PONATinib Hydrochloride (Monograph)
Brand name: Iclusig
Drug class: Antineoplastic Agents
Warning
- Arterial Occlusive Events
-
Arterial occlusive and thromboembolic events, including fatal MI, stroke, stenosis of large arterial vessels of the brain, severe peripheral vascular disease, and requirement for urgent revascularization procedures, occurred in patients receiving ponatinib.
-
Arterial occlusive events observed in patients with or without cardiovascular risk factors, including patients ≤50 years of age.
-
If an arterial occlusive event occurs, interrupt or discontinue ponatinib based on severity. Consider whether the benefits of restarting ponatinib therapy outweigh the risks.
- Venous Thromboembolic Events
-
Venous thromboembolic events (VTEs) occurred in patients receiving ponatinib. Monitor for evidence of VTEs.
-
If VTE occurs, interrupt or discontinue ponatinib based on severity.
- Heart Failure
-
Serious or fatal heart failure observed.
-
Monitor for heart failure and manage as clinically indicated.
-
If new or worsening heart failure occurs, interrupt therapy or discontinue ponatinib.
- Hepatotoxicity
-
Hepatotoxicity, liver failure, and death observed.
-
Monitor liver function tests prior to initiation of therapy and at least monthly thereafter or as clinically indicated.
-
If hepatotoxicity occurs, interrupt therapy and reduce dosage upon resumption, or discontinue ponatinib.
Introduction
Antineoplastic agent; an inhibitor of multiple receptor tyrosine kinases.
Uses for PONATinib Hydrochloride
Chronic Myelogenous Leukemia (CML) or Philadelphia Chromosome-Positive Acute Lymphoblastic Leukemia (ALL)
Treatment of adults with T315I-positive chronic phase, accelerated phase, or blast phase CML. Also used for chronic phase CML with resistance or intolerance to at least 2 prior kinase inhibitors and for accelerated phase or blast phase CML in patients for whom no other kinase inhibitors are indicated.
Not recommended for treatment of newly diagnosed chronic phase CML.
Used as monotherapy for treatment of Ph+ ALL in patients for whom no other kinase inhibitors are indicated or T315I-positive Ph+ALL.
Also used for treatment of newly diagnosed Ph+ALL in combination with chemotherapy. This indication is approved under accelerated approval based on minimal residual disease (MRD)-negative complete remission at end of induction. Continued approval for this indication may be contingent upon verification of clinical benefit in confirmatory trial(s).
Designated an orphan drug by FDA for use in these conditions.
PONATinib Hydrochloride Dosage and Administration
General
Pretreatment Screening
-
Verify pregnancy status of females of reproductive potential.
-
Perform liver function tests at baseline.
-
Measure BP at baseline.
-
Conduct a comprehensive eye exam at baseline.
-
Ensure adequate hydration and treat high uric acid levels prior to initiating ponatinib.
Patient Monitoring
-
Monitor liver function tests at least monthly or as clinically indicated.
-
Monitor serum lipase every 2 weeks for the first 2 months, then monthly thereafter or as clinically indicated; consider additional serum lipase monitoring in patients with a history of pancreatitis or alcohol abuse.
-
Monitor CBC every 2 weeks for the first 3 months, then monthly or as clinically indicated.
-
Monitor BP as clinically indicated.
-
Monitor for evidence of arterial occlusive events and VTE.
-
Monitor for signs or symptoms of heart failure.
-
Monitor for signs and symptoms suggestive of slow heart rate (e.g., fainting, dizziness) or rapid heart rate (e.g., chest pain, palpitations, dizziness).
-
Monitor for symptoms of neuropathy (e.g., hypoesthesia, hyperesthesia, paresthesia, discomfort, burning sensation, neuropathic pain or weakness).
-
Conduct comprehensive eye exams periodically during treatment.
-
Monitor for the presence of fluid retention and hemorrhage.
