Ibrutinib
Generic name: ibrutinib
Brand name: Imbruvica
Dosage form: oral tablet, oral capsule, oral suspension
Drug class: BTK inhibitors
What is ibrutinib?
Ibrutinib (Imbruvica) is a type of medication called a kinase inhibitor, which is used to treat various blood cancers and also a serious complication of allogeneic stem cell transplants called chronic graft versus host disease (cGVHD).
Ibrutinib helps to slow down how quickly certain blood cancers progress by working against cancerous B cells, a type of white blood cell. It does this by blocking Bruton's tyrosine kinase (BTK) signaling. BTK is a protein found on B cells that instructs B cells to remain alive and multiply. Ibrutinib also blocks the activity of a similar protein called interleukin-2-inducible T-cell kinase (ITK). It's thought that this action and it's ability to block BTK helps in cGVHD.
Ibrutinib was first approved by the US Food and Drug Administration (FDA) in 2013.
What is ibrutinib used for?
Ibrutinib is a prescription medicine used to treat :
- Adults with mantle cell lymphoma (MCL) who have received at least one prior treatment.
- Adults with chronic lymphocytic leukemia (CLL)/Small lymphocytic lymphoma (SLL).
- Adults with chronic lymphocytic leukemia (CLL)/Small lymphocytic lymphoma (SLL) with 17p deletion.
- Adults with Waldenström’s macroglobulinemia (WM).
- Adults with marginal zone lymphoma (MZL) who require a medicine by mouth or injection (systemic therapy) and have received a certain type of prior treatment.
- Adults and children 1 year of age and older with chronic graft versus host disease (cGVHD) after failure of 1 or more lines of systemic therapy.
It is not known if it is safe and effective in children under 1 year of age.
What should I tell my doctor before taking ibrutinib?
Before taking ibrutinib, tell your healthcare provider about all of your medical conditions, including if you:
- have had recent surgery or plan to have surgery. Your healthcare provider may stop ibrutinib for any planned medical, surgical, or dental procedure.
- have bleeding problems
- have or had heart rhythm problems, smoke, or have a medical condition that increases your risk of heart disease, such as high blood pressure, high cholesterol, or diabetes
- have an infection
- have liver problems
How should I take ibrutinib?
- Take ibrutinib exactly as your healthcare provider tells you to take it.
- Take 1 time a day at about the same time each day.
How should I take ibrutinib tablets and capsules
- Swallow ibrutinib capsules or tablets whole with a glass of water.
- Do not open, break, or chew the capsules.
- Do not cut, crush, or chew the tablets.
How should I take ibrutinib oral suspension
- Follow the Instructions for Use that comes with your oral suspension for information about the correct way to give a dose to your child. If you have questions about how to give this medication, talk to your healthcare provider or call 1-877-877-3536.
- Each oral suspension carton contains:
- 1 bottle of the medication with pre-inserted bottle adapter. Do not remove the bottle adapter
- 2 reusable 3 mL oral dosing syringes (called ‘syringe’ in this Instructions for Use) measuring in 0.1 mL increments.
- Only use the syringes that come with your medication. Do not use the syringes for other patients or with other medicines.
- If you cannot read the markings on the syringes, throw them away and call 1-877-877-3536 to get new ones.
- Preparing and giving a dose of ibrutinib oral suspension
- Step 1: Gather and check supplies
- Check your child’s prescribed dose in milliliters (mLs). Find this mL marking on the syringe.
- If the dose is more than the marking on the syringe, split the dose between syringes as prescribed.
- Gather bottle and syringe(s).
- Check the bottle and make sure that it is the correct medication and the printed on it and the expiration date (“EXP”) has not passed.
- Do not use if the expiration date has passed or the carton seal has been tampered with
- Step 2: Record or check discard date
- When opening the bottle for the first time, record the date that is 60 days from the day the bottle is opened underneath the words “Discard Date. Use within 60 days of opening.
- Step 3: Shake bottle before each use
- Step 4: Remove cap from bottle
- Press down and twist the cap counterclockwise to remove it from the bottle.
- If there is fluid on top of the adapter you may wipe it with clean disposable tissue.
- Do not remove the bottle adapter.
- Step 5: Attach syringe to bottle
- Make sure the syringe is clean and dry before use.
- Push the plunger down all the way.
- Gently insert tip of the syringe into the adapter.
- Turn the assembled bottle and syringe upside down.
- Step 6: Fill syringe
- Slowly pull the syringe plunger down, past the number of mLs for your prescribed dose.
- Check for air bubbles and proceed to Step 7 for instructions on how to remove air bubbles.
- Step 7: Remove air bubbles and adjust to the prescribed dose (mL)
- Hold the syringe and tap the sides to send bubbles to the tip.
- With the syringe attached to the bottle, push the plunger up to remove the air bubbles from the top.
- After the bubbles are removed, push the plunger up until the top of the colored plunger is even with the markings on the syringe for the dose.
