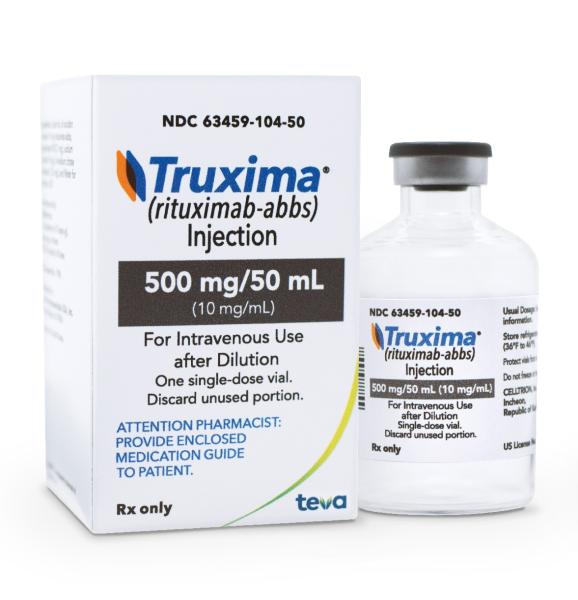
Truxima
Generic name: rituximab [ ri-TUX-i-mab ]
Drug class: CD20 monoclonal antibodies
What is Truxima?
Truxima injection is a prescription medicine used alone or in combination with other medicines to treat the following conditions in adults:
-
adults with rheumatoid arthritis; or
-
adults with granulomatosis with polyangiitis (GPA) and microscopic polyangiitis (MPA).
Truxima is not to be used in the treatment of children.
Warnings
Truxima may cause a serious brain infection that can lead to disability or death. Call your doctor right away if you have problems with speech, thought, vision, or muscle movement. These symptoms may start gradually and get worse quickly.
Tell your doctor if you have ever had hepatitis B. Truxima can cause this condition to come back or get worse.
Severe skin problems can also occur during treatment with Truxima. Call your doctor if you have painful skin or mouth sores, or a severe skin rash with blistering, peeling, or pus.
Some side effects may occur during the injection or within 24 hours afterward. Tell your caregiver right away if you feel itchy, dizzy, weak, light-headed, short of breath, or if you have chest pain, wheezing, sudden cough, or pounding heartbeats or fluttering in your chest.
Before taking this medicine
Truxima may cause a serious brain infection that can lead to disability or death. This infection may be more likely if have used an immunosuppressant drug in the past, or if you have received this medicine with a stem cell transplant.
To make sure Truxima is safe for you, tell your doctor if you have:
-
liver disease or hepatitis (or if you are a carrier of hepatitis B);
-
an infection, including herpes, shingles, cytomegalovirus, chickenpox, parvovirus, West Nile virus, or hepatitis B or C;
-
kidney disease;
-
lung disease or a breathing disorder;
-
a weak immune system (caused by disease or by using certain medicines);
-
heart disease, angina (chest pain), or heart rhythm disorder; or
-
if you have used Truxima in the past, or you have had a severe allergic reaction to this medicine.
You should be up-to-date on any needed immunizations before starting treatment with Truxima. Tell your doctor if you (or a child receiving this medicine) have received any vaccines within the past 4 weeks.
Do not use rituximab if you are pregnant. It could harm the unborn baby. Use effective birth control to prevent pregnancy while you are using Truxima and for at least 12 months after your last dose.
Do not breastfeed while using this medicine, and for at least 6 months after your last dose.
Related/similar drugs
Rituxan, Kymriah, Breyanzi, Yescarta, Polivy, Monjuvi, Xpovio
How is Truxima given?
Truxima is given as an infusion into a vein. A healthcare provider will give you this injection.
Your doctor will perform blood tests to make sure you do not have conditions that would prevent you from safely using Truxima.
Truxima is not given daily. Your schedule will depend on the condition being treated. Follow your doctor's dosing instructions very carefully.
Before each injection, you may be given other medications to prevent certain side effects of rituximab.
You will need frequent medical tests.
If you've ever had hepatitis B, using Truxima can cause this virus to become active or get worse. You may need frequent liver function tests while using this medicine and for several months after you stop.
If you need surgery, tell the surgeon ahead of time that you are using Truxima.
What happens if I miss a dose?
Call your doctor if you miss an appointment for your Truxima.
What happens if I overdose?
Since this medication is given by a healthcare professional in a medical setting, an overdose is unlikely to occur.
What should I avoid while receiving Truxima?
Do not receive a "live" vaccine while using Truxima. Live vaccines include measles, mumps, rubella (MMR), rotavirus, typhoid, yellow fever, varicella (chickenpox), zoster (shingles), and nasal flu (influenza) vaccine.
Truxima side effects
Get emergency medical help if you have signs of an allergic reaction to Truxima (hives, difficult breathing, swelling in your face or throat) or a severe skin reaction (fever, sore throat, burning eyes, skin pain, red or purple skin rash with blistering and peeling).
