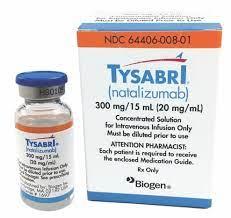
Natalizumab (Monograph)
Brand names: Tysabri, Tyruko
Drug class: Monoclonal Antibodies
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for natalizumab products to ensure that the benefits outweigh the risks. The REMS may apply to one or more preparations of natalizumab and consists of the following: medication guide, elements to assure safe use, and implementation system. See https://www.accessdata.fda.gov/scripts/cder/rems/.
Warning
- Progressive Multifocal Leukoencephalopathy
-
Increased risk of progressive multifocal leukoencephalopathy (PML), an opportunistic viral infection of the brain; usually leads to death or severe disability.
-
Risk factors include duration of therapy (e.g., >2 years), prior use of immunosuppressants, and presence of anti-JC virus antibodies. When initiating and continuing treatment with natalizumab, consider these risk factors in the context of expected benefit.
-
Because of risk of PML, available only through a restricted distribution program (TOUCH Prescribing Program for Tysabri and TYRUKO REMS for Tyruko).
-
Monitor patients during therapy for any new signs or symptoms suggestive of PML; immediately withhold the drug at first such sign or symptom.
Introduction
Biologic response modifier; a recombinant humanized anti-α4-integrin monoclonal antibody.
Natalizumab-sztn (Tyruko) is biosimilar to natalizumab (Tysabri). A biosimilar is a biological that is highly similar to an FDA-licensed reference biological with the exception of minor differences in clinically inactive components and for which there are no clinically meaningful differences in safety, purity, or potency. Biosimilars are approved through an abbreviated licensure pathway that establishes biosimilarity between proposed biological and reference biological but does not independently establish safety and effectiveness of the proposed biological. In order to be considered an interchangeable biosimilar, a biological product must meet additional requirements beyond demonstrating biosimilarity to its reference product. The currently available natalizumab biosimilar does not have interchangeable data at this time.
In this monograph, unless otherwise stated, the term "natalizumab products" refers to natalizumab (the reference drug) and its biosimilar (natalizumab-sztn).
Uses for Natalizumab
Multiple Sclerosis (MS)
Monotherapy for relapsing forms of MS, to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease in adults.
Natalizumab is one of several disease-modifying therapies used in the management of relapsing forms of MS. Although not curative, these therapies have all been shown to modify several measures of disease activity, including relapse rates, new or enhancing MRI lesions, and disability progression.
The American Academy of Neurology (AAN) recommends that disease-modifying therapy be offered to patients with relapsing forms of MS who have had recent relapses and/or MRI activity. Clinicians should consider adverse effects, tolerability, method of administration, safety, efficacy, and cost of the drugs in addition to patient preferences when selecting an appropriate therapy.
Because of risk of PML, consider whether expected benefits of natalizumab are sufficient to offset this risk when initiating or continuing therapy. Because a few cases of PML have occurred in patients receiving natalizumab concomitantly with interferon beta-1a, the drug is currently restricted to use as monotherapy.
Crohn Disease
Used to induce and maintain clinical response and remission in adults with moderately to severely active Crohn disease with evidence of inflammation who have had an inadequate response to or who do not tolerate conventional therapies and inhibitors of tumor necrosis factor (TNF; TNF-α).
Do not use in combination with immunosuppressants (e.g., mercaptopurine, azathioprine, cyclosporine, methotrexate) or TNF inhibitors in patients with Crohn disease, because of potential for increased risk of PML and other infections.
Aminosalicylates may be used in patients receiving natalizumab.
American College of Gastroenterology guideline states that for moderate to severe disease/moderate to high risk disease, natalizumab is more effective than placebo and should be considered for induction of symptomatic response and remission in patients with Crohn disease.
American Gastroenterological Association guideline suggests against use of natalizumab over no treatment for induction and maintenance of remission in adult outpatients with moderate to severe Crohn disease due to evidence of harm from PML and availability of other drugs without this concern.
Natalizumab Dosage and Administration
General
Patient Monitoring
-
Monitor patients for signs and symptoms of infection during therapy.
-
Assess patients for bleeding abnormalities.
-
Monitor for any new signs or symptoms that may be suggestive of PML.
-
Monitor for the development of immune reconstitution inflammatory syndrome (IRIS).
-
Monitor patients during infusion. Observe patients for 1 hour after the infusion is complete for the first 12 infusions. For patients who have received 12 infusions without evidence of hypersensitivity, the need for subsequent monitoring should be guided by clinical judgment.
