Oxaliplatin (Monograph)
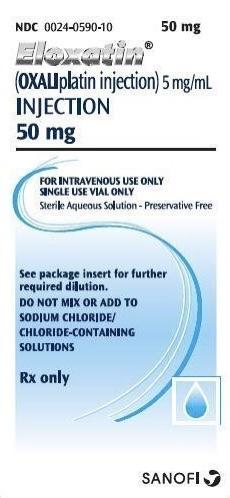
Brand name: Eloxatin
Drug class: Antineoplastic Agents
VA class: AN900
Chemical name: [SP-4-2-(1R-trans)]-(1,2-cyclohexanediamine-N,N′)[ethanedioato(2-)-O,O′]platinum
Molecular formula: C8H14N2O4Pt
CAS number: 61825-94-3
Warning
-
Risk of serious and fatal hypersensitivity reactions, including anaphylaxis; may occur within minutes following administration.1 (See Hypersensitivity Reactions under Cautions.)
Introduction
Antineoplastic agent; platinum-containing compound.1 2
Uses for Oxaliplatin
Colorectal Cancer
Used in combination with fluorouracil and leucovorin as adjuvant therapy for stage III colon cancer following complete resection of the primary tumor.1 9 10
Combined therapy with oral capecitabine† [off-label] is a reasonable choice (accepted, treatment option) as adjuvant therapy following complete resection of primary tumor in patients with stage III colon cancer.10001 10002 10003 10006 10007 10008 10011 10012 10013 10014 10015 10016 10018
Used in combination with fluorouracil and leucovorin for the treatment of advanced carcinoma of the colon or rectum.1 Evaluated as first-line therapy for unresectable colorectal cancer1 11 and as second-line therapy in patients whose disease recurred or progressed during or within 6 months following first-line therapy with fluorouracil, leucovorin, and irinotecan.1
Oxaliplatin Dosage and Administration
General
-
Administer on day 1 as part of a 2-day combination regimen.1 24
-
Premedication with antiemetics, including selective inhibitors of type 3 serotonergic (5-HT3) receptors (e.g., dolasetron, granisetron, ondansetron) with or without dexamethasone, recommended prior to each 2-day cycle.1
-
Hydration prior to administration not necessary.1
-
Handle cautiously (e.g., use gloves) to avoid exposure to oxaliplatin during preparation of IV solutions.1 Immediately treat accidental contact; wash skin thoroughly with soap and water or flush mucosa with copious amounts of water.1 Consult specialized references for procedures for proper handling and disposal of antineoplastics.
Administration
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Administer by IV infusion.1 24
Flush infusion line with 5% dextrose injection prior to administration of oxaliplatin or any concomitant drug.1 7 24
Aluminum may cause degradation of platinum compounds; do not use needles or IV administration sets that contain aluminum parts for reconstitution or dilution.1 24
Administer leucovorin by IV infusion concurrently with oxaliplatin but in a separate container using a Y-type administration set.1 24 Administer fluorouracil by direct IV injection (over 2–4 minutes), then by IV infusion.1 24 Consult respective manufacturer’s prescribing information for additional information on reconstitution and administration of fluorouracil and leucovorin.1 24
Reconstitution
Reconstitute vial containing 50 or 100 mg of oxaliplatin powder with 10 or 20 mL, respectively, of water for injection or 5% dextrose injection to provide a solution containing 5 mg/mL.7 24
Must be diluted further before IV administration.1 24
Dilution
Reconstituted solution or commercially available concentrate (5 mg/mL) must be further diluted prior to IV administration.1 24
Withdraw appropriate dose of oxaliplatin and dilute in 250–500 mL of 5% dextrose injection.1 24
Manufacturers of oxaliplatin recommend leucovorin and fluorouracil for IV infusion be diluted with 5% dextrose injection.1 24
Rate of Administration
Administer oxaliplatin over 2 hours.1 24
Administer leucovorin over 2 hours.1 24
Administer fluorouracil injection over 2–4 minutes followed by an IV infusion over 22 hours.1 24
Dosage
Adults
Stage III Colon Cancer (Adjuvant Therapy)
IV
Administer oxaliplatin/fluorouracil/leucovorin (FOLFOX4) regimen over 2 consecutive days.1 9
On day 1, administer oxaliplatin 85 mg/m2 concurrently with leucovorin 200 mg/m2 (in separate containers) by IV infusion over 2 hours.1 Then administer fluorouracil 400 mg/m2 by IV injection over 2–4 minutes, followed by fluorouracil 600 mg/m2 by IV infusion over 22 hours.1
On day 2, administer leucovorin 200 mg/m2 by IV infusion over 2 hours.1 Then administer fluorouracil 400 mg/m2 by IV injection over 2–4 minutes, followed by fluorouracil 600 mg/m2 by IV infusion over 22 hours.1
Repeat regimen at intervals of 2 weeks for a total of 12 cycles (6 months).1 9
Alternative regimen (modified FOLFOX6): On day 1, administer oxaliplatin 85 mg/m2 concurrently with leucovorin 400 mg/m2 (in separate containers) by IV infusion over 2 hours.12 Then administer fluorouracil 400 mg/m2 by IV injection over 5 minutes, followed by fluorouracil 1200 mg/m2 by IV infusion daily for 2 days (i.e., 2400 mg/m2 by IV infusion over 46–48 hours [total fluorouracil dosage of 2800 mg/m2 per cycle]).12 Repeat regimen at intervals of 2 weeks.12