Dispensing and Administration Precautions
-
To avoid medication errors, the Institute for Safe Medication Practices (ISMP) recommends that prescribers communicate both the brand and generic names for ponatinib on the prescription order form.
Administration
Oral Administration
Administer orally once daily without regard to food.
Swallow tablets whole; do not crush, break, cut, or chew tablets.
If a dose is missed, give next dose at the regularly scheduled time the next day.
Dosage
Available as ponatinib hydrochloride; dosage expressed in terms of ponatinib.
Adults
Chronic Phase CML
Oral
Initially, 45 mg once daily; reduce to 15 mg once daily upon achievement of BCR-ABL1 IS ≤1%.
-
Re-escalate dosage to a previously tolerated dosage of 30 or 45 mg once daily if response is lost on 15 mg once daily.
-
Continue until loss of response at re-escalated dosage or unacceptable toxicity occurs.
-
Consider discontinuation if hematologic response not achieved by 3 months.
Accelerated Phase and Blast Phase CML
Oral
Initially, 45 mg once daily; optimal dosage not established.
-
Consider dosage reduction in patients with accelerated phase CML who have achieved major cytogenetic response.
-
Continue until loss of response or unacceptable toxicity occurs.
-
Consider discontinuation if hematologic response not achieved by 3 months.
Ph+ ALL
Oral
Newly diagnosed Ph+ ALL: initially, 30 mg once daily in combination with chemotherapy; reduce to 15 mg once daily upon achievement of MRD-negative (≤0.01% BCR::ABL1/ABL1) complete remission at end of induction. Continue ponatinib in combination with chemotherapy for up to 20 cycles until loss of response or unacceptable toxicity occurs.
Ph+ ALL for whom no other kinase inhibitors are indicated or T315I-positive Ph+ ALL: Initially, 45 mg once daily as monotherapy; optimal dosage not established. Continue until loss of response or unacceptable toxicity occurs. Consider discontinuation if response not achieved by 3 months.
Dosage Modification for Toxicity
If adverse reactions occur, temporary interruption of therapy, dosage reduction, and/or discontinuance of ponatinib may be necessary. If dosage modification required, reduce dosage as described in Table 1. Permanently discontinue in patients who are unable to tolerate the lowest dosage described in Table 1.
|
Dosage Reduction |
Chronic Phase CML |
Accelerated Phase or Blast Phase CML, or Ph+ ALL Monotherapy |
Newly Diagnosed Ph+ ALL |
|---|---|---|---|
|
First |
30 mg once daily |
30 mg once daily |
15 mg once daily |
|
Second |
15 mg once daily |
15 mg once daily |
10 mg once daily |
|
Third |
10 mg once daily |
Permanently discontinue if patient is unable to tolerate 15 mg once daily |
Permanently discontinue if patient is unable to tolerate 10 mg once daily |
|
Subsequent reduction |
Permanently discontinue if patient is unable to tolerate 10 mg once daily |
Permanently discontinue if patient is unable to tolerate 15 mg once daily |
Permanently discontinue if patient is unable to tolerate 10 mg once daily |
If an adverse reaction occurs, reduce ponatinib dosage, or interrupt or permanently discontinue therapy as described in Table 2.