-
Obtain a CBC in neonates with in utero exposure to natalizumab.
REMS
-
Because of risk of PML, natalizumab is available only through a restricted distribution program (TOUCH Prescribing Program for Tysabri and TYRUKO REMS program for Tyruko ).
-
Clinicians, pharmacies, infusion centers, and patients must enroll in and meet all conditions of the TOUCH or TYRUKO REMS program before they can prescribe, dispense, infuse, or receive natalizumab.
-
Information about TOUCH program (MS TOUCH and CD TOUCH) is available at 800-456-2255 or [Web]. Information about the TYRUKO REMS program is available at 800-489-7856 or [Web].
Administration
IV Administration
Administer by IV infusion. Do not administer by rapid IV injection.
Do not infuse or admix with any other drug.
Use of filtration devices during IV infusion not evaluated.
Following completion of infusion, flush infusion set with 0.9% sodium chloride injection.
Dilution
The concentrate for injection containing 300 mg/15 mL must be diluted in 0.9% sodium chloride prior to IV infusion. Do not use other IV diluents.
Withdraw 15 mL of the concentrate from a single-use vial and add to 100 mL of 0.9% sodium chloride injection (final concentration: 2.6 mg/mL). Gently invert diluted solution to mix completely; do not shake.
Allow refrigerated solution to warm to room temperature prior to administration.
Rate of Administration
Administer IV infusions over approximately 1 hour (infusion rate approximately 5 mg/minute).
Dosage
Adults
Multiple Sclerosis
IV
300 mg once every 4 weeks by IV infusion.
Crohn Disease
IV
300 mg once every 4 weeks.
In patients receiving chronic oral corticosteroid therapy, start tapering corticosteroid dosage as soon as a therapeutic benefit of natalizumab occurs. Discontinue natalizumab if patient cannot be tapered off oral corticosteroids within 6 months of initiating natalizumab. Consider discontinuing natalizumab in patients who require additional corticosteroid use that exceeds 3 months in a calendar year to control Crohn disease other than the 6-month corticosteroid taper.
Discontinue natalizumab if no therapeutic benefit is evident by 12 weeks of induction therapy.
Special Populations
No special population recommendations at this time for patients with hepatic or renal impairment or geriatric patients.
Cautions for Natalizumab
Contraindications
-
Known hypersensitivity to natalizumab products.
-
Current or previous history of PML.
Warnings/Precautions
Warnings
Progressive Multifocal Leukoencephalopathy
PML, an opportunistic viral infection of the brain caused by the JC virus, reported in patients receiving natalizumab (see Boxed Warning). As of January 2012, 201 cases reported among 96,582 patients treated with natalizumab worldwide; cases continue to be reported during postmarketing surveillance.
PML typically occurs in immunocompromised patients (e.g., patients with HIV infection) and usually leads to death or severe disability.
Has been reported in patients receiving natalizumab who were recently or concomitantly treated with immunomodulators or immunosuppressants (i.e., interferon beta-1a in MS patients, infliximab and azathioprine in Crohn patients); also reported in patients receiving natalizumab without concomitant immunomodulatory drugs.
The 3 factors known to increase risk of PML in natalizumab-treated patients are longer treatment duration (especially >2 years), prior treatment with immunosuppressants (e.g., mitoxantrone, azathioprine, methotrexate, cyclophosphamide, mycophenolate mofetil), and presence of anti-JC virus antibodies.
Generally, not recommended in patients receiving chronic immunosuppressant or immunomodulatory therapy or in those with systemic medical conditions that result in clinically important compromised immune system.
Consider testing for anti-JC virus antibody status (using an analytically and clinically validated immunoassay). In patients undergoing plasma exchange, do not perform anti-JC virus antibody test during or for at least 2 weeks after the procedure to avoid false-negative results. To avoid false-positive results in patients receiving IV immunoglobulin, allow at least 6 months to elapse before performing antibody test.
Positive anti-JC virus antibody test indicates individual has been exposed to JC virus in the past. For purposes of risk assessment, consider patient anti-JC virus antibody positive if they had a positive test at any time, regardless of results of prior or subsequent anti-JC virus antibody tests.
Negative anti-JC virus antibody test indicates exposure to JC virus has not been detected. Such patients are still at risk for PML because of potential for subsequent JC virus infection or possibility of false-negative results for anti-JC virus antibody. Periodically retest patients with negative anti-JC virus antibody test.
Interventions that can reliably prevent or adequately treat PML not known.