Dosage of 130 mg/m2 IV over 2 hours on day 1 in combination with capecitabine† [off-label] 1 g/m2 orally twice daily on days 1–14 of each 3-week cycle, for a total of 4 or 8 cycles, also has been used;10001 10006 10008 10016 10017 4 cycles (for a treatment duration of 3 months) have been shown to have comparable efficacy and less toxicity than 8 cycles of therapy (for a treatment duration of 6 months).10008 10016 10017
Dosage Modification of FOLFOX4 for Toxicity in Stage III Colon Cancer
IVTo minimize acute toxicities, administer oxaliplatin over 6 hours; adjustment of infusion duration for fluorouracil or leucovorin not necessary.1
If hypersensitivity reaction, posterior reversible encephalopathy syndrome (PRES), interstitial lung disease, pulmonary fibrosis, or rhabdomyolysis occurs, permanently discontinue oxaliplatin.1
If persistent grade 2 peripheral sensory neuropathy occurs, consider reducing oxaliplatin dosage to 75 mg/m2.1 Consider drug discontinuance if persistent grade 3 peripheral sensory neuropathy occurs.1 If grade 4 peripheral sensory neuropathy occurs, discontinue oxaliplatin.1
If grade 3 or 4 thrombocytopenia, grade 4 neutropenia, or febrile neutropenia occurs, delay next dose of oxaliplatin until neutrophil count ≥1500/mm3 and platelet count ≥75,000/mm3, then resume oxaliplatin at a reduced dosage of 75 mg/m2.1
If grade 3 or 4 GI toxicity occurs, interrupt therapy until GI toxicity resolves, then reduce oxaliplatin dosage to 75 mg/m2 and reduce fluorouracil dosage to 300 mg/m2 by IV injection over 2–4 minutes and 500 mg/m2 by IV infusion over 22 hours.1
Advanced Colorectal Cancer
IV
Administer oxaliplatin/fluorouracil/leucovorin (FOLFOX4) regimen over 2 consecutive days.1 9
On day 1, administer oxaliplatin 85 mg/m2 concurrently with leucovorin 200 mg/m2 (in separate containers) by IV infusion over 2 hours.1 Then administer fluorouracil 400 mg/m2 by IV injection over 2–4 minutes, followed by fluorouracil 600 mg/m2 by IV infusion over 22 hours.1
On day 2, administer leucovorin 200 mg/m2 by IV infusion over 2 hours.1 Then administer fluorouracil 400 mg/m2 by IV injection over 2–4 minutes, followed by fluorouracil 600 mg/m2 by IV infusion over 22 hours.1
Repeat regimen at intervals of 2 weeks.1 Continue therapy until disease progression or unacceptable toxicity occurs.1 11
Alternative regimen (modified FOLFOX6): On day 1, administer oxaliplatin 85 mg/m2 concurrently with leucovorin 400 mg/m2 (or, alternatively, leucovorin 350 mg) (in separate containers) by IV infusion over 2 hours.12 Then administer fluorouracil 400 mg/m2 by IV injection over 5 minutes, followed by fluorouracil 1200 mg/m2 by IV infusion daily for 2 days (i.e., 2400 mg/m2 by IV infusion over 46–48 hours [total fluorouracil dosage of 2800 mg/m2 per cycle]).12 Repeat regimen at intervals of 2 weeks.12
Dosage Modification of FOLFOX4 for Toxicity in Advanced Colorectal Cancer
IVTo minimize acute toxicities, administer oxaliplatin over 6 hours; adjustment of infusion duration for fluorouracil or leucovorin not necessary.1
If hypersensitivity reaction, posterior reversible encephalopathy syndrome (PRES), interstitial lung disease, pulmonary fibrosis, or rhabdomyolysis occurs, permanently discontinue oxaliplatin.1
If persistent grade 2 adverse neurosensory effects occur, consider reducing the oxaliplatin dosage to 65 mg/m2.1 Consider drug discontinuance if persistent grade 3 neurosensory effects occur.1 If grade 4 peripheral sensory neuropathy occurs, discontinue oxaliplatin.1
If grade 3 or 4 thrombocytopenia, grade 4 neutropenia, or febrile neutropenia occurs, delay next dose of oxaliplatin until neutrophil count ≥1500/mm3 and platelet count ≥75,000/mm3, then resume oxaliplatin at a reduced dosage of 65 mg/m2.1
If grade 3 or 4 GI toxicity occurs, reduce oxaliplatin dosage to 65 mg/m2 and reduce fluorouracil dosage to 300 mg/m2 by IV injection over 2–4 minutes and 500 mg/m2 by IV infusion over 22 hours.1
Special Populations
Renal Impairment
Severe renal impairment (Clcr <30 mL/minute): Reduce dosage to 65 mg/m2.1
Mild (Clcr 50–79 mL/minute) or moderate (Clcr 30–49 mL/minute) renal impairment: No dosage adjustment necessary.1
Cautions for Oxaliplatin
Contraindications
-
History of hypersensitivity reactions to oxaliplatin, any ingredient in the formulation, or other platinum-containing compounds.1 7
Warnings/Precautions
Warnings
Hypersensitivity Reactions
Risk of anaphylaxis and other hypersensitivity reactions (e.g., rash, urticaria, erythema, pruritus, flushing, infusion-associated diarrhea, dyspnea, bronchospasm, diaphoresis, hypotension, chest pain, disorientation, syncope).1 24 (See Boxed Warning.) Can be fatal.1 Similar in nature and severity to those associated with other platinum-containing antineoplastic agents.1 May occur within minutes following administration and during any cycle of therapy.1
