Lutetium Lu 177 Dotatate (Monograph)
Brand name: Lutathera
Drug class: Antineoplastic Agents
Introduction
Peptide receptor radionuclide agent; a lutetium 177 radiolabeled tetraazacyclododecane-tetra-acetic acid (DOTA)-somatostatin analog conjugate consisting of the somatostatin analog octreotide linked to a chelator (DOTA).
Uses for Lutetium Lu 177 Dotatate
Neuroendocrine Tumors of Gastroenteropancreatic Origin
Treatment of somatostatin receptor-positive neuroendocrine tumors of gastroenteropancreatic origin (GEP-NET), including foregut, midgut, and hindgut neuroendocrine tumors (designated an orphan drug by FDA for treatment of this cancer).
Lutetium Lu 177 Dotatate Dosage and Administration
General
-
Consult specialized references for procedures for proper handling (i.e., use of waterproof gloves, shields, tongs) and disposal of radionuclides.
-
Use only by qualified clinicians (i.e., authorized by an appropriate regulatory agency) experienced in the safe use and handling of radionuclides.
-
To minimize risk of nephrotoxicity, administer an amino acid solution containing 18–24 g of l-lysine and 18–24 g of l-arginine (osmolarity <1050 mOsm/L) in 1.5–2.2 L by IV infusion 30 minutes prior to each lutetium Lu 177 dotatate infusion and continue during and for at least 3 hours following completion of the lutetium Lu 177 dotatate infusion. (See Renal Effects under Cautions.) To minimize risk of nausea associated with amino acid infusions, administer an antiemetic (e.g., granisetron, ondansetron) 30 minutes prior to each amino acid infusion.
-
Amino acid solution may be administered through the same IV line (equipped with a 3-way valve) or a separate IV line in the opposite arm.
-
Adequately hydrate patients (e.g., one glass of water every hour) during and after administration of lutetium Lu 177 dotatate to ensure good urinary output.
-
When used in combination with short-acting (immediate-release) or long-acting (extended-release) octreotide, withhold short- or long-acting octreotide for 24 hours or 4 weeks, respectively, prior to each dose of lutetium Lu 177 dotatate. (See Specific Drugs under Interactions.)
-
Single 30-mg dose of long-acting octreotide acetate may be administered by IM injection between 4–24 hours after administration of lutetium Lu 177 dotatate; do not administer within 4 weeks prior to administration of lutetium Lu 177 dotatate. May continue long-acting octreotide acetate (30 mg administered by IM injection every 4 weeks) until disease progression or for a treatment duration of up to 18 months following discontinuance of lutetium Lu 177 dotatate.
Administration
IV Administration
Observe standard precautions for minimizing risk of radiation exposure (i.e., use of waterproof gloves, shielding, tongs).
Administer by IV infusion. Do not administer by rapid IV injection (e.g., IV push or bolus). After lutetium Lu 177 dotatate administration, flush with 25 mL of 0.9% sodium chloride injection.
Do not inject directly into IV solutions.
Confirm level of radioactivity in vial containing lutetium Lu 177 dotatate with an appropriate calibrated radioactivity measurement system (e.g., Geiger counter ).
Insert short (2.5-cm length) 20-gauge needle, connected to a primed administration set and infusion bag containing 500 mL of 0.9% sodium chloride injection, into vial containing 370 MBq/mL (equivalent to 10 mCi/mL) of lutetium Lu 177 dotatate; placement of this needle must remain above the lutetium Lu 177 dotatate solution. Do not inject lutetium Lu 177 dotatate directly into the 0.9% sodium chloride solution.
Insert long (9-cm length) 18-gauge needle into the same vial containing 370 MBq/mL (equivalent to 10 mCi/mL) of lutetium Lu 177 dotatate; securely position needle at bottom of the vial for the duration of infusion. Connect long needle to a dedicated IV line, primed with 0.9% sodium chloride solution, for infusion of lutetium Lu 177 dotatate to patient.
