Applies to atazanavir: oral capsule, oral powder.
Precautions
It is very important that your doctor check your progress at regular visits to make sure this medicine is working properly. Blood and urine tests are needed to check for unwanted effects.
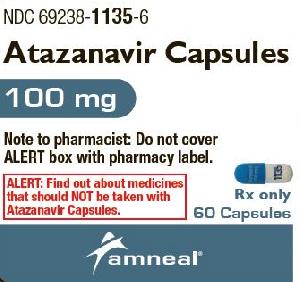
Do not use this medicine if you are also using alfuzosin (Uroxatral®), amiodarone (Pacerone®) with ritonavir, apalutamide (Erleada®), carbamazepine (Tegretol®), cisapride (Propulsid®), elbasvir/grazoprevir (Zepatier®), encorafenib (Braftovi®), glecaprevir/pibrentasvir (Mavyret®), indinavir (Crixivan®), irinotecan (Camptosar®), ivosidenib (Tibsovo®), lomitapide (Juxtapid®), lovastatin (Altocor®, Mevacor®), lurasidone (Latuda®) with ritonavir, nevirapine (Viramune®), oral midazolam (Versed®), phenobarbital (Solfoton®), phenytoin (Dilantin®), pimozide (Orap®), quinidine (Cardioquin®) with ritonavir, rifampin (Rifadin®, Rifamate®, Rifater®, Rimactane®), salmeterol (Advair®, Serevent®), sildenafil (Revatio®), simvastatin (Zocor®), triazolam (Halcion®), or ergot medicines (eg, dihydroergotamine, ergonovine, ergotamine, methylergonovine, Cafergot®, D.H.E. 45®, Ergomar®, Ergostat®, Ergotrate®, Methergine®, Migranal®, or Wigraine®).
This medicine may cause heart rhythm problems. Tell your doctor right away if you get dizzy or lightheaded, have a fast or irregular heartbeat, or feel like fainting.
Check with your doctor right away if you have pain or tenderness in the upper stomach, pale stools, dark urine, loss of appetite, nausea, unusual tiredness or weakness, or yellow eyes or skin. These could be symptoms of a serious liver problem.
This medicine may cause serious kidney problems, including chronic kidney disease. Your doctor may want your urine tested before and during treatment with this medicine. Talk to your doctor if you have concerns.
This medicine may increase your risk of having kidney stones. Check with your doctor right away if you have blood in your urine, nausea and vomiting, pain in the groin or genitals, or sharp back pain just below the ribs.
This medicine may increase blood sugar levels. Check with your doctor if you notice a change in the results of your blood or urine sugar tests.
Birth control pills may not work as well while you are using atazanavir. To keep from getting pregnant, use an additional form of birth control along with your pills. Other forms of birth control include condoms, a diaphragm, or contraceptive foam or jelly.
Your immune system may get stronger when you start taking HIV medicines. Tell your doctor right away if you notice any changes in your health. Sometimes the immune system will start to fight infections that were hidden in your body, including pneumonia or tuberculosis, or may result in a flare-up of a hidden autoimmune disorder (eg, Graves disease, polymyositis, Guillain-Barré syndrome, or autoimmune hepatitis).
Serious skin reactions (eg, Stevens-Johnson syndrome, erythema multiforme, toxic skin eruptions) can occur with this medicine. Check with your doctor right away if you have blistering, peeling, or loosening of the skin, chills, cough, diarrhea, itching, joint or muscle pain, red skin lesions, often with a purple center, skin rash, sore throat, sores, ulcers, or white spots in the mouth or on the lips, or unusual tiredness or weakness.
This medicine may cause you to have excess body fat. Tell your doctor if you notice changes in your body shape, including an increased amount of fat in the upper back and neck, or around the chest and stomach area. You might also lose fat from the legs, arms, and face.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription and nonprescription (over-the-counter [OTC]) medicines, and herbal (eg, St. John’s wort) or vitamin supplements.