Prior to initiating natalizumab in patients with MS, perform baseline MRI scan since this may help differentiate subsequent MS symptoms from PML. Baseline brain MRI scan also may be useful in patients with Crohn disease, but baseline brain lesions that could cause diagnostic difficulty are uncommon in these patients.
Monitor patients for any new signs or symptoms suggestive of PML (i.e., progressive weakness on one side of the body; clumsiness of limbs; disturbance of vision; changes in thinking, memory, and orientation leading to confusion and personality changes); seizures and headache also reported rarely. The progression of deficits usually leads to death or severe disability over weeks or months.
Immediately withhold natalizumab at the first sign or symptom of PML and perform appropriate diagnostic evaluation. MRI signs may be apparent before clinical manifestations develop; any suspicious findings on MRI should be followed by further evaluation.
Do not use anti-JC virus antibody test to diagnose PML. An evaluation that includes a gadolinium-enhanced MRI brain scan and, when indicated, CSF analysis for JC viral DNA recommended to diagnose PML. If clinical suspicion remains despite an initial negative evaluation for PML, do not reinitiate natalizumab until the evaluation has been repeated and confirmed.
Because of risk of PML, natalizumab products are available only through a restricted distribution program (Tysabri: TOUCH Prescribing Program and Tyruko: TYRUKO REMS).
Promptly report any case of PML, serious opportunistic infection, atypical infection, or death to Biogen for Tysabri at 800-456-2255 or Sandoz for Tyruko at 800-525-8747 and to FDA’s MedWatch program at 800-332-1088.
Immune reconstitution inflammatory syndrome (IRIS) reported in majority of natalizumab-treated patients who discontinued the drug after developing PML; not reported to date when natalizumab discontinued for reasons unrelated to PML.
IRIS is a severe inflammatory response occurring during or after immune system recovery; usually presents as clinical decline (sometimes after apparent clinical improvement) and may progress rapidly, leading to serious neurologic complications or death. In MS patients with PML who developed IRIS after discontinuing natalizumab, IRIS generally developed within days to several weeks after the patient received plasma exchange or immunoadsorption to enhance natalizumab removal.
Monitor patients for IRIS development; if IRIS occurs, treat the associated inflammation as appropriate.
Other Warnings and Precautions
Herpes Infections
Natalizumab increases risk of encephalitis and meningitis caused by herpes simplex and varicella zoster viruses. Serious, life-threatening, and sometimes fatal cases reported in patients with MS administered natalizumab. Duration of therapy prior to infection onset ranged from a few months to several years. Monitor patients for signs and symptoms of meningitis and encephalitis. If herpes encephalitis or meningitis occurs, discontinue natalizumab and initiate appropriate treatment.
An increased risk of acute retinal necrosis (ARN) reported in patients administered natalizumab. Refer patients presenting with eye symptoms (e.g., decreased visual acuity, redness, eye pain) for retinal screening for ARN. Some ARN cases occurred in patients with CNS herpes infections; serious cases have led to blindness. Following ARN diagnosis, consider natalizumab discontinuation.
Hepatotoxicity
Clinically important liver dysfunction (e.g., elevated hepatic enzymes, elevated total bilirubin) reported as early as 6 days after administration of the first dose of natalizumab and also after multiple doses. Liver dysfunction may recur upon rechallenge indicating that natalizumab caused the injury.
Elevated transaminase levels together with elevated bilirubin (without evidence of obstruction) generally is recognized as an important predictor of severe liver injury that may lead to death or the need for liver transplantation.
Discontinue natalizumab in patients with jaundice or other evidence of clinically important liver injury (e.g., laboratory evidence).
Hypersensitivity/Antibody Formation
Serious hypersensitivity reactions (e.g., anaphylaxis/anaphylactoid reaction) reported in <1% of patients; usually occurred within 2 hours after initiation of IV infusion and generally associated with antibodies to the drug.
If hypersensitivity reactions (e.g., anaphylaxis, urticaria, dizziness, fever, rash, rigors, pruritus, nausea, flushing, hypotension, dyspnea, chest pain) occur, discontinue immediately and initiate appropriate therapy. Do not reinitiate in any patient who experienced a hypersensitivity reaction to the drug. Consider possibility of anti-natalizumab antibodies in patients who have hypersensitivity reactions.
Antibodies to natalizumab may develop. Antibodies against natalizumab may be neutralizing and persistent antibody-positivity may be associated with decreased natalizumab serum concentrations, decreased efficacy, increased rate of myalgia, hypertension, dyspnea, anxiety and tachycardia, and increased risk of infusion-related reactions.