Level of lutetium Lu 177 dotatate solution in vial should remain constant during entire infusion to ensure complete administration. Discontinue lutetium Lu 177 dotatate infusion once level of radioactivity stabilizes for ≥5 minutes.
Discard any partially used vial or administration sets according to local and federal regulations.
Rate of Administration
Flow of 0.9% sodium chloride injection into the vial containing lutetium Lu 177 dotatate increases vial pressure which facilitates flow of lutetium Lu 177 dotatate to patient.
Allow 0.9% sodium chloride injection to flow (regulated by clamp) into vial containing lutetium Lu 177 dotatate injection by gravity.
Alternatively, may use infusion pump to control rate of 0.9% sodium chloride solution. If an infusion pump is used, set 0.9% sodium chloride solution at initial rate of 50–100 mL/hour for 5–10 minutes, then increase to 200–300 mL/hour for 25–30 minutes (total infusion time of 30–40 minutes).
Dosage
Adults
GEP-NET
IV
7.4 GBq (equivalent to 200 mCi) every 8 weeks for a total of 4 doses.
Dosage Modification for Toxicity
IV
Some adverse effects require temporary interruption, dosage reduction, and/or permanent discontinuance of therapy.
Do not reduce dosage of amino acid solution if dosage of lutetium Lu 177 dotatate is reduced.
Hematologic Toxicity
IVIf grade 2–4 thrombocytopenia occurs, withhold therapy until toxicity improves to grade 1 or less, and then resume therapy at a reduced dosage of 3.7 GBq (equivalent to 100 mCi). If grade 2–4 thrombocytopenia does not recur on a reduced dosage, re-escalate dosage to 7.4 GBq (equivalent to 200 mCi). If grade 2–4 thrombocytopenia recurs or does not improve within 16 weeks of withholding therapy, permanently discontinue lutetium Lu 177 dotatate. (See Hematologic Effects under Cautions.)
If grade 3 or 4 neutropenia or anemia occurs, withhold therapy until toxicity improves to grade 2 or less, and then resume therapy at a reduced dosage of 3.7 GBq (equivalent to 100 mCi). If grade 3 or 4 neutropenia or anemia does not recur on a reduced dosage, re-escalate dosage to 7.4 GBq (equivalent to 200 mCi). If grade 3 or 4 neutropenia or anemia recurs or does not improve within 16 weeks of withholding therapy, permanently discontinue lutetium Lu 177 dotatate.
Nephrotoxicity
IVFor Scr elevations of ≥40% from baseline, Clcr <40 mL/minute, or decrease in Clcr of ≥40% from baseline, withhold therapy until toxicity completely resolves, and then resume therapy at a reduced dosage of 3.7 GBq (equivalent to 100 mCi). If the toxicity does not recur on a reduced dosage, re-escalate dosage to 7.4 GBq (equivalent to 200 mCi). If the toxicity recurs or does not improve within 16 weeks of withholding therapy, permanently discontinue lutetium Lu 177 dotatate. (See Renal Effects under Cautions.)
Hepatotoxicity
IVFor serum bilirubin elevations >3 times the ULN or for serum albumin <3 g/dL with PT ratio <70%, withhold therapy until toxicity completely resolves, and then resume therapy at a reduced dosage of 3.7 GBq (equivalent to 100 mCi). If the toxicity does not recur on a reduced dosage, re-escalate dosage to 7.4 GBq (equivalent to 200 mCi). If the toxicity recurs or does not improve within 16 weeks of withholding therapy, permanently discontinue lutetium Lu 177 dotatate. (See Hepatic Toxicity under Cautions.)
Other Toxicity
IVIf grade 3 or 4 nonhematologic toxicity occurs, withhold therapy until toxicity improves to grade 2 or less, and then resume therapy at a reduced dosage of 3.7 GBq (equivalent to 100 mCi). If the toxicity does not recur on a reduced dosage, re-escalate dosage to 7.4 GBq (equivalent to 200 mCi). If the toxicity recurs or does not improve within 16 weeks of withholding therapy, permanently discontinue lutetium Lu 177 dotatate.