Common side effects of atazanavir
Some side effects of atazanavir may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- back pain
- cough, increased
- discouragement
- extra body fat
- feeling sad or empty
- irritability
- loss of interest or pleasure
- trouble concentrating
- trouble sleeping
Less common side effects
- burning, numbness, tingling, or painful sensations
- difficulty with moving
- muscle stiffness
- pain
- pain in the joints
- unsteadiness or awkwardness
- weakness in the arms, hands, legs, or feet
Incidence not known
- hair loss or thinning of the hair
- rash with flat lesions or small raised lesions on the skin
Serious side effects of atazanavir
Along with its needed effects, atazanavir may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking atazanavir:
Incidence not known
- bloating
- blood in the urine
- blurred vision
- chest pain, discomfort, or tightness
- chills
- clay-colored stools
- constipation
- dark urine
- decreased appetite
- diarrhea
- dizziness or lightheadedness
- dry mouth
- fainting
- fast heartbeat
- fast, shallow breathing
- fever
- flushed, dry skin
- fruit-like breath odor
- gaseous abdominal or stomach pain
- general feeling of discomfort
- headache
- hives, itching, or skin rash
- increased hunger
- increased thirst
- increased urination
- indigestion
- irregular heartbeat
- loss of appetite
- loss of consciousness
- muscle pain or cramping
- nausea
- pain in the groin or genitals
- pain in the stomach, side, or abdomen, possibly radiating to the back
- recurrent fever
- severe nausea or vomiting
- sharp back pain just below the ribs
- sleepiness
- slow or irregular heartbeat
- stomach discomfort or fullness
- sweating
- swelling
- trouble breathing
- unexplained weight loss
- unpleasant breath odor
- unusual tiredness or weakness
- vomiting
- vomiting of blood
- yellow eyes or skin
See also:
For healthcare professionals
Applies to atazanavir: oral capsule, oral powder for reconstitution.
General adverse events
The most common side effects reported in therapy-naive patients during clinical trials were nausea, jaundice/scleral icterus, and rash. The most common side effects reported in therapy-experienced patients during clinical trials were jaundice/scleral icterus and myalgia.[Ref]
Hepatic
- Very common (10% or more): Elevated indirect (unconjugated) bilirubin (up to 87%), elevated total bilirubin (up to 53%), elevated ALT (up to 25%), jaundice (up to 19%)
- Common (1% to 10%): Elevated AST, jaundice/scleral icterus
- Uncommon (0.1% to 1%): Hepatitis
- Rare (less than 0.1%): Hepatosplenomegaly
- Frequency not reported: Hepatomegaly, liver damage, acute hepatic cytolysis, biliary lithiasis, choledocholithiasis
- Postmarketing reports: Hepatic function abnormalities, cholelithiasis, cholecystitis, cholestasis[Ref]
Elevated total bilirubin (at least 2.6 times the upper limit of normal [2.6 x ULN]), ALT (at least 5.1 x ULN), and AST (at least 5.1 x ULN) have been reported in up to 53%, up to 25%, and up to 10% of patients, respectively.
Most patients taking this drug experienced asymptomatic elevations in indirect (unconjugated) bilirubin related to inhibition of UDP-glucuronosyl transferase. This hyperbilirubinemia was reversible upon discontinuation of this drug.[Ref]
Other
- Very common (10% or more): Elevated total cholesterol (up to 25%)
- Common (1% to 10%): Elevated triglycerides, fever/pyrexia, pain, fatigue, asthenia, lipodystrophy syndrome
- Uncommon (0.1% to 1%): Chest pain, malaise, gait disturbances, decreased weight, weight gain
- Rare (less than 0.1%): Edema
- Frequency not reported: Elevated low-density lipoprotein cholesterol, elevated high-density lipoprotein cholesterol, burning sensation, dysplasia, facial atrophy, generalized edema, heat sensitivity, infection, overdose, pallor, peripheral edema, substernal chest pain, sweating, semicircular canal lithiasis[Ref]