If a hypersensitivity reaction occurs, immediately and permanently discontinue the drug and initiate appropriate treatment.1
Other Warnings and Precautions
Consider the usual cautions, precautions, and contraindications of fluorouracil and leucovorin therapy.7
Neuropathy
Consistently associated with acute or delayed peripheral neuropathy.1 2 3 4 Duration and severity increase with increasing oxaliplatin cumulative dosage.2 7
Acute, reversible sensory neuropathy (e.g., acute transient paresthesia,1 3 dysesthesia,1 3 and hypoesthesia in hands, feet, perioral area, or throat, jaw spasm, abnormal tongue sensation, dysarthria, ocular pain, feeling of chest pressure1 ) may occur within hours1 2 or 2 days following oxaliplatin administration, resolves within 14 days, and frequently recurs with further administration of the drug.1 Acute neuropathy may be precipitated or exacerbated by exposure to cold temperature or cold objects;1 2 avoid ice (e.g., for mucositis prophylaxis) during oxaliplatin infusion.1
Possible acute pharyngolaryngeal dysesthesia;1 3 incidence may be reduced by prolonging duration of infusion.2 7
Delayed sensory neuropathy (e.g., paresthesias, dysesthesias, hypoesthesias, impaired proprioception)1 2 can occur without any prior acute neuropathic event and typically persists for >14 days following oxaliplatin administration;1 symptoms may improve upon discontinuance of therapy.1
Insufficient evidence to support use of any preventive strategy (e.g., intermittent [“stop and go”] oxaliplatin regimens, potential neuromodulatory agents).14
Hematologic Effects
Possible grade 3 or 4 neutropenia, febrile neutropenia, or infection with severe neutropenia.1 Sepsis, neutropenic sepsis, and septic shock, sometimes fatal, also reported.1
Monitor CBCs at baseline, prior to each cycle of therapy, and as clinically indicated.1 Do not administer oxaliplatin until neutrophil counts reach ≥1500/mm3 and platelet counts reach ≥75,000/mm3.1 If sepsis or septic shock occurs, interrupt therapy.1
Posterior Reversible Encephalopathy Syndrome (PRES)
PRES, with or without concomitant hypertension, reported.1 Manifestations include headache, altered mental status, seizure, and visual disturbance (e.g., vision loss, blurred vision).1
If PRES is suspected, perform MRI for diagnostic evaluation.1 If PRES is confirmed. permanently discontinue oxaliplatin.1
Pulmonary Toxicity
Pulmonary fibrosis (sometimes fatal) reported.1 7 If unexplained respiratory manifestations (e.g., nonproductive cough, dyspnea, crackles, radiographic evidence of pulmonary infiltrates) develop, temporarily discontinue therapy until interstitial lung disease and pulmonary fibrosis are excluded.1 If interstitial lung disease or pulmonary fibrosis is confirmed, permanently discontinue oxaliplatin.1
Fatal eosinophilic pneumonia reported.1
Hepatic Effects
Possible elevation of ALT, AST, alkaline phosphatase, or bilirubin concentrations.1 Perform liver function tests (e.g., aminotransferases, bilirubin) at baseline, prior to each cycle of therapy, and as clinically indicated.1 7
Hepatic vascular conditions (e.g., peliosis hepatis, nodular regenerative hyperplasia or sinusoidal changes, perisinusoidal fibrosis, veno-occlusive lesions) reported in patients receiving oxaliplatin in combination with fluorouracil and leucovorin.1 Consider hepatic vascular toxicity in patients with abnormal liver function test results or portal hypertension that cannot be explained by metastases to the liver; investigate as clinically appropriate.1
Cardiac Effects
Prolongation of the QT interval and subsequent ventricular arrhythmia, including torsades de pointes with fatal outcome, reported.1
Avoid in patients with congenital long QT syndrome.1 Monitor ECGs in patients with CHF, bradyarrhythmias, or electrolyte abnormalities and in those who are receiving drugs known to prolong the QT interval (i.e., class IA and III antiarrhythmics).1 Monitor and correct serum electrolyte abnormalities prior to initiation of oxaliplatin and periodically during therapy.1
Rhabdomyolysis
Rhabdomyolysis, which may be fatal, reported.1
If manifestations of rhabdomyolysis (e.g., hematuria, anuria) occur, permanently discontinue oxaliplatin.1
Hemorrhage
Possible thrombocytopenia and hemorrhage (e.g., GI bleeding, hematuria, epistaxis).1 Rapid onset of thrombocytopenia and increased risk of hemorrhage observed in patients experiencing immune-mediated thrombocytopenia; consider discontinuance of oxaliplatin therapy if immune-mediated thrombocytopenia occurs.1 (See Hematologic Effects under Cautions.)