|
Adverse Reaction and Severity |
Modification |
|---|---|
|
Cardiovascular or Cerebrovascular Arterial Occlusive Event |
|
|
Grade 1 |
Withhold ponatinib until resolved, then resume at the same dosage |
|
Grade 2 |
Withhold ponatinib until grade 0 or 1, then resume at the next lower dosage; discontinue ponatinib if event recurs |
|
Grade 3 or 4 |
Discontinue ponatinib |
|
Peripheral Vascular or Other Arterial Occlusive Event |
|
|
Grade 1 |
Withhold ponatinib until resolved, then resume at the same dosage |
|
Grade 2 |
Withhold ponatinib until grade 0 or 1, then resume at the same dosage; if event recurs, withhold ponatinib until grade 0 or 1, then resume at the next lower dosage |
|
Grade 3 |
Withhold ponatinib until grade 0 or 1, then resume at the next lower dosage; discontinue ponatinib if event recurs |
|
Grade 4 |
Discontinue ponatinib |
|
Venous Thromboembolism |
|
|
Grade 1 |
Withhold ponatinib until resolved, then resume at the same dosage |
|
Grade 2 |
Withhold ponatinib until grade 0 or 1, then resume at the same dosage; if event recurs, withhold ponatinib until grade 0 or 1, then resume at the next lower dosage |
|
Grade 3 |
Withhold ponatinib until grade 0 or 1, then resume at the next lower dosage; discontinue ponatinib if event recurs |
|
Grade 4 |
Discontinue ponatinib |
|
Heart Failure |
|
|
Grade 2 or 3 |
Withhold ponatinib until grade 0 or 1, then resume at the next lower dosage; discontinue ponatinib if event recurs |
|
Grade 4 |
Discontinue ponatinib |
|
Hepatotoxicity |
|
|
AST or ALT >3 times ULN |
Withhold ponatinib until grade 0 or 1, then resume at the next lower dosage |
|
AST or ALT ≥3 times ULN concurrent with bilirubin >2 times ULN and alkaline phosphatase <2 times ULN |
Discontinue ponatinib |
|
Pancreatitis or Elevated Serum Lipase |
|
|
Serum lipase >1 to 1.5 times ULN |
Consider withholding ponatinib until resolution, then resume at same dosage |
|
Serum lipase >1.5 to 2 times ULN, serum lipase 2 to 5 times ULN and asymptomatic, or asymptomatic radiologic pancreatitis |
Withhold ponatinib until grade 0 or 1 (<1.5 times ULN), then resume at next lower dosage |
|
Serum lipase >2 to 5 times ULN and symptomatic, symptomatic grade 3 pancreatitis, or serum lipase >5 times ULN and asymptomatic |
Withhold ponatinib until complete resolution of symptoms and after recovery of lipase elevation to grade 0 or 1; then resume at the next lower dosage |
|
Symptomatic pancreatitis and serum lipase >5 times ULN |
Discontinue ponatinib |
|
Myelosuppression |
|
|
ANC <1000/mm3 or platelets <50,000/mm3 |
Withhold ponatinib until ANC ≥1500/mm3 and platelets ≥75,000/mm3, then resume at the same dosage; if myelosuppression recurs, withhold ponatinib until resolution, then resume at the next lower dosage |
|
Other Non-Hematologic Adverse Events |
|
|
Grade 1 |
Withhold ponatinib until resolved, then resume at the same dosage |
|
Grade 2 |
Withhold ponatinib until grade 0 or 1, then resume at the same dosage; if event recurs, withhold ponatinib until grade 0 or 1, then resume at the next lower dosage |
|
Grade 3 or 4 |
Withhold ponatinib until grade 0 or 1, then resume at the next lower dosage; if event recurs, discontinue ponatinib |
Dosage Modification for Concomitant Use with Strong CYP3A Inhibitors
Avoid concomitant use of ponatinib with strong CYP3A inhibitors when possible. If concomitant use cannot be avoided, reduce ponatinib dosage as described in Table 3. After discontinuing a strong CYP3A inhibitor for 3–5 elimination half-lives, resume the dosage of ponatinib that was tolerated prior to initiating the strong CYP3A inhibitor.
|
Current Ponatinib Dosage |
Recommended Ponatinib Dosage with a Strong CYP3A Inhibitor |
|---|---|
|
45 mg once daily |
30 mg once daily |
|
30 mg once daily |
15 mg once daily |
|
15 mg once daily |
10 mg once daily |
|
10 mg once daily |
Avoid coadministration of ponatinib with a strong CYP3A inhibitor |
Special Populations
Hepatic Impairment
In patients with chronic phase CML, accelerated phase CML, blast phase CML, or Ph+ ALL and pre-existing hepatic impairment (Child-Pugh class A, B, or C) receiving monotherapy with ponatinib: reduce initial dosage from 45 mg once daily to 30 mg once daily.