Prescribing Limits
Adults
Neuroendocrine Tumors of Gastroenteropancreatic Origin
IV
Maximum of 4 doses (maximum cumulative dose of 29.6 GBq [equivalent to 800 mCi]).
Special Populations
Hepatic Impairment
Mild or moderate hepatic impairment: No initial dosage adjustment required.
Severe hepatic impairment (total bilirubin concentration >3 times the ULN with any AST concentration): Not studied.
Renal Impairment
Mild or moderate renal impairment (Clcr ≥30 mL/minute): No initial dosage adjustment required.
Severe renal impairment (Clcr <30 mL/minute) or end-stage renal disease: Not studied.
Geriatric Patients
No specific dosage recommendations.
Cautions for Lutetium Lu 177 Dotatate
Contraindications
-
Manufacturer states none known.
Warnings/Precautions
Radiation Exposure
Radioactive component of lutetium Lu 177 dotatate (lutetium 177) contributes to patient's lifetime cumulative radiation exposure. Development of new malignancies is a known risk of long-term radiation exposure. (See Myelodysplastic Syndrome [MDS] and Acute Leukemia under Cautions.)
Radioactivity can be detected in urine for up to 30 days following administration of lutetium Lu 177 dotatate. Employ institutional good radiation safety practices and patient management procedures during and after administration of lutetium Lu 177 dotatate to minimize exposure of patients, medical personnel, and household contacts to radiation.
Hematologic Effects
Anemia, thrombocytopenia, and neutropenia occur frequently in patients receiving lutetium Lu 177 dotatate in combination with long-acting octreotide. Median time to nadir platelet count is 5.1 weeks. Thrombocytopenia resolves in most patients in a median of 2 months.
Risk factors for developing grade 3 or 4 hematologic toxicity include preexisting renal impairment, WBC count <4000/mm3, advanced age (i.e., >70 years of age), extensive tumor mass, and high tumor uptake on octreotide scintigraphy (i.e., OctreoScan).
Monitor CBC counts prior to and periodically during therapy. If hematologic toxicity occurs, temporary interruption followed by dosage reduction or discontinuance of therapy may be necessary. (See Dosage Modification for Toxicity under Dosage and Administration.)
Myelodysplastic Syndrome (MDS) and Acute Leukemia
MDS and acute leukemia reported rarely in patients receiving lutetium Lu 177 dotatate in combination with long-acting octreotide. Median duration of lutetium Lu 177 dotatate therapy in patients who developed MDS or acute leukemia was 28 (range: 9–41 months) or 55 months (range: 32–155 months), respectively.
Renal Effects
Renal failure, sometimes requiring dialysis, reported in patients receiving lutetium Lu 177 dotatate; however, some patients had preexisting renal impairment or risk factors for renal failure (e.g., diabetes mellitus, hypertension). Lutetium Lu 177 dotatate is extensively reabsorbed in renal proximal tubules; accumulation of lutetium 177 in renal interstitium can result in acute or chronic renal damage.
Advanced age (i.e., >60 years of age), poorly controlled diabetes mellitus, hypertension, prior platinum-containing therapy, and preexisting renal impairment may be risk factors for developing nephrotoxicity associated with peptide receptor radionuclide therapy (PRRT).
Coadministration of positively charged amino acids (e.g., l-lysine, l-arginine) with PRRT minimizes the risk of nephrotoxicity. Administer an amino acid solution containing l-lysine and l-arginine 30 minutes prior to each lutetium Lu 177 dotatate infusion and continue during and for at least 3 hours after the lutetium Lu 177 dotatate infusion. (See General under Dosage and Administration.)