Possible prolongation of PT and INR with possible hemorrhage in patients receiving anticoagulant therapy; monitor patients receiving concomitant oral anticoagulant therapy (e.g., warfarin) more frequently.1
Fetal/Neonatal Morbidity and Mortality
Possible fetal harm; teratogenicity and embryolethality demonstrated in animals.1 Avoid pregnancy during therapy.1 Confirm pregnancy status prior to initiation of therapy.1 Women of reproductive potential should use effective contraceptive methods during therapy and for at least 9 months after the last dose of the drug.1 Men with female partners of reproductive potential should use effective contraceptive methods during therapy and for 6 months after the last dose of the drug.1 If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.1
Impairment of Fertility
Based on animal studies, may impair male and female fertility.1
Specific Populations
Pregnancy
May cause fetal harm.1 (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Not known whether oxaliplatin or its metabolites are distributed into milk or if drug has any effect on milk production or the nursing infant.1 Women should not breast-feed during therapy and for 3 months after the last dose of the drug.1
Pediatric Use
Safety and efficacy not established in pediatric patients.1 7 No substantial antitumor activity reported in 69 pediatric patients with solid tumors.1
Geriatric Use
Clearance of ultrafilterable platinum does not appear to be affected substantially by age.1 However, incidence of certain adverse effects (i.e., diarrhea, dehydration, hypokalemia, granulocytopenia, leukopenia, grade 3 or 4 neutropenia, fatigue, syncope) was increased in geriatric patients compared with younger adults.1 5 7
Efficacy (effect on disease-free survival) of oxaliplatin/fluorouracil/leucovorin versus fluorouracil/leucovorin as adjuvant therapy for colon cancer was inconclusive in patients ≥65 years of age (based on descriptive subset analysis of study data).1
In patients receiving oxaliplatin/fluorouracil/leucovorin as first-line therapy for advanced colorectal cancer, no differences in efficacy observed in patients ≥65 years of age compared with the overall study population.1
In patients receiving the oxaliplatin/fluorouracil/leucovorin regimen for previously treated advanced colorectal cancer, no differences in efficacy observed in patients ≥65 years of age compared with younger adults.1
Renal Impairment
Mild or moderate renal impairment: Increases mean dose-adjusted AUC of unbound platinum following administration of oxaliplatin 85 mg/m2.1 Peak plasma concentrations of unbound platinum not altered.1
Severe renal impairment: Increases mean dose-adjusted AUC and peak plasma concentration of unbound platinum following administration of oxaliplatin 65 mg/m2; dosage adjustment recommended.1
Common Adverse Effects
Adjuvant combination therapy with fluorouracil and leucovorin in patients with colon cancer: Peripheral sensory neuropathy, nausea, vomiting, diarrhea, fatigue, anorexia, pyrexia, neutropenia, thrombocytopenia, anemia, elevated aminotransferase concentrations, elevated alkaline phosphatase concentrations.1
Combination therapy with fluorouracil and leucovorin in patients with previously untreated advanced colorectal cancer: Adverse neurologic effects (i.e., neuropathy, including paresthesia, pharyngo-laryngeal dysesthesias), adverse GI effects (i.e., nausea, diarrhea, vomiting, stomatitis, anorexia, constipation, abdominal pain), fatigue, cough, alopecia, leukopenia, neutropenia, thrombocytopenia, anemia.1
Combination therapy with fluorouracil and leucovorin in patients with previously treated advanced colorectal cancer: Adverse neurologic effects (i.e., neuropathy, including acute or persistent neuropathy), adverse GI effects (nausea, vomiting, diarrhea, stomatitis, abdominal pain, anorexia), fatigue, pyrexia, dyspnea, constipation, anemia, leukopenia, neutropenia, thrombocytopenia, elevated aminotransferase concentrations.1
Drug Interactions
Not metabolized by and does not inhibit CYP isoenzymes.1
Nephrotoxic Drugs
Potential pharmacokinetic interaction (decreased clearance of platinum-containing compounds); however, this interaction has not been specifically studied.1 Avoid concomitant use with other nephrotoxic drugs.1
Protein-bound Drugs
Pharmacokinetic interaction with highly protein-bound drugs unlikely; platinum displacement not observed in vitro.1 7
Drugs Affecting Hepatic Microsomal Enzymes
Pharmacokinetic interaction with drugs metabolized by CYP isoenzymes or those that induce or inhibit these isoenzymes unlikely.1 However, no studies have been conducted.1
Drugs that Prolong the QT Interval
Avoid concomitant use with other drugs known to prolong the QT interval (i.e., class IA and III antiarrhythmics).1 (See Cardiac Effects under Cautions.)