In patients with newly diagnosed Ph+ ALL: no dosage adjustment necessary in mild hepatic impairment (Child-Pugh class A). Monitor patients with moderate or severe hepatic impairment (Child-Pugh class B or C) closely and modify dosage in the event of adverse reactions.
Renal Impairment
No specific dosage recommendations at this time.
Geriatric Use
Select dosage with caution because of greater frequency of age-related decreases in hepatic, renal, and/or cardiac function and of concomitant disease and drug therapy.
Cautions for PONATinib Hydrochloride
Contraindications
-
None.
Warnings/Precautions
Warnings
Arterial Occlusive Events
Arterial occlusive events, including fatalities, have occurred in patients receiving ponatinib in clinical trials. (See Boxed Warning.)
Consider whether benefits of ponatinib therapy outweigh risks. Monitor patients for manifestations of arterial occlusive events. If arterial occlusion is suspected, interrupt or discontinue therapy. Following evaluation, weigh the risks and benefits of restarting ponatinib.
Venous Thromboembolic Events
Serious or severe VTEs have occurred in patients receiving ponatinib. (See Boxed Warning.)
Monitor patients for manifestations of VTEs. If VTE occurs, interrupt treatment, then resume at the same or decreased dose or discontinue ponatinib based on recurrence/severity.
Heart Failure
Serious or severe heart failure events, including fatalities, have occurred. (See Boxed Warning.)
Monitor for manifestations of heart failure; manage as clinically indicated.
If new or worsening heart failure occurs, interrupt therapy and reduce dosage upon resumption or discontinue ponatinib.
Hepatotoxicity
Risk of hepatotoxicity, including liver failure and death. (See Boxed Warning.) Fulminant hepatic failure resulting in death following 1 week of therapy has occurred rarely. Liver enzyme elevations occur commonly.
Perform liver function tests prior to initiation of therapy and at least monthly thereafter or as clinically indicated.
If hepatotoxicity occurs, interrupt therapy and reduce dosage, or discontinue ponatinib.
Other Warnings and Precautions
Hypertension
Serious or severe hypertension, including hypertensive crisis, observed. BP elevations occur commonly. Urgent clinical intervention for symptoms associated with hypertension (e.g., confusion, headache, chest pain, shortness of breath) may be required.
Monitor BP and treat as clinically indicated. If hypertension is not medically controlled, interrupt therapy, reduce the dosage, or discontinue ponatinib. For significant worsening, labile, or treatment-resistant hypertension, interrupt ponatinib and consider evaluation for renal artery stenosis.
Pancreatitis
Pancreatitis and pancreatic laboratory abnormalities (e.g., elevated serum amylase and lipase) observed. Most cases resolve within 2 weeks of interruption of therapy or dosage reduction.
Monitor serum lipase concentrations every 2 weeks during the first 2 months of therapy and then monthly thereafter or as clinically indicated; consider more frequent monitoring in patients with a history of pancreatitis or alcohol abuse. If serum lipase concentrations are elevated and accompanied by abdominal pain, evaluate the patient for pancreatitis.
If pancreatitis occurs, interrupt therapy, then resume at the same or a reduced dosage, or discontinue ponatinib.
Increased Toxicity in Newly Diagnosed Chronic Phase CML
Ponatinib not indicated or recommended for use in patients with newly diagnosed chronic phase CML. Arterial and venous thrombosis and occlusions occurred at least twice as often in patients receiving ponatinib compared to patients receiving imatinib. Patients receiving ponatinib also had a higher incidence of myelosuppression, pancreatitis, hepatotoxicity, cardiac failure, hypertension, and skin and subcutaneous tissue disorders.
Neuropathy
Peripheral and cranial neuropathy observed; onset has occurred during the initial month of therapy. Most common peripheral neuropathies were paresthesia, hypoesthesia, and muscular weakness.