Monitor renal function (i.e., Scr) prior to and periodically during therapy, and more frequently in patients with mild or moderate renal impairment. If nephrotoxicity occurs, temporary interruption followed by dosage reduction or discontinuance of therapy may be necessary. (See Dosage Modification for Toxicity under Dosage and Administration.)
Hepatic Toxicity
Hepatic tumor hemorrhage, edema, necrosis, intrahepatic congestion, and cholestasis reported in patients receiving lutetium Lu 177 dotatate. Hepatic metastases may increase risk of developing hepatotoxicity.
Monitor liver function tests (i.e., serum ALT/AST, bilirubin, albumin) prior to and periodically during treatment. If hepatotoxicity occurs, temporary interruption followed by dosage reduction or discontinuance of therapy may be necessary. (See Dosage Modification for Toxicity under Dosage and Administration.)
Carcinoid Hormonal Crisis
Carcinoid hormonal crisis (also known as neuroendocrine hormonal crisis) reported rarely, generally during or within 24 hours of the initial dose of lutetium Lu 177 dotatate. May manifest as flushing, diarrhea, bronchospasm, or hypotension. Hypercalcemia also reported.
Monitor patients for manifestations of carcinoid hormonal crisis and manage (e.g., IV somatostatin analog, hydration, corticosteroids, electrolytes) as clinically indicated if such crises occur.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. No available data on use in pregnant women.
Verify pregnancy status prior to initiating therapy. Avoid pregnancy during therapy. Women of reproductive potential should use an effective method of contraception while receiving lutetium Lu 177 dotatate and for 7 months after the final dose. Men who are partners of such women should use effective contraception during therapy and for 4 months after the final dose. If used during pregnancy or if patient becomes pregnant while receiving the drug, apprise patients of potential fetal hazard.
Impairment of Fertility
May impair male and female fertility.
Specific Populations
Pregnancy
May cause fetal harm. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Not known whether distributed into human milk. Effects on nursing infant and milk production also unknown. Discontinue nursing during therapy and for 2.5 months after the last dose.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
No differences in serious adverse effects and response rate relative to younger adults; however, some data suggest advanced age may increase risk for developing nephrotoxicity or grade 3 or 4 hematologic toxicity. (See Hematologic Effects and also see Renal Effects under Cautions.)
Hepatic Impairment
Data lacking in patients with hepatic impairment.
Safety not established in patients with severe hepatic impairment (total bilirubin concentration >3 times the ULN with any AST concentration).
Renal Impairment
Mild or moderate renal impairment may increase risk for adverse reactions. Monitor renal function frequently.
Safety not established in patients with severe renal impairment (Clcr <30 mL/minute) or end-stage renal disease.
Common Adverse Effects
Nausea, vomiting, fatigue, musculoskeletal pain, abdominal pain, diarrhea, decreased appetite, dizziness, headache, peripheral edema, flushing, alopecia, distension, anxiety, hypertension, renal failure, cough, constipation, lymphopenia, elevated concentrations of Scr, hyperglycemia, anemia, elevated concentrations of γ-glutamyltransferase (γ-glutamyltranspeptidase, GGT, GGTP), elevated concentrations of alkaline phosphatase, leukopenia, thrombocytopenia, elevated AST or ALT concentrations, hyperuricemia, hypocalcemia, elevated concentrations of bilirubin, hypokalemia, neutropenia, hyperkalemia, hypernatremia, hypoglycemia.
At a median follow-up >4 years in a retrospective analysis, serious adverse reactions included MDS, acute leukemia, renal failure, hypotension, cardiac failure, MI, and carcinoid crisis. Most patients received a cumulative lutetium Lu 177 dotatate dose of ≥22.2 GBq.
Drug Interactions
In vitro, nonradioactive lutetium dotatate (lutetium Lu 175 dotatate) does not inhibit or induce CYP isoenzymes 1A2, 2B6, 2C9, 2C19, or 2D6.