Specific Drugs
|
Drug |
Interaction |
Comment |
|---|---|---|
|
Anticoagulants, oral (warfarin) |
Possible prolonged PT and INR; hemorrhage reported1 |
More frequent monitoring required1 |
|
Erythromycin |
Platinum displacement from protein binding sites not observed in vitro1 |
|
|
Fluorouracil |
Pharmacokinetic interaction unlikely when recommended dosages and administration schedule are used1 2 Potential pharmacokinetic interaction (increased plasma fluorouracil concentrations) when used concomitantly with oxaliplatin dosages greater than recommended (e.g., 130 mg/m2) at intervals of 3 weeks1 7 |
|
|
Granisetron |
Platinum displacement from protein binding sites not observed in vitro1 |
|
|
Irinotecan |
Pharmacokinetic interaction unlikely2 |
|
|
Paclitaxel |
Platinum displacement from protein binding sites not observed in vitro1 |
|
|
Salicylates |
Platinum displacement from protein binding sites not observed in vitro1 |
|
|
Topotecan |
Pharmacokinetic interaction unlikely2 |
|
|
Valproate sodium |
Platinum displacement from protein binding sites not observed in vitro1 |
Oxaliplatin Pharmacokinetics
Undergoes rapid and extensive nonenzymatic biotransformation to numerous platinum-containing transient reactive intermediates.1 2 Pharmacokinetic parameters generally expressed in terms of platinum-containing complexes rather than parent compound.2
Absorption
Special Populations
Increased mean dose-adjusted AUC of unbound platinum by 40 or 95% in patients with mild (Clcr of 50–80 mL/minute) or moderate (Clcr of 30–49 mL/minute) renal impairment, respectively, following administration of oxaliplatin 85 mg/m2.1 Mean dose-adjusted peak plasma concentration of unbound platinum not altered.1
Increased mean dose-adjusted AUC and peak plasma concentration of unbound platinum by 342 or 38%, respectively, in patients with severe renal impairment receiving oxaliplatin 65 mg/m2 compared with patients with normal renal function receiving oxaliplatin 85 mg/m2.1
Distribution
Extent
Following a 2-hour IV infusion, 85% of administered platinum is rapidly distributed into tissues or eliminated in urine; approximately 15% of administered platinum is present in systemic circulation.1
No evidence of accumulation in plasma following usual dosage;1 2 possible progressive accumulation in erythrocytes.2
Not known whether oxaliplatin or its metabolites are distributed into milk.1
Plasma Protein Binding
>90% irreversibly bound to plasma proteins (principally albumin and γ-globulins).1
Elimination
Metabolism
Undergoes rapid and extensive nonenzymatic biotransformation; no evidence of CYP-mediated metabolism in vitro.1
Elimination Route
Eliminated principally by renal excretion;1 2 renal clearance of ultrafilterable platinum appears to be directly proportional to GFR.1
Following 2-hour IV infusion, approximately 54 or 2% of platinum-containing derivatives is excreted in urine and feces, respectively, within 5 days.1
Half-life
Distribution and elimination of platinum-containing derivatives appears to be triphasic, with 2 relatively short distribution phases with half-lives of approximately 0.43 and 16.8 hours, respectively, and a long elimination phase with a half-life of approximately 392 hours.1
Stability
Storage
Parenteral
Powder for Injection
25°C (may be exposed to 15–30°C).1
Following reconstitution, store in original vial at 2–8°C; discard after 24 hours.1
Following dilution, store at 2–8°C for up to 24 hours or at room temperature (i.e., 20–25°C) for up to 6 hours.1
Concentrate for Injection
25°C (may be exposed to 15–30°C).1 Do not freeze.1
Protect concentrate from light (keep in original outer carton).1 Not necessary to protect diluted solution from light.1
Following dilution, store at 2–8°C for up to 24 hours or at room temperature (i.e., 20–25°C) for up to 6 hours.1
Compatibility
Aluminum reportedly causes degradation of platinum compounds; do not use needles or IV administration sets that contain aluminum parts for preparation or administration.1
Parenteral
Solution Compatibility
Drug Compatibility
|
Compatible |
|---|
|
Bumetanide |
|
Buprenorphine HCl |
|
Butorphanol tartrate |
|
Calcium gluconate |
|
Carboplatin |
|
Chlorpromazine HCl |
|
Cyclophosphamide |
|
Dexamethasone sodium phosphate |
|
Diphenhydramine HCl |
|
Dobutamine HCl |
|
Docetaxel |
|
Dolasetron mesylate |
|
Dopamine HCl |
|
Doxorubicin HCl |
|
Droperidol |
|
Enalaprilat |
|
Epirubicin HCl |
|
Etoposide phosphate |
|
Famotidine |
|
Fentanyl citrate |
|
Furosemide |
|
Gemcitabine HCl |
|
Granisetron HCl |
|
Haloperidol lactate |
|
Heparin sodium |
|
Hydrocortisone sodium succinate |
|
Hydromorphone HCl |
|
Hydroxyzine HCl |
|
Ifosfamide |
|
Irinotecan HCl |
|
Leucovorin calcium |
|
Lorazepam |
|
Magnesium sulfate |
|
Mannitol |
|
Meperidine HCl |
|
Mesna |
|
Methotrexate sodium |
|
Methylprednisolone sodium succinate |
|
Metoclopramide HCl |
|
Mitoxantrone HCl |
|
Morphine sulfate |
|
Nalbuphine HCl |
|
Ondansetron HCl |
|
Paclitaxel |
|
Palonosetron HCl |
|
Potassium chloride |
|
Prochlorperazine edisylate |
|
Promethazine HCl |
|
Ranitidine HCl |
|
Theophylline |
|
Topotecan HCl |
|
Verapamil HCl |
|
Vincristine sulfate |
|
Vinorelbine tartrate |
|
Incompatible |
|
Alkaline drugs or media (e.g., basic solutions of fluorouracil)1 |