Monitor patient for manifestations of neuropathy.
If neuropathy occurs, interrupt therapy, then resume at the same or a reduced dosage, or discontinue ponatinib.
Ocular Toxicity
Serious ocular toxicities leading to blindness or blurred vision observed. Retinal toxicities (i.e., macular edema, age-related macular degeneration, retinal vein occlusion, retinal hemorrhage, vitreous floaters), blurred vision, eye pain, and dry eye have occurred.
Perform comprehensive ophthalmologic examination at baseline and periodically during therapy.
Hemorrhage
Hemorrhage, sometimes serious or fatal, observed; increased incidence of serious hemorrhage in patients with accelerated or blast phase CML or Ph+ ALL than in patients with chronic phase CML. Most serious hemorrhagic events were GI hemorrhage or subdural hematoma. Hemorrhagic events occurred principally in patients with grade 4 thrombocytopenia.
Monitor for hemorrhage and manage as clinically indicated. If hemorrhage occurs, interrupt therapy, then resume at the same or a reduced dosage, or discontinue ponatinib.
Fluid Retention
Risk of serious fluid retention (i.e., pleural effusion, pericardial effusion, angioedema); brain edema resulting in death reported rarely.
Monitor for signs and symptoms of fluid retention. If fluid retention develops, manage patients as clinically indicated and interrupt therapy, then resume at the same or a reduced dosage, or discontinue ponatinib.
Cardiac Arrhythmias
Grade 3 or 4 cardiac arrhythmia events, sometimes requiring hospitalization, reported, including atrial fibrillation, atrial flutter, ventricular arrhythmia, symptomatic bradyarrhythmia requiring pacemaker implantation, cardiorespiratory arrest, supraventricular extrasystoles, supraventricular and ventricular tachycardia, atrial tachycardia, sinus bradycardia, bradycardia, QT prolongation, complete atrioventricular block, sinus node dysfunction, loss of consciousness, and syncope.
Monitor for signs and symptoms of slow heart rate (e.g., fainting, dizziness) or rapid heart rate (e.g., chest pain, palpitations, dizziness) and manage as clinically indicated. If cardiac arrhythmias occur, interrupt therapy, then resume at the same or a reduced dosage, or discontinue ponatinib.
Myelosuppression
Risk of grade 3 or 4 myelosuppression (i.e., neutropenia, anemia, thrombocytopenia); incidence increased in patients with blast or accelerated phase CML or Ph+ ALL.
Monitor CBC every 2 weeks during the first 3 months of therapy and then monthly (or as clinically indicated) thereafter. If hematologic toxicity occurs, interrupt therapy, then resume at the same or a reduced dosage.
Tumor Lysis Syndrome
Tumor lysis syndrome and hyperuricemia reported.
Ensure adequate hydration and treat hyperuricemia prior to initiation of ponatinib.
Reversible Posterior Leukoencephalopathy Syndrome
Reversible posterior leukoencephalopathy syndrome (RPLS) reported. Symptoms include hypertension, seizure, headache, decreased alertness, altered mental function, vision loss, and other visual and neurological disturbances. Magnetic resonance imaging is necessary to confirm diagnosis.
If RPLS occurs, interrupt ponatinib until resolution; safety of resuming ponatinib upon resolution is unknown.
Wound Healing Complications and GI Perforation
Impaired wound healing reported. Withhold ponatinib for ≥1 week before elective surgery and do not administer following major surgery for ≥2 weeks and until adequate wound healing occurs. Safety of ponatinib resumption after resolution of wound healing complications not established.
GI perforation or fistula reported. Permanently discontinue ponatinib in patients with GI perforation.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm based on mechanism of action and findings from animal studies. Verify pregnancy status of females of reproductive potential prior to initiating therapy. Advise females of reproductive potential to use effective contraception during therapy and for 3 weeks after the last dose. If used during pregnancy or if patient becomes pregnant, apprise patient of potential fetal hazard.