Elevated total cholesterol (at least 240 mg/dL) and triglycerides (at least 751 mg/dL) have been reported in up to 25% and up to 8% of patients, respectively.[Ref]
Dermatologic
- Very common (10% or more): Rash (up to 20%)
- Common (1% to 10%): Lipodystrophy
- Uncommon (0.1% to 1%): Alopecia, pruritus, urticaria
- Rare (less than 0.1%): Vesiculobullous rash, eczema
- Frequency not reported: Photosensitivity
- Postmarketing reports: Maculopapular rash, erythema multiforme, toxic skin eruptions, drug rash with eosinophilia and systemic symptoms (DRESS) syndrome, angioedema, Stevens-Johnson syndrome[Ref]
Gastrointestinal
- Very common (10% or more): Nausea (up to 20%), elevated amylase (up to 14%), elevated lipase (up to 11%)
- Common (1% to 10%): Abdominal pain, diarrhea, vomiting, dyspepsia
- Uncommon (0.1% to 1%): Dry mouth, flatulence, gastritis, pancreatitis, abdominal distension, aphthous stomatitis
- Frequency not reported: Acholia, colitis, constipation, dental pain, esophageal ulcer, gastrointestinal disorder, peptic ulcer, sialolithiasis/parotid gland lithiasis[Ref]
Elevated amylase (at least 2.1 x ULN) and lipase (at least 2.1 x ULN) have been reported in up to 14% and up to 11% of patients, respectively.[Ref]
Nervous system
- Very common (10% or more): Headache (up to 14%)
- Common (1% to 10%): Peripheral neurological symptoms, dizziness
- Uncommon (0.1% to 1%): Syncope, peripheral neuropathy, amnesia, somnolence, dysgeusia
- Frequency not reported: Paresthesias[Ref]
Musculoskeletal
- Very common (10% or more): Elevated creatine kinase (up to 11%)
- Common (1% to 10%): Back pain, myalgia, arthralgia
- Uncommon (0.1% to 1%): Muscle atrophy
- Rare (less than 0.1%): Myopathy
- Frequency not reported: Bone pain, extremity pain, myasthenia, osteonecrosis[Ref]
Elevated creatine kinase (at least 5.1 x ULN) has been reported in up to 11% of patients.[Ref]
Hematologic
- Common (1% to 10%): Decreased neutrophils, decreased hemoglobin, decreased platelets
- Rare (less than 0.1%): Spontaneous bleeding in hemophiliacs[Ref]
Decreased neutrophils (less than 750 cells/mm3), hemoglobin (less than 8 g/dL), and platelets (less than 50,000 cells/mm3) have been reported in up to 8%, up to 5%, and up to 5% of patients, respectively.[Ref]
Metabolic
- Common (1% to 10%): Elevated glucose
- Uncommon (0.1% to 1%): Anorexia, increased appetite
- Rare (less than 0.1%): Ketoacidosis
- Frequency not reported: Hyperkalemia, lactic acidosis, hyperlactatemia, redistribution/accumulation of body fat (including central obesity, dorsocervical fat enlargement, peripheral wasting, facial wasting, breast enlargement, "cushingoid appearance"), hypertriglyceridemia, hypercholesterolemia, insulin resistance
- Postmarketing reports: New onset diabetes mellitus, exacerbation of preexisting diabetes mellitus, hyperglycemia[Ref]
Elevated glucose (at least 251 mg/dL) has been reported in 5% of patients.[Ref]
Psychiatric
- Common (1% to 10%): Depression, insomnia
- Uncommon (0.1% to 1%): Anxiety, disorientation, sleep disorder, abnormal dream[Ref]
Ocular
- Common (1% to 10%): Scleral icterus/ocular icterus[Ref]
Respiratory
- Common (1% to 10%): Increased cough
- Uncommon (0.1% to 1%): Dyspnea[Ref]
Cardiovascular
- Uncommon (0.1% to 1%): Hypertension
- Rare (less than 0.1%): Palpitation, vasodilatation
- Frequency not reported: Prolongation of the PR interval, abnormalities in atrioventricular (AV) conduction, first-degree AV block, prolonged QT interval, ventricular tachycardia, increased QRS interval, heart arrest, heart block, myocarditis
- Postmarketing reports: Second-degree AV block, third-degree AV block, left bundle branch block, QTc prolongation, torsades de pointes[Ref]
In healthy volunteers and patients, abnormalities in AV conduction were asymptomatic and generally limited to first-degree AV block.