|
Diazepam |
Actions
-
Antineoplastic agent;1 2 consists of a platinum atom complexed with 1,2-diaminocyclohexane (DACH) and a labile oxalate ligand.1
-
Must undergo nonenzymatic activation before antineoplastic activity occurs.1 7 In physiologic solutions, the labile oxalate ligand presumably is displaced, forming several transient reactive complexes (e.g., monoaquo DACH platinum, diaquo DACH platinum).1 2 These complexes covalently bind to specific DNA base sequences, producing intrastrand and interstrand DNA cross-links, which are thought to inhibit DNA replication and transcription.1 2
-
Cycle-phase nonspecific.1
-
Exhibits antitumor activity against colon carcinoma in vivo.1 Exhibits synergistic antiproliferative activity with fluorouracil.1 2
-
Risk of hypersensitivity reactions.1 Importance of seeking immediate medical attention if signs of severe hypersensitivity reaction (e.g., chest tightness, shortness of breath, wheezing, dizziness, faintness, angioedema) occur.1
-
Risk of neuropathy.1 Instruct patients to avoid cold drinks and use of ice (e.g., for mucositis prophylaxis) and to cover skin prior to exposure to cold temperature or cold objects since such exposure can precipitate or exacerbate acute sensory neuropathy.1 Importance of reading manufacturer’s patient information for further instructions to minimize exposure to cold temperature or cold objects.1
-
Risk of anemia, leukopenia, neutropenia, and thrombocytopenia; importance of informing a clinician immediately if bleeding, fever (particularly if associated with persistent diarrhea), or evidence of infection develops.1
-
Risk of posterior reversible encephalopathy syndrome and visual abnormalities (e.g., transient vision loss); such effects may affect ability to drive or operate machinery.1
-
Risk of pulmonary toxicity.1 Importance of promptly informing clinician of any persistent or recurrent respiratory symptoms (e.g., nonproductive cough, dyspnea).1
-
Risk of hepatotoxicity.1 Importance of informing clinician if symptoms of hepatotoxicity occur.1
-
Risk of QT-interval prolongation.1 Importance of informing clinician if symptoms of QT-interval prolongation (e.g., syncope) occur.1
-
Risk of rhabdomyolysis.1 Importance of promptly informing clinician if new or worsening signs or symptoms of rhabdomyolysis (e.g., dark urine, anuria, urinary retention) occur.1
-
Risk of persistent vomiting, diarrhea, or signs of dehydration.1
-
Risk of fetal harm.1 Necessity of advising women of reproductive potential that they should use effective contraceptive methods while receiving the drug and for 9 months after the last dose of the drug.1 Importance of advising men who are partners with women of reproductive potential to use effective methods of contraception while receiving the drug and for 6 months after the last dose of the drug.1 Importance of patients informing their clinicians if they are pregnant or think they may be pregnant.1 If pregnancy occurs, advise patient of potential risk to fetus.1
-
Importance of advising women to avoid breast-feeding while receiving oxaliplatin therapy and for 3 months after the last dose of the drug.1
-
Risk of impaired male and female fertility.1
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as concomitant illness.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection, for IV infusion |
50 mg* |
Oxaliplatin |
|
|
100 mg* |
Oxaliplatin |
|||
|
For injection concentrate, for IV infusion |
5 mg/mL (50 and 100 mg) |
Eloxatin |
Sanofi-Aventis |
|
|
5 mg/mL (50, 100, and 200 mg* |
Oxaliplatin |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 24, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Sanofi-Aventis. Eloxatin (oxaliplatin) for injection prescribing information. Bridgewater, NJ; 2020 Apr.
2. Culy CR, Clemett D, Wiseman LR. Oxaliplatin: a review of its pharmacological properties and clinical efficacy in metastatic colorectal cancer and its potential in other malignancies. Drugs. 2000; 60:895-924. https://pubmed.ncbi.nlm.nih.gov/11085200
3. de Gramont A, Figer A, Seymour M et al. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol. 2000 Aug;18:2938-47.
4. Giacchetti S, Perpoint B, Zidani R et al. Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil-leucovorin as first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2000 Jan;18:136-47.
5. Tabah-Fisch I, Maindrault-Goebel F, Benavides M et al. Oxaliplatin/5FU/LV is feasible, safe and active in elderly colorectal cancer (CRC) patients. Proceedings of ASCO. 2002; Abstract No. 556.
6. Grothey A, Deschler B, Kroening H et al. Phase III study of bolus 5-fluorouracil (5-FU)/folinic acid (FA) (Mayo) vs weekly high-dose 24-h 5-FU infusion/FA + oxaliplatin (OXA) (FUFOX) in advanced colorectal cancer (ACRC). Proceedings of ASCO. 2002; Abstract No. 512.
7. Sanofi-Synthelabo, New York, NY: Personal communication.
8. Goldberg RM, Morton RF, Sargent DJ et al. Oxaliplatin or CPT-11 + 5FU/leucovorin or oxaliplatin + CPT-11 in advanced colorectal cancer (ACRC): efficacy and safety results from a North American Gastrointestinal Intergroup Study (N9741). Abstract #6 presented at Perspectives in Colorectal Cancer, a Consensus Meeting, Fourth International Conference, Barcelona, June 2002.