Specific Populations
Pregnancy
May cause fetal harm based on mechanism of action and findings from animal studies. No data available in human pregnancy. Verify pregnancy status of females of reproductive potential prior to initiating therapy. If used during pregnancy or if patient becomes pregnant, apprise patient of potential fetal hazard.
Lactation
No data on the presence of ponatinib in human milk or effects on the breastfed child or on milk production. Advise patients to avoid breastfeeding during ponatinib treatment and for 1 week following the last dose.
Females and Males of Reproductive Potential
Based on its mechanism of action and findings from animal studies, ponatinib may cause fetal harm. Verify the pregnancy status of females of reproductive potential prior to initiating therapy. Advise females of reproductive potential to use effective contraception during therapy and for 3 weeks after the last dose.
May impair fertility in females of reproductive potential; not known whether these effects on fertility are reversible.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
In the OPTIC trial in patients with chronic phase CML, patients ≥65 years of age had lower rates of BCR-ABL1 IS ≤1% at 12 months compared to younger patients (27% versus 47%). Patients ≥65 years of age were also more likely to experience arterial occlusive events compared to younger patients (38% versus 9%).
In the PACE trial, the major cytogenetic response rate in patients with chronic phase CML was 40% in patients ≥65 years of age compared with 65% in patients <65 years of age. In patients with accelerated or blast phase CML or Ph+ ALL, the major hematologic response rate was 45% in patients ≥65 years of age compared with 44% in patients <65 years of age. Arterial occlusive events occurred in 35% of patients ≥65 years of age and 21% of patients <65 years of age.
In the PhALLCON trial, no differences in efficacy seen in patients ≥65 years of age and younger patients. Arterial occlusive events occurred more frequently in patients ≥65 years of age as compared to those <65 years of age (21% versus 2.3%).
Certain toxicities may occur more frequently in geriatric patients ≥65 years of age. Select dosage cautiously in geriatric patients.
Hepatic Impairment
Patients with hepatic impairment are more likely to experience adverse reactions. Reduce initial dosage of ponatinib in patients with pre-existing hepatic impairment and chronic phase CML, accelerated phase CML, blast phase CML, or Ph+ ALL receiving monotherapy. Monitor patients with newly diagnosed Ph+ALL and moderate or severe hepatic impairment closely for an increased incidence of adverse reactions; dosage modification may be necessary.
Renal Impairment
No clinically significant difference in pharmacokinetics observed in patients with mild to moderate renal impairment (Clcr 30–89 mL/min). Data lacking in patients with severe renal impairment.
Common Adverse Effects
Monotherapy: Most common adverse reactions (>20%) include rash and related conditions, arthralgia, abdominal pain, headache, constipation, dry skin, hypertension, fatigue, fluid retention and edema, pyrexia, nausea, pancreatitis/lipase elevation, hemorrhage, anemia, hepatic dysfunction, arterial occlusive events. Grade 3 or 4 laboratory abnormalities (>20%) include decreased platelet count, decreased neutrophil count, decreased white blood cell count.
Combination with chemotherapy: Most common adverse reactions include hepatic dysfunction, arthralgia, rash and related complications, headache, pyrexia, abdominal pain, constipation, fatigue, nausea, oral mucositis, hypertension, pancreatitis/lipase elevation, peripheral neuropathy, hemorrhage, febrile neutropenia, fluid retention and edema, vomiting, paresthesia, cardiac arrhythmias. Grade 3 or 4 laboratory abnormalities (>20%) include decreased white blood cell count, decreased neutrophil count, decreased platelet count, decreased lymphocytes, decreased hemoglobin, increased lipase, increased ALT.
Drug Interactions
Principally metabolized by CYP3A4 and, to a lesser extent, by CYP isoenzymes 2C8, 2D6, and 3A5.
Does not inhibit metabolism of substrates for CYP isoenzymes 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A; does not induce metabolism of substrates for CYP1A2, 2B6, or 3A.