Some side effects may occur during the injection (or within 24 hours afterward). Tell your caregiver right away if you feel itchy, dizzy, weak, light-headed, short of breath, or if you have chest pain, wheezing, sudden cough, or pounding heartbeats or fluttering in your chest.
Truxima may cause a serious brain infection that can lead to disability or death. Call your doctor right away if you have any of the following symptoms (which may start gradually and get worse quickly):
-
confusion, memory problems, or other changes in your mental state;
-
weakness on one side of your body;
-
vision changes; or
-
problems with speech or walking.
Call your doctor at once if you have any of these other side effects, even if they occur several months after you receive Truxima, or after your treatment ends.
-
painful skin or mouth sores, or a severe skin rash with blistering, peeling, or pus;
-
redness, warmth, or swelling of the skin;
-
severe stomach pain, vomiting, constipation, bloody or tarry stools;
-
irregular heartbeats, chest pain or pressure, pain spreading to your jaw or shoulder;
-
tiredness or jaundice (yellowing of the skin or eyes);
-
signs of infection - fever, chills, cold or flu symptoms, cough, sore throat, mouth sores, headache, earache, pain or burning when you urinate; or
-
signs of tumor cell breakdown - confusion, weakness, muscle cramps, nausea, vomiting, fast or slow heart rate, decreased urination, tingling in your hands and feet or around your mouth.
Common Truxima side effects may include:
-
low white and red blood cells (fever, chills, body aches, pale skin, unusual tiredness, infections);
-
nausea, diarrhea;
-
swelling in your hands or feet;
-
headache, weakness;
-
painful urination;
-
muscle spasms;
-
depressed mood; or
-
cold symptoms such as stuffy nose, sneezing, sore throat.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
What other drugs will affect Truxima?
Tell your doctor about all your other medicines, especially:
-
medicines to treat conditions such as rheumatoid arthritis, Crohn's disease, ulcerative colitis, or psoriasis - adalimumab, certolizumab, etanercept, golimumab, infliximab, leflunomide, methotrexate, sulfasalazine, tocilizumab, tofacitinib, and others.
This list is not complete. Other drugs may interact with rituximab, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible drug interactions are listed here.
Popular FAQ
A biosimilar is a biological product that is similar to a reference biologic (usually the original product) and for which there are no clinically meaningful differences in terms of safety, purity, and potency. As an example, the biosimilar Amjevita (adalimumab-atto) was approved as the first biosimilar to Humira (adalimumab). Biosimilars are meant help to save patients and the healthcare system money. Continue reading
Weight gain has been reported in 11% of patients being treated with Truxima (rituximab) for non-Hodgkin’s lymphoma (NHL). Be sure to contact your doctor right away if you have a rapid or unexplained weight gain or fluid retention (edema), nausea, vomiting, diarrhea, or lack of energy when using Truxima, as you may need immediate medical care. Continue reading
Truxima (rituximab-abbs) is not a chemotherapy drug, rather it is a biologic that is targeted toward specific antigens (proteins). In this case, Truxima targets the CD20 antigen expressed on the surface of pre-B and mature B-lymphocytes. Truxima forms a complex with the CD20 antigen which causes B-cell death (lysis). Most cases of non-Hodgkin’s lymphoma and chronic lymphocytic leukemia arise from B cells. Truxima is usually used together with chemotherapy treatments. Continue reading
In patients with hematological or blood cancers, including non-Hodgkin's lymphoma (NHL) and chronic lymphocytic leukemia (CLL), Rituxan’s success is measured in a number of ways. It is measured by looking at how long patients responded to treatment (median duration of response), how long they live without their disease progressing (progression-free survival) and how many patients respond to treatment (response rate).
Rituxan treatment improves outcomes in certain patients with NHL. Adding Rituxan alongside standard therapies enhances the response patients have to treatment and improves overall outcomes, including increasing the time patients live for without experiencing a progression of their disease.
Rituxan helps to improve overall survival in certain patients with CLL and also helps to increase the time patients live for without experiencing disease progression. Adding Rituxan alongside standard therapy enhances the response patients have to therapy. Continue reading
Rituximab infusion reactions are caused primarily by cytokine release in the body. Cytokines are immune system proteins in the body that help to fight infections but can cause an inflammatory response. Infusion reactions may cause hives, itching, shortness of breath, chest pain or dizziness and are a very common side effect of treatment with rituximab (Rituxan). Continue reading
Treatment with Rituxan (rituximab) successfully improves patient outcomes in patients with rheumatoid arthritis including reducing symptoms, reducing levels of fatigue and disability, and increasing health-related quality of life. It also slows the progression of structural damage in joints. Continue reading
More FAQ
- How many biosimilars have been approved in the United States?
- What is the difference between Truxima and Rituxan?
- What are the new drugs for rheumatoid arthritis (RA)?
More about Truxima (rituximab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- FDA approval history
- Drug class: CD20 monoclonal antibodies
- Breastfeeding
- En español
Patient resources
- Truxima (Rituximab Intravenous) advanced reading
- Truxima (Rituximab-abbs Intravenous) (Advanced Reading)
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use Truxima only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 15.02.