Long-term immunogenicity remains to be determined; effects of low to moderate levels of antibodies against natalizumab not known. Patients who receive natalizumab for a short period (1–2 infusions) followed by an extended period without such treatment may be at higher risk of developing anti-natalizumab antibodies and/or hypersensitivity reactions upon re-exposure.
Consider testing for presence of antibodies to natalizumab in patients who wish to resume treatment following an interruption in therapy. Patients who have tested negative for antibodies against natalizumab prior to retreatment have a risk of antibody development with retreatment that is similar to natalizumab-naïve patients. Perform sequential antibody testing if presence of persistent antibodies suspected. Antibodies detected early in treatment course (e.g., within first 6 months) may be transient and disappear with continued use; repeat testing at 3 months after initial positive result to confirm persistent antibodies. Consider overall benefits and risks of the drug in patients who have persistent antibodies.
Immunosuppression and Infections
Possible increased risk of infections, including opportunistic infections (e.g., PML).
Pneumonia, urinary tract infections (sometimes severe), influenza, gastroenteritis, vaginal infections, tooth infections, tonsillitis or pharyngitis, and herpes infections reported in MS patients. Most infections were mild to moderate and did not require interruption of therapy. At least 1 case of cryptosporidial gastroenteritis with a prolonged course reported in an MS patient.
Pneumocystis jiroveci (formerly P. carinii) pneumonia, pulmonary Mycobacterium avium complex (MAC) infections, bronchopulmonary aspergillosis, and Burkholderia cepacia infection reported rarely in patients with Crohn disease. Increased incidence of infections observed in patients receiving corticosteroids concomitantly with natalizumab; however, incidence similar to that observed in patients receiving corticosteroids alone.
Concomitant use of natalizumab and antineoplastic agents, immunosuppressive agents, or immunomodulating agents may further increase risk of infections, including PML and other opportunistic infections. Safety and efficacy of natalizumab in combination with antineoplastic, immunosuppressive, or immunomodulating agents not established.
Laboratory Test Abnormalities
Natalizumab induced increases in circulating lymphocytes, monocytes, eosinophils, basophils, and nucleated red blood cells. Observed changes persisted during exposure, but were reversible, returning to baseline usually within 16 weeks after last dose. Natalizumab also induced mild decreases in hemoglobin levels that were frequently transient.
Hematological Abnormalities
Thrombocytopenia, including immune thrombocytopenic purpura (ITP), reported. Symptoms may include easy bruising, abnormal bleeding, and petechiae. If thrombocytopenia suspected, discontinue natalizumab.
Cases of neonatal thrombocytopenia and anemia reported in newborns with in utero natalizumab exposure. Obtain CBC in neonates with in utero exposure.
Immunizations
No data available on vaccination effects or on secondary transmission of infection by live vaccines in patients administered natalizumab.
Specific Populations
Pregnancy
No adequate data on risk of major birth defects, miscarriage, or other adverse maternal outcomes associated with use of natalizumab during pregnancy; adverse fetal outcomes of neonatal thrombocytopenia, at times associated with anemia, reported. Obtain a CBC in neonates exposed to natalizumab in utero.
Lactation
Distributed into human milk; effects of the drug on nursing infants or on milk production not known.
Consider benefits of breastfeeding along with the woman's clinical need for natalizumab and any potential adverse effects on the breastfed infant from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy not established in patients <18 years of age with MS or Crohn disease.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.
Hepatic Impairment
Clinically important liver dysfunction reported in patients receiving natalizumab.
Renal Impairment
Not studied in patients with renal impairment.
Common Adverse Effects
Adverse effects occurring in ≥10% of patients with MS include headache, fatigue, arthralgia, depression, urinary tract infection, lower respiratory tract infection, gastroenteritis, vaginitis, depression, extremity pain, abdominal discomfort, diarrhea, rash.
Adverse effects occurring in ≥10% of patients with Crohn disease receiving the drug include headache, fatigue, upper respiratory tract infections, nausea.
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Corticosteroids |
Increased incidence of infection |
|
|
Immunosuppressive agents (e.g., azathioprine, cyclosporine, mercaptopurine, methotrexate) and TNF inhibitors |
Potential for increased risk of PML and other infections |
Do not use concomitantly in patients with Crohn disease Generally avoid natalizumab in MS patients receiving chronic immunosuppressive or immunomodulatory therapy |
|
Interferon beta |
Potential increased natalizumab serum concentrations and half-life; no apparent effect on interferon beta-1a pharmacokinetics |
Pharmacokinetic interaction may not be clinically important Safety of concomitant interferon beta not established |
|
Vaccines |
Data not available on effects of vaccination, including secondary transmission of infection from live viral vaccines, in patients receiving natalizumab |
Natalizumab Pharmacokinetics
Elimination
Half-life
Mean half-life is approximately 11 days.