- Air bubbles must be removed to ensure the correct dose. Repeat steps 6 and 7 if any air bubbles remain.
- Step 8: Remove syringe from bottle
- Turn the assembled bottle upright.
- Hold the middle of the syringe and carefully remove it from the bottle.
- Place the bottle aside.
- Do not touch the plunger of the syringe to avoid accidentally spilling the medicine before you are ready.
- Note: If more than 1 syringe is needed to give the full dose, repeat steps 5 to 8 with the second syringe to complete the prescribed dose.
- Step 9: Give ibrutinib oral suspension
- Place the tip of the syringe along the inside of your child’s cheek.
- Slowly push the plunger all the way in to give the entire dose.
- Repeat with second syringe if needed to complete the prescribed dose.
- Note: this medication must be given as soon as possible after being drawn from the bottle.
- Note: Make sure your child drinks water after swallowing the dose of medicine.
- Step 10: Recap bottle
- Place the cap back on the bottle.
- Make sure the bottle is tightly closed between each use.
- Step 11: Rinse syringe
- Remove plunger from the syringe, rinse only with water and air dry.
- Store the syringe in a clean, dry place.
- Do not clean the syringe with soap or in the dishwasher.
- Step 1: Gather and check supplies
- Each oral suspension carton contains:
What happens if I miss a dose?
If you miss a dose of ibrutinib take it as soon as you remember on the same day. Take your next dose at your regular time on the next day. Do not take extra doses of this medication to make up for a missed dose.
What happens if I overdose?
If you take too much ibrutinib call your healthcare provider or go to the nearest hospital emergency room right away.
What should I avoid while taking ibrutinib?
You should not drink grapefruit juice, eat grapefruit, or eat Seville oranges (often used in marmalades) during treatment with ibrutinib. These products may increase the amount of ibrutinib in your blood.
Dosing information
The recommended dose of ibrutinib for:
- Mantel cell lymphoma and marginal zone lymphoma is 560 mg taken orally once daily.
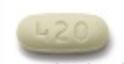
- Chronic lymphocytic leukemia/small lymphocytic lymphoma and Waldenström’s macroglobulinemia is 420 mg taken orally once daily.
- Chronic graft versus host disease in patients 12 years and older in 420 mg taken orally once daily. In patients aged 1 to less than 12 years of age the recommended dose is 240 mg/m2 taken orally once daily (up to a dose of 420 mg).
What are the side effects of ibrutinib?
Ibrutinib may cause serious side effects, including:
- Bleeding problems (hemorrhage) are common during treatment with ibrutinib, and can also be serious and may lead to death. Your risk of bleeding may increase if you are also taking a blood thinner medicine. Tell your healthcare provider if you have any signs of bleeding, including:
- blood in your stools or black stools (looks like tar)
- pink or brown urine
- unexpected bleeding, or bleeding that is severe or that you cannot control
- vomit blood or vomit looks like coffee grounds
- cough up blood or blood clots
- increased bruising
- dizziness
- weakness
- confusion
- change in your speech
- headache that lasts a long time or severe headache
- Infections can happen during treatment with ibrutinib. These infections can be serious and may lead to death. Tell your healthcare provider right away if you have fever, chills, weakness, confusion, or other signs or symptoms of an infection during treatment with ibrutinib.
- Heart problems. Serious heart rhythm problems (ventricular arrhythmias, atrial fibrillation and atrial flutter), heart failure and death have happened in people treated with ibrutinib, especially in people who have an increased risk for heart disease, have an infection, or who have had heart rhythm problems in the past. Tell your healthcare provider if you get any symptoms of heart problems, such as feeling as if your heart is beating fast and irregular, lightheadedness, dizziness, shortness of breath, swelling of the feet, ankles or legs, chest discomfort, or you faint. If you develop any of these symptoms, your healthcare provider may do a test to check your heart (ECG) and may change your ibrutinib dose.
- High blood pressure (hypertension). New or worsening high blood pressure has happened in people treated with ibrutinib. Your healthcare provider may start you on blood pressure medicine or change current medicines to treat your blood pressure.
- Decrease in blood cell counts. Decreased blood counts (white blood cells, platelets, and red blood cells) are common with ibrutinib, but can also be severe. Your healthcare provider should do monthly blood tests to check your blood counts.
- Second primary cancers. New cancers have happened during treatment with ibrutinib, including cancers of the skin or other organs.
- Tumor lysis syndrome (TLS). TLS is caused by the fast breakdown of cancer cells. TLS can cause kidney failure and the need for dialysis treatment, abnormal heart rhythm, seizure, and sometimes death. Your healthcare provider may do blood tests to check you for TLS.