Inhibits P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), and bile salt export pump (BSEP); is a weak substrate for P-gp and BCRP.
Not a substrate for organic anion transport polypeptide (OATP) 1B1 or OATP1B3, or organic cation transporter (OCT) 1; does not inhibit OATP1B1, OATP1B3, OCT1, OCT2, organic anion transporter (OAT) 1, or OAT3.
Drugs and Foods Affecting Hepatic Microsomal Enzymes
Strong CYP3A inhibitors: Possible pharmacokinetic interaction (increased plasma concentrations of ponatinib). Avoid concomitant use when possible; if used concomitantly, reduce dosage of ponatinib.
Strong CYP3A inducers: Possible pharmacokinetic interaction (decreased plasma concentrations of ponatinib). Manufacturer recommends selecting medications with no or minimal CYP3A induction potential. Avoid concomitant use with strong CYP3A inducers unless potential benefit outweighs possible risk of reduced ponatinib exposure. Monitor for signs of reduced ponatinib efficacy if concomitant use cannot be avoided.
Specific Drugs and Food
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Grapefruit juice |
Possible increased serum concentrations of ponatinib |
Do not consume grapefruit products concomitantly with ponatinib |
|
Ketoconazole |
Increased ponatinib peak concentration by 47% and AUC by 78% |
Avoid concomitant use when possible; if used concomitantly, reduce ponatinib dosage |
|
Lansoprazole |
Decreased ponatinib peak concentration by 25% and AUC by 6% |
|
|
Rifampin |
Decreased ponatinib peak concentration by 42% and AUC by 62% |
Avoid concomitant use unless potential benefit outweighs the potential risk of decreased ponatinib exposure; if concomitant use cannot be avoided, monitor for signs of reduced ponatinib efficacy |
PONATinib Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Following oral administration, peak plasma concentrations are attained within 6 hours.
AUC and peak plasma concentration are approximately dose proportional over the ponatinib dose range of 2–60 mg.
Food
High-fat or low-fat meal did not affect peak plasma concentrations and AUC.
Distribution
Extent
Not known whether ponatinib is distributed into human milk.
Plasma Protein Binding
>99%.
Elimination
Metabolism
At least 64% of a dose undergoes phase I and phase II metabolism; principally metabolized by hepatic CYP isoenzymes (i.e., CYP3A4 and, to a lesser extent, CYP2C8, 2D6, and 3A5) and by esterases and/or amidases.
Elimination Route
Eliminated in feces (87%) and urine (5%).
Half-life
Mean terminal half-life: approximately 24 hours.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).
Actions
-
Inhibits multiple tyrosine kinases, including wild-type and mutant BCR-ABL, members of the Src family, c-Kit, members of the Eph family, TIE-2, Flt-3, RET, members of the vascular endothelial growth factor (VEGF) family, members of the platelet-derived growth factor (PDGF) family, and members of the fibroblast growth factor (FGF) family.
-
Inhibits BCR-ABL tyrosine kinase, an abnormal protein created by the Philadelphia chromosome abnormality in CML and Ph+ ALL that exhibits enhanced tyrosine kinase activity (i.e., increased phosphorylation of tyrosine residues).
-
Potently inhibits BCR-ABL kinase domain mutant forms, including T315I; also inhibits additional mutant tyrosine kinase receptors and oncogenic fusion proteins in vitro.
Advice to Patients
-
Advise patients to swallow ponatinib tablets whole and not to cut, crush, or dissolve the tablets. Advise patients not to drink grapefruit juice or eat grapefruit as it may increase the risk of adverse reactions with ponatinib.
-
Advise patients that if a dose of ponatinib is missed, the next dose should be taken at the regularly scheduled time; the dose should not be doubled.