9. André T, Boni C, Mounedji-Boudiaf L et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med. 2004; 350:2343-51. https://pubmed.ncbi.nlm.nih.gov/15175436
10. André T, Boni C, Navarro M et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol. 2009; 27:3109-16. https://pubmed.ncbi.nlm.nih.gov/19451431
11. Goldberg RM, Sargent DJ, Morton RF et al. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004; 22:23-30. https://pubmed.ncbi.nlm.nih.gov/14665611
12. Cheeseman SL, Joel SP, Chester JD et al. A ’modified de Gramont’ regimen of fluorouracil, alone and with oxaliplatin, for advanced colorectal cancer. Br J Cancer. 2002; 87:393-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2376131/ https://pubmed.ncbi.nlm.nih.gov/12177775
14. Saif MW, Reardon J. Management of oxaliplatin-induced peripheral neuropathy. Ther Clin Risk Manag. 2005; 1:249-58. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1661634/ https://pubmed.ncbi.nlm.nih.gov/18360567
15. Gamelin L, Boisdron-Celle M, Delva R et al. Prevention of oxaliplatin-related neurotoxicity by calcium and magnesium infusions: a retrospective study of 161 patients receiving oxaliplatin combined with 5-Fluorouracil and leucovorin for advanced colorectal cancer. Clin Cancer Res. 2004; 10:4055-61. https://pubmed.ncbi.nlm.nih.gov/15217938
16. Nikcevich, DA, Grothey A, Sloan JA et al. Effect of intravenous calcium and magnesium (IV CaMg) on oxaliplatin-induced sensory neuropathy (sNT) in adjuvant colon cancer: results of the phase III placebo-controlled, double-blind NCCTG trial N0347. J Clin Oncol. 2008; 26: Abstract 4009 (presented at the 2008 ASCO Annual Meeting).
17. Gamelin L, Boisdron-Celle M, Morel A et al. Oxaliplatin-related neurotoxicity: interest of calcium-magnesium infusion and no impact on its efficacy. J Clin Oncol. 2008; 26:1188-9; author reply 1189-90. https://pubmed.ncbi.nlm.nih.gov/18309961
18. Hochster HS, Grothey A, Shplisky A et al. Effect of intravenous (IV) calcium and magnesium (Ca/Mg) versus placebo on reponse to FOLFOX + bevacizumab (BEV) in the CONcePT trial. Presented at the ASCO 2008 Gastrointestinal Cancers Symposium. From ASCO website. Abstract 280. Accessed 2009 Jul 9. http://www.asco.org
19. A phase III randomized, placebo-controlled, double-blind study of intravenous calcium/magnesium to prevent oxaliplatin-induced sensory neuropathy. From ClinicalTrials.gov registry. Accessed 2009 Jul 13. http://www.clinicaltrials.gov/ct2/show/NCT00316914?term=N04C7&rank=1
20. CONCEPT: Phase IV, randomized, prospective, multicenter comparison of intermittent schedule of oxaliplatin combined with FOLFOX/bevacizumab vs conventional mode of administration of FOLFOX/bevacizumab + neuroprophylaxis with calcium/magnesium for optimization of first-line therapy of metastatic colorectal cancer. From ClinicalTrials.gov registry. Accessed 2009 Jul 16. http://www.clinicaltrials.gov/ct2/show/NCT00129870?term=CONcePT&rank=19
21. O’Dea D, Handy CM, Wexler A. Ocular changes with oxaliplatin. Clin J Oncol Nurs. 2006; 10:227-9. https://pubmed.ncbi.nlm.nih.gov/16708705
22. Leonard GD, Wright MA, Quinn MG et al. Survey of oxaliplatin-associated neurotoxicity using an interview-based questionnaire in patients with metastatic colorectal cancer. BMC Cancer. 2005; 5:116. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1266024/ https://pubmed.ncbi.nlm.nih.gov/16168057
23. André T, de Gramont A, Vernerey D et al. Adjuvant Fluorouracil, Leucovorin, and Oxaliplatin in Stage II to III Colon Cancer: Updated 10-Year Survival and Outcomes According to BRAF Mutation and Mismatch Repair Status of the MOSAIC Study. J Clin Oncol. 2015; 33:4176-87. https://pubmed.ncbi.nlm.nih.gov/26527776