The most common side effects of ibrutinib in adults with B-cell malignancies (MCL, CLL/SLL, WM and MZL) include:
- diarrhea
- tiredness
- muscle and bone pain
- rash
- bruising
The most common side effects of ibrutinib in adults or children 1 year of age and older with cGVHD include:
- tiredness
- muscle and joint pain
- nausea
- low red blood cell count (anemia)
- fever
- stomach pain
- bruising
- muscle spasms
- pneumonia
- diarrhea
- mouth sores (stomatitis)
- headache
- low platelet count
- bleeding
Diarrhea is a common side effect in people who take ibrutinib. Drink plenty of fluids during treatment with ibrutinib to help reduce your risk of losing too much fluid (dehydration) due to diarrhea. Tell your healthcare provider if you have diarrhea that does not go away.
These are not all the possible side effects of this medication.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
Interactions
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Taking ibrutinib with certain other medicines may affect how ibrutinib works and can cause side effects.
Pregnancy and breastfeeding
Tell your doctor if you are pregnant or plan to become pregnant. Ibrutinib can harm your unborn baby. If you are able to become pregnant, your healthcare provider will do a pregnancy test before starting treatment with ibrutinib. Tell your healthcare provider if you are pregnant or think you may be pregnant during treatment with ibrutinib.
- Females who are able to become pregnant should use effective birth control (contraception) during treatment with ibrutinib and for 1 month after the last dose.
- Males with female partners who are able to become pregnant should use effective birth control, such as condoms, during treatment with ibrutinib and for 1 month after the last dose.
Tell your doctor if you are breastfeeding or plan to breastfeed. Do not breastfeed during treatment with ibrutinib and for 1 week after the last dose.
Storage
- Store ibrutinib capsules and tablets at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep capsules in the original container with the lid tightly closed.
- Keep tablets in the original carton.
- Store ibrutinib oral suspension between 36°F and 77°F (2°C and 25°C).
- Do not freeze the oral suspension.
- Use the oral suspension within 60 days after first opening the bottle. Throw away any unused portion 60 days after opening.
Keep ibrutinib and all medicines out of sight and reach of children.
What are the ingredients in ibrutinib?
Active ingredient: ibrutinib
Inactive ingredients:
Capsules: croscarmellose sodium, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The 70 mg capsule shell contains gelatin, titanium dioxide, yellow iron oxide, and black ink. The 140 mg capsule shell contains gelatin, titanium dioxide, and black ink.
Tablets: colloidal silicon dioxide, croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone, and sodium lauryl sulfate. The film coating for each tablet contains ferrosoferric oxide (140 mg, 280 mg, and 420 mg tablets), polyvinyl alcohol, polyethylene glycol, red iron oxide (280 mg and 560 mg tablets), talc, titanium dioxide, and yellow iron oxide (140 mg, 420 mg, and 560 mg tablets).
Oral suspension: benzyl alcohol, citric acid monohydrate, disodium hydrogen phosphate, hypromellose, microcrystalline cellulose and carboxymethylcellulose sodium, purified water and sucralose.
Ibrutinib is distributed and marketed by Pharmacyclics LLC South San Francisco, CA 94080 USA. It is also marketed by Janssen Biotech, Inc. Horsham, PA 19044 USA.
Popular FAQ
How much does Imbruvica cost?
According to the Drugs.com price guide which bases its price on the Drugs.com discount card which is accepted at most U.S. pharmacies, the cost for Imbruvica 420mg tablet is around $616 per tablet or $17 269 for a supply of 28 tablets depending on the pharmacy you visit. Prices are for cash paying customers only and are not valid with insurance plans. Continue reading
How long can you stay on Imbruvica (ibrutinib)?
Imbruvica (ibrutinib) is usually continued indefinitely if it is being well tolerated, there is limited disease progression, and toxicity has not occurred. Continue reading
Can ibrutinib be stopped safely?
Stopping ibrutinib can result in a disease flare-up in patients with chronic lymphocytic leukemia (CLL). A 2020 study in The Oncologist found that approximately 25% of ibrutinib patients with a median interruption period of 8 days experienced a flare or rapid CLL progression. Continue reading
How quickly does Imbruvica (ibrutinib) work?
In some people, very good partial clinical responses to Imbruvica may occur within three to six months. Imbruvica is usually given until disease progression or unacceptable toxicity occurs, or in the case of graft vs host disease, recurrence of an underlying malignancy. The average duration of Imbruvica therapy in clinical trials has been around 41 months (range, 2–51 months).
Continue readingAcalabrutinib vs. ibrutinib: How do they compare?
A 2021 phase III study in the Journal of Clinical Oncology found that while both medications have similar efficacy, acalabrutinib was better tolerated with fewer side effects. Continue reading
Does ibrutinib cause hair loss?
Hair loss (alopecia) has not been noted as a side effect of ibrutinib (Imbuvica) in the product label. Textural hair changes (softening, straightening or curliness) and nail changes (brittle fingernails and toenails) were noted in a study evaluating ibrutinib use over the long term for treatment of chronic lymphocytic leukemia (CLL). Continue reading
More FAQ
References
More about ibrutinib
- Check interactions
- Compare alternatives
- Reviews (87)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: BTK inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.