A 59-year-old HIV-infected woman with congestive heart failure and an ejection fraction of 30% started lamivudine, zidovudine, and atazanavir. One month later, the patient presented with syncope and complained of nausea, which had begun 5 days prior. During the month after therapy initiation, the patient experienced slowly progressive shortness of breath. An ECG showed a QTc interval prolongation of 619 min. Prior to starting antiretroviral therapy, an ECG showed a QTc interval of 398 min for the patient. The patient developed continuous ventricular tachycardia and was defibrillated to sinus bradycardia, which worsened her QT interval prolongation. The patient developed torsades de pointes, which reverted after further defibrillation. Treatment to increase her heart rate and decrease her QT interval was started. The patient's antiretroviral therapy was discontinued during her hospitalization and was not restarted due to concerns regarding QT prolongation. The patient's QTc interval decreased to 394 min and she had no additional ventricular tachyarrhythmias. The patient was restarted on lamivudine, zidovudine, and atazanavir and within 2 days, ECG showed QTc interval prolongation to 571 min. The atazanavir was concluded to be the cause of the prolonged QT interval and torsades de pointes. The patient's QT interval returned to normal following discontinuation of her antiretroviral therapy.[Ref]
Renal
- Uncommon (0.1% to 1%): Interstitial nephritis
- Rare (less than 0.1%): Acute interstitial nephritis, renal colic, reversible acute renal failure, urolithiasis, kidney pain
- Postmarketing reports: Nephrolithiasis, hydronephrosis, renal insufficiency, granulomatous interstitial nephritis, chronic kidney disease[Ref]
An analysis of a ureteral stone determined it was 60% atazanavir metabolite and 40% calcium phosphate (carbonate apatite). The stone was not metabolites adsorbed into the apatite but contained atazanavir crystals. Analysis of renal calculi from additional patients determined concentrations of atazanavir ranging from 40% to 100%.
Postmarketing reports of chronic kidney disease in HIV-infected patients using this drug (with or without ritonavir) included biopsy-proven cases of granulomatous interstitial nephritis associated with deposition of atazanavir crystals in renal parenchyma.[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Hypersensitivity
- Frequency not reported: Allergic reaction[Ref]
Genitourinary
- Uncommon (0.1% to 1%): Hematuria, frequency of micturition/pollakiuria, proteinuria, gynecomastia
- Frequency not reported: Decreased male fertility[Ref]
Immunologic
- Frequency not reported: Immune reconstitution syndrome, autoimmune disorders in the setting of immune reconstitution (e.g., Graves' disease, polymyositis, Guillain-Barre syndrome)[Ref]
References
1. (2003) "Product Information. Reyataz (atazanavir)." Bristol-Myers Squibb
2. EMEA. European Medicines Agency (2007) EPARs. European Union Public Assessment Reports. http://www.ema.europa.eu/ema/index.jsp?curl=pages/includes/medicines/medicines_landingpage.jsp&mid
3. Croom KF, Dhillon S, Keam SJ (2009) "Atazanavir: A Review of its Use in the Management of HIV-1 Infection." Drugs, 69, p. 1107-40
4. Panel on Antiretroviral Guidelines for Adults and Adolescents (2018) Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf
5. Eholie SP, Lacombe K, Serfaty L, Wendum D, Girard PM (2004) "Acute hepatic cytolysis in an HIV-infected patient taking atazanavir." AIDS, 18, p. 1610-1
6. Anderson PL (2004) "Pharmacologic perspectives for once-daily antiretroviral therapy." Ann Pharmacother, 38, p. 1969-70
7. Johnson M, Grinsztejn B, Rodriguez C, et al. (2005) "Atazanavir plus ritonavir or saquinavir, and lopinavir/ritonavir in patients experiencing multiple virological failures." AIDS, 19, p. 685-94
8. Rotger M, Taffe P, Bleiber G, et al. (2005) "Gilbert syndrome and the development of antiretroviral therapy-associated hyperbilirubinemia." J Infect Dis, 192, p. 1381-6
9. Swainston Harrison T, Scott LJ (2005) "Atazanavir: A Review of its Use in the Management of HIV Infection." Drugs, 65, p. 2309-36
10. Johnson M, Grinsztejn B, Rodriguez C, et al. (2006) "96-week comparison of once-daily atazanavir/ritonavir and twice-daily lopinavir/ritonavir in patients with multiple virologic failures." AIDS, 20, p. 711-718
11. Ouagari Z, Tubiana R, Mohand HA, et al. (2006) "Skin rash associated with atazanavir: report of three cases." AIDS, 20, p. 1207-8