24. Breckenridge Pharmaceutical, Inc. Oxaliplatin for injection prescribing information. Berlin, CT; 2019 May.
10001. Haller DG, Tabernero J, Maroun J et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol. 2011; 29:1465-71. https://pubmed.ncbi.nlm.nih.gov/21383294
10002. Schmoll HJ, Tabernero J, Maroun J et al. Capecitabine Plus Oxaliplatin Compared With Fluorouracil/Folinic Acid As Adjuvant Therapy for Stage III Colon Cancer: Final Results of the NO16968 Randomized Controlled Phase III Trial. J Clin Oncol. 2015; 33:3733-40. https://pubmed.ncbi.nlm.nih.gov/26324362
10003. Schmoll HJ, Cartwright T, Tabernero J et al. Phase III trial of capecitabine plus oxaliplatin as adjuvant therapy for stage III colon cancer: a planned safety analysis in 1,864 patients. J Clin Oncol. 2007; 25:102-9. https://pubmed.ncbi.nlm.nih.gov/17194911
10004. Yothers G, O'Connell MJ, Allegra CJ et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses. J Clin Oncol. 2011; 29:3768-74. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3188282/ https://pubmed.ncbi.nlm.nih.gov/21859995
10006. Pectasides D, Karavasilis V, Papaxoinis G et al. Randomized phase III clinical trial comparing the combination of capecitabine and oxaliplatin (CAPOX) with the combination of 5-fluorouracil, leucovorin and oxaliplatin (modified FOLFOX6) as adjuvant therapy in patients with operated high-risk stage II or stage III colorectal cancer. BMC Cancer. 2015; 15:384. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4445286/ https://pubmed.ncbi.nlm.nih.gov/25956750
10007. AHFS final determination of medical acceptance: Off-label use of capecitabine in combination with oxaliplatin for the adjuvant treatment of stage III colon cancer. Published November 9, 2016
10008. Grothey A, Sobrero AF, Shields AF et al. Duration of Adjuvant Chemotherapy for Stage III Colon Cancer. N Engl J Med. 2018; 378:1177-1188. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC6426127/ https://pubmed.ncbi.nlm.nih.gov/29590544
10009. Lieu C, Kennedy EB, Bergsland E et al. Duration of Oxaliplatin-Containing Adjuvant Therapy for Stage III Colon Cancer: ASCO Clinical Practice Guideline. J Clin Oncol. 2019; 37:1436-1447. https://pubmed.ncbi.nlm.nih.gov/30986117
10010. Oxaliplatin, Leucovorin Calcium, and Fluorouracil With or Without Celecoxib in Treating Patients With Stage III Colon Cancer Previously Treated With Surgery. From ClinicalTrials.gov registry. Accessed 2020 Aug 4.
10011. André T, Vernerey D, Mineur L et al. Three Versus 6 Months of Oxaliplatin-Based Adjuvant Chemotherapy for Patients With Stage III Colon Cancer: Disease-Free Survival Results From a Randomized, Open-Label, International Duration Evaluation of Adjuvant (IDEA) France, Phase III Trial. J Clin Oncol. 2018; 36:1469-1477. https://pubmed.ncbi.nlm.nih.gov/29620995
10012. Sobrero A, Lonardi S, Rosati G et al. FOLFOX or CAPOX in Stage II to III Colon Cancer: Efficacy Results of the Italian Three or Six Colon Adjuvant Trial. J Clin Oncol. 2018; 36:1478-1485. https://pubmed.ncbi.nlm.nih.gov/29620994
10013. Combination Chemotherapy After Surgery in Treating Patients With High-Risk Stage II or Stage III Colorectal Cancer. From ClinicalTrials.gov registry. Accessed 2020 Aug 4.
10014. Yoshino T, Yamanaka T, Oki E et al. Efficacy and Long-term Peripheral Sensory Neuropathy of 3 vs 6 Months of Oxaliplatin-Based Adjuvant Chemotherapy for Colon Cancer: The ACHIEVE Phase 3 Randomized Clinical Trial. JAMA Oncol. 2019; https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC6743062/ https://pubmed.ncbi.nlm.nih.gov/31513248
10015. Souglakos J, Boukovinas I, Kakolyris S et al. Three- versus six-month adjuvant FOLFOX or CAPOX for high-risk stage II and stage III colon cancer patients: the efficacy results of Hellenic Oncology Research Group (HORG) participation to the International Duration Evaluation of Adjuvant Chemotherapy (IDEA) project. Ann Oncol. 2019; 30:1304-1310. https://pubmed.ncbi.nlm.nih.gov/31228203
10016. André T, Iveson T, Labianca R et al. The IDEA (International Duration Evaluation of Adjuvant Chemotherapy) Collaboration: Prospective Combined Analysis of Phase III Trials Investigating Duration of Adjuvant Therapy with the FOLFOX (FOLFOX4 or Modified FOLFOX6) or XELOX (3 versus 6 months) Regimen for Patients with Stage III Colon Cancer: Trial Design and Current Status. Curr Colorectal Cancer Rep. 2013; 9:261-269. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC3766516/ https://pubmed.ncbi.nlm.nih.gov/24032000
10017. André T, Meyerhardt J, Iveson T et al. Effect of duration of adjuvant chemotherapy for patients with stage III colon cancer (IDEA collaboration): final results from a prospective, pooled analysis of six randomised, phase 3 trials. Lancet Oncol. 2020; 21:1620-1629. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC7786835/ https://pubmed.ncbi.nlm.nih.gov/33271092
10018. AHFS final determination of medical acceptance: Off-label use of capecitabine in combination with oxaliplatin for the adjuvant treatment of stage III colon cancer. Published October 24, 2022.
a. ASHP Injectable Drug Information. Oxaliplatin. American Society of Health-System Pharmacists; Updated 31 Jan 2020. Accessed 5 Nov 2020. https://injectables.ashp.org
Related/similar drugs
Frequently asked questions
- What is the FOLFOX chemo regimen and is it effective?
- How do you manage neuropathy from chemo?
- What is the CAPOX (XELOX) chemotherapy regimen?
- Chemo side effects: What should I expect and how to cope?
- What is the FLOT chemotherapy regimen and how does it work?
- What is chemo brain and how long does it last?
- What is FOLFIRINOX regimen and how is it used?
- How long does oxaliplatin stay in your system?
- How soon can you start chemo after port placement?
More about oxaliplatin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (5)
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: alkylating agents
- Breastfeeding
- En español