-
Risk of arterial occlusive events and venous thromboembolic events. Advise patients to seek emergency help and contact clinician if any symptoms suggestive of a thromboembolic event occur (e.g., chest pain or pressure, shortness of breath, unilateral numbness or weakness, speech difficulty, headache, vision changes, severe abdominal pain, leg pain or swelling, or arm, back, neck, or jaw pain).
-
Risk of heart failure or cardiac arrhythmias. Advise patients to immediately report symptoms of irregular or slow or fast heart beat (e.g., dizziness, fainting or feeling faint, chest pain, palpitations, shortness of breath).
-
Risk of hepatotoxicity and importance of liver function test monitoring. Advise patients to immediately report any manifestations of hepatotoxicity (e.g., jaundice, unusual fatigue or drowsiness, unusually dark or “tea-colored” urine, anorexia, bleeding or bruising).
-
Risk of fetal harm. Advise patients to inform clinicians if they are or plan to become pregnant or plan to breast-feed. Apprise patient of potential hazard to the fetus if used during pregnancy; females of reproductive potential should use effective contraception during treatment and for 3 weeks after the last dose. Patients should avoid breastfeeding during treatment and for 1 week after the last dose. Advise females of reproductive potential of the potential for reduced fertility with ponatinib.
-
Risk of hypertension. Advise patients on the importance of regular monitoring of blood pressure during treatment. Advise patients to immediately report confusion, headache, dizziness, chest pain, or shortness of breath.
-
Risk of pancreatitis and importance of serum lipase monitoring. Advise patients to immediately report abdominal pain, nausea, or vomiting.
-
Risk of neuropathy. Advise patients to inform clinician if symptoms of neuropathy occur (e.g., hypoesthesia, hyperesthesia, paresthesia, discomfort, burning or tingling sensation, neuropathic pain or weakness, muscle weakness, vision changes, difficulty moving the eye, sagging or drooping of the face or eyelids, change in taste).
-
Risk of adverse ocular effects and importance of ophthalmologic examinations prior to and during ponatinib therapy. Advise patients to inform clinician if bleeding in the eye, perceived flashes of light, light sensitivity, floaters, dry or itchy eyes, blurred vision, or eye pain occur.
-
Risk of bleeding. Advise patients to promptly inform clinician of any episodes or signs of bleeding (e.g., unusual bleeding, bruising, confusion, headache, change in speech, drowsiness).
-
Risk of cytopenias. Advise patients to inform clinician if fever or other signs and symptoms of infection occur.
-
Risk of tumor lysis syndrome. Advise patients to maintain adequate hydration.
-
Risk of fluid retention. Advise patients to contact clinician promptly if swelling, weight gain, shortness of breath, or coughing occurs.
-
Risk of reversible posterior leukoencephalopathy syndrome. Advise patients to report symptoms such as seizure, headache, decreased alertness, altered mental function, vision loss, and other visual and neurological disturbances.
-
Risk of wound healing complications. Advise patients to inform clinician about any scheduled surgical procedure.
-
Risk of GI perforation. Advise patients to report any manifestations of GI perforation (e.g., abdominal pain or swelling, high fever).
-
Advise patients that ponatinib tablets contain lactose monohydrate.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care. For further information on the handling of antineoplastic agents, see the ASHP Guidelines on Handling Hazardous Drugs at [Web].
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
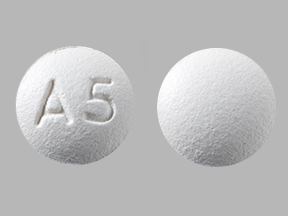
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
10 mg (of ponatinib) |
Iclusig |
Takeda |
|
15 mg (of ponatinib) |
Iclusig |
Takeda |
||
|
30 mg (of ponatinib) |
Iclusig |
Takeda |
||
|
45 mg (of ponatinib) |
Iclusig |
Takeda |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions December 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about ponatinib
- Check interactions
- Compare alternatives
- Reviews (2)
- Side effects
- Dosage information
- During pregnancy
- Drug class: BCR-ABL tyrosine kinase inhibitors
- Breastfeeding
- En español