12. Cerner Multum, Inc. "UK Summary of Product Characteristics."
13. Piacenti FJ (2006) "An update and review of antiretroviral therapy." Pharmacotherapy, 26, p. 1111-33
14. Hammer SM, Saag MS, Schechter M, et al. (2006) "Treatment for adult HIV infection: 2006 recommendations of the International AIDS Society-USA panel." JAMA, 296, p. 827-43
15. Colombo S, Buclin T, Cavassini M, et al. (2006) "Population pharmacokinetics of atazanavir in patients with human immunodeficiency virus infection." Antimicrob Agents Chemother
16. Pacanowski J, Poirier JM, Petit I, Meynard JL, Girard PM (2006) "Atazanavir urinary stones in an HIV-infected patient." AIDS, 20, p. 2131
17. van Leeuwen E, Ter Heine R, van der Veen F, Repping S, Beijnen JH, Prins JM (2007) "Penetration of atazanavir in seminal plasma of men infected with HIV-1." Antimicrob Agents Chemother, 51, p. 335-7
18. Rodriguez-Novoa S, Martin-Carbonero L, Barreiro P, et al. (2007) "Genetic factors influencing atazanavir plasma concentrations and the risk of severe hyperbilirubinemia." AIDS, 21, p. 41-6
19. von Hentig N, Muller A, Rottmann C, et al. (2007) "Pharmacokinetics of saquinavir, atazanavir and ritonavir in a boosted double-protease inhibitor twice-daily regimen." Antimicrob Agents Chemother, 51, p. 1431-9
20. Gatell J, Salmon-Ceron D, Lazzarin A, et al. (2007) "Efficacy and safety of atazanavir-based highly active antiretroviral therapy in patients with virologic suppression switched from a stable, boosted or unboosted protease inhibitor treatment regimen: the SWAN Study (AI424-097) 48-week results." Clin Infect Dis, 44, p. 1484-92
21. Vernazza P, Daneel S, Schiffer V, et al. (2007) "The role of compartment penetration in PI-Monotherapy: the Atazanavir-Ritonavir Monomaintenance (ATARITMO) Trial." AIDS, 21, p. 1309-1315
22. Soriano V, Puoti M, Sulkowski M, et al. (2007) "Care of patients coinfected with HIV and hepatitis C virus: 2007 updated recommendations from the HCV-HIV International Panel." AIDS, 21, p. 1073-89
23. Warnke D, Barreto J, Temesgen Z (2007) "Antiretroviral drugs." J Clin Pharmacol, 47, p. 1570-9
24. Guaraldi G, Cocchi S, Motta A, et al. (2008) "A pilot study on the efficacy, pharmacokinetics and safety of atazanavir in patients with end-stage liver disease." J Antimicrob Chemother, 62, p. 1356-64
25. (2009) "Drugs for HIV infection." Treat Guidel Med Lett, 7, p. 11-22
26. Torti C, Lapadula G, Antinori A, et al. (2009) "Hyperbilirubinemia during atazanavir treatment in 2,404 patients in the Italian Atazanavir Expanded Access Program and MASTER Cohorts." Infection, 37, p. 244-9
27. Jacques AC, Giguere P, Zhang G, Touchie C, la Porte CJ (2009) "Atazanavir-associated choledocholithiasis leading to acute hepatitis in an HIV-infected adult (January)." Ann Pharmacother, 44, p. 202-6
28. Tozzi V (2010) "Pharmacogenetics of antiretrovirals." Antiviral Res, 85, p. 190-200
29. Park WB, Choe PG, Song KH, et al. (2010) "Genetic factors influencing severe atazanavir-associated hyperbilirubinemia in a population with low UDP-glucuronosyltransferase 1A1*28 allele frequency." Clin Infect Dis, 51, p. 101-6
30. Courbon E, Laylavoix F, Soulie C, et al. (2012) "Unexpected atazanavir-associated biliary lithiasis in an HIV-infected patient." J Antimicrob Chemother, 67, p. 250-1