Special Populations
Clearance increases with body weight in less than proportional manner.
Presence of persistent anti-natalizumab antibodies appears to increase drug clearance approximately 3-fold.
Stability
Storage
Parenteral
Concentrate for IV Infusion
Store vials at 2–8°C; protect from light. Do not shake or freeze.
Following dilution, infuse immediately or refrigerate at 2–8°C and use within 48 hours for Tysabri and 4 hours for Tyruko. Do not freeze diluted solution.
Actions
-
Mechanism of action in MS not fully elucidated; may involve blockade of α4β1 integrin-mediated leukocyte migration from peripheral blood into CNS.
-
Binds specifically to α4-subunits of α4β1 and α4β7 integrins expressed on the surface of all leukocytes (except neutrophils) and inhibits α4-mediated adhesion of leukocytes to their counterreceptors, including vascular cell adhesion molecule-1 (VCAM-1).
-
May also block α4-mediated cell binding to ligands such as osteopontin and CS-1 of fibronectin.
-
In Crohn disease, interaction of α4β7 integrin with the endothelial receptor mucosal addressin cell adhesion molecule-1 (MAdCAM-1) implicated as an important contributor to the chronic inflammation of the disease. MAdCAM-1 expression found to be increased at active sites of inflammation suggesting that it may play a role in the recruitment of leukocytes to mucosa and contribute to the inflammatory response characteristic of the disease.
-
Mechanism of action in Crohn disease not fully elucidated; may involve blockade of the interaction of α4β7 integrin receptor with MAdCAM-1 expressed on the vascular endothelium at inflammatory foci.
Advice to Patients
-
Advise patients to read the FDA-approved patient labeling (medication guide) prior to initiating natalizumab therapy and before each dose of the drug.
-
Inform patients that PML has occurred in patients treated with natalizumab and that PML usually leads to death or severe disability over weeks or months.
-
Stress importance of promptly informing clinicians of any new or worsening symptoms suggestive of PML (e.g., progressive weakness on one side of the body; clumsiness of limbs; disturbance of vision; changes in thinking, memory, personality, orientation leading to confusion) that have progressed over days to weeks.
-
Advise patients that natalizumab is only available through restricted distribution programs under a REMS.
-
Advise patients to immediately report any symptoms consistent with a hypersensitivity reaction (e.g., urticaria, pruritus, difficulty breathing) during or following an infusion of natalizumab.
-
Inform patients that natalizumab may lower the ability of their immune system to fight infections and to report any symptoms of infection to their clinician.
-
Inform patients that natalizumab increases the risk of developing encephalitis and meningitis, which could be fatal, and acute retinal necrosis, which could lead to blindness, caused by the family of herpes viruses (e.g., herpes simplex and varicella zoster viruses). Instruct patients to immediately report any possible symptoms of encephalitis and meningitis (such as fever, headache, and confusion) or acute retinal necrosis (such as decreased visual acuity, eye redness, or eye pain).
-
Inform patients that natalizumab may result in a reduced platelet count, which can cause severe bleeding. Instruct patients to report any related symptoms (e.g., easy bruising, prolonged bleeding, petechiae, abnormally heavy menstrual periods, new bleeding from the nose or gums) to their clinician. Advise patients that natalizumab may cause low platelet or red blood cell counts in neonates exposed to the drug during pregnancy.
-
Inform patients of the risk of liver injury with natalizumab and to contact their clinician if symptoms of hepatotoxicity develop.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and any concomitant illnesses.
-
Advise patients to inform their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer's labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Natalizumab is available only through a restricted distribution program (TOUCH Prescribing Program for Tysabri and TYRUKO REMS for Tyruko).
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection concentrate, for IV infusion only |
300 mg/15 mL |
Tysabri |
Biogen |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection concentrate, for IV infusion only |
300 mg/15 mL |
Tyruko |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Biological Products Related to natalizumab
Find detailed information on biosimilars for this medication.
Frequently asked questions
- Does Tysabri suppress the immune system?
- What biosimilars have been approved in the United States?
- How long can you take Tysabri for?
- Is Tysabri a form of chemotherapy?
- Does Tysabri cause cancer?
- How to prevent hair loss from Tysabri (natalizumab)?
More about natalizumab
- Check interactions
- Compare alternatives
- Reviews (102)
- Side effects
- Dosage information
- During pregnancy
- Drug class: selective immunosuppressants
- Breastfeeding
- En español