31. Rakotondravelo S, Poinsignon Y, Borsa-Lebas F, et al. (2012) "Complicated atazanavir-associated Cholelithiasis: a Report of 14 Cases." Clin Infect Dis, 55, p. 1270-2
32. Jemsek JG, Arathoon E, Arlotti M, et al. (2006) "Body fat and other metabolic effects of atazanavir and efavirenz, each administered in combination with zidovudine plus lamivudine, in antiretroviral-naive HIV-infected patients." Clin Infect Dis, 42, p. 273-80
33. Pastori D, Esposito A, Cagliuso M, Conti V, Mezzaroma I (2009) "Lithiasis of semicircular canals and parotid glands: unusual stones deposition in atazanavir-treated individuals." AIDS, 23, p. 2233-4
34. Torres HA, Barnett BJ, Arduino RC (2007) "Alopecia associated with ritonavir-boosted atazanavir therapy." AIDS, 21, p. 1391-1392
35. Borras-Blasco J, Navarro-Ruiz A, Borras C, Castera E (2008) "Adverse cutaneous reactions associated with the newest antiretroviral drugs in patients with human immunodeficiency virus infection." J Antimicrob Chemother, 62, p. 879-88
36. Le MP, Stitou H, Soulie C, Katlama C, Peytavin G (2012) "Sialolithiasis in an HIV-1-infected patient treated with atazanavir/ritonavir monotherapy." J Antimicrob Chemother, 68, p. 727-9
37. Bergersen BM (2006) "Cardiovascular Risk in Patients with HIV Infection : Impact of Antiretroviral Therapy." Drugs, 66, p. 1971-87
38. Ly T, Ruiz ME (2007) "Prolonged QT Interval and Torsades de Pointes Associated with Atazanavir Therapy." Clin Infect Dis, 44, e67-8
39. Gallagher DP, Kieran J, Sheehan G, Lambert J, Mahon N, Mallon PW (2008) "Ritonavir-boosted atazanavir, methadone, and ventricular tachycardia: 2 case reports." Clin Infect Dis, 47, e36-8
40. Brewster UC, Perazella MA (2004) "Acute interstitial nephritis associated with atazanavir, a new protease inhibitor." Am J Kidney Dis, 44, e81-4
41. Roling J, Schmid H, Fischereder M, Draenert R, Goebel FD (2006) "HIV-Associated Renal Diseases and Highly Active Antiretroviral Therapy-Induced Nephropathy." Clin Infect Dis, 42, p. 1488-95
42. Chang HR, Pella PM (2006) "Atazanavir urolithiasis." N Engl J Med, 355, p. 2158-2159
43. Anderson PL, Lichtenstein KA, Gerig NE, Kiser JJ, Bushman LR (2007) "Atazanavir-containing renal calculi in an HIV-infected patient." AIDS, 21, p. 1060-2
44. Chan-Tack KM, Truffa MM, Struble KA, Birnkrant DB (2007) "Atazanavir-associated nephrolithiasis: cases from the US Food and Drug Administration's Adverse Event Reporting System." AIDS, 21, p. 1215-8
45. Couzigou C, Daudon M, Meynard JL, et al. (2007) "Urolithiasis in HIV-positive patients treated with atazanavir." Clin Infect Dis, 45, e105-8
46. Izzedine H, M'rad MB, Bardier A, Daudon M, Salmon D (2007) "Atazanavir crystal nephropathy." AIDS, 21, p. 2357-8
47. Koblic PM, Gold WL, la Porte CJ, Lee TC (2011) "Medication-based urolithiasis and atazanavir." CMAJ, 183, E748-51
Frequently asked questions
More about atazanavir
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (4)
- Drug images
- Dosage information
- During pregnancy
- Drug class: protease inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Atazanavir side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.