In vitro, nonradioactive lutetium dotatate does not inhibit P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), organic anion transporter (OAT) 1, OAT3, organic anion transport protein (OATP) 1B1, OATP1B3, organic cation transporter (OCT) 1, or OCT2.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Corticosteroids |
May induce down-regulation of somatostatin receptor type 2 (SSRT2) |
No specific information in US prescribing information Manufacturer in European Union (EU) recommends avoiding concomitant use with long-term, high-dose corticosteroids; evaluate patients receiving corticosteroids for chronic conditions for sufficient somatostatin receptor expression Manufacturer in EU also recommends avoiding concomitant intermittent corticosteroid use; if such use cannot be avoided, may administer a single corticosteroid dose ≥1 hour after completion of the lutetium Lu 177 dotatate infusion |
|
Octreotide |
May competitively inhibit binding of lutetium Lu 177 dotatate to somatostatin receptors resulting in reduced lutetium Lu 177 dotatate efficacy |
Withhold long-acting octreotide for ≥4 weeks prior to administering lutetium Lu 177 dotatate; may administer single 30-mg IM dose of long-acting octreotide acetate between 4–24 hours after each dose of lutetium Lu 177 dotatate May continue long-acting octreotide acetate (30 mg IM every 4 weeks) until disease progression or for up to 18 months following discontinuance of lutetium Lu 177 dotatate Withhold short-acting octreotide for ≥24 hours prior to each dose of lutetium Lu 177 dotatate |
Lutetium Lu 177 Dotatate Pharmacokinetics
Distribution
Extent
Following IV administration, rapidly distributes into kidneys, tumor lesions, liver, spleen, pituitary gland, and thyroid within 4 hours.
Not known whether lutetium Lu 177 dotatate is distributed into milk.
Plasma Protein Binding
Nonradioactive lutetium dotatate (lutetium Lu 175 dotatate): 43%.
Elimination
Elimination Route
Eliminated primarily in urine. Following IV administration, 44, 58, or 65% of the dose is excreted in urine within 5, 24, or 48 hours, respectively.
Following IV administration, >99% of dose expected to be eliminated within 14 days.
Coadministration of l-lysine and l-arginine increases mean β-phase plasma clearance by 36%.
Half-life
Mean effective half-life in blood is 3.5 hours.
Mean terminal half-life is 71 hours.
Stability
Storage
Parenteral
Injection
<25°C. Store in manufacturer's lead shielded container in provided plastic sealed container; shelf-life of the injection is 72 hours.
Compatibility
Parenteral
Solution Compatibility1
|
Compatible |
|---|
|
Sodium chloride 0.9% |
Y-Site Compatibility1
|
Compatible |
|---|
|
l-Lysine |
|
l-Arginine |
Actions
-
Peptide receptor radionuclide agent; a lutetium 177 radiolabeled tetraazacyclododecane-tetra-acetic acid (DOTA)-somatostatin analog conjugate consisting of the somatostatin analog octreotide linked to a chelator (DOTA).
-
Somatostatin analog component of lutetium Lu 177 dotatate binds to somatostatin receptors (specifically SSRT2), the resultant complex is internalized by tumor cells, and lutetium 177 induces cellular damage by forming free radicals in the target and neighboring cells.
Advice to Patients
-
Importance of advising patients to follow standard precautions for minimizing radiation exposure to household contacts.
-
Risk of myelosuppression (e.g., thrombocytopenia, neutropenia, anemia). Importance of monitoring CBC counts prior to and periodically during therapy. Importance of informing clinician promptly if any signs or symptoms of myelosuppression or infection (e.g., fever, chills, dizziness, shortness of breath, bleeding, easy bruising) occur.
-
Risk of MDS and acute leukemia.
-
Risk of renal toxicity. Importance of monitoring renal function prior to and periodically during therapy. Importance of advising patients to maintain adequate hydration during and after administration of lutetium Lu 177 dotatate to ensure good urinary output.
-
Risk of hepatotoxicity. Importance of liver function test monitoring prior to and periodically during treatment.
-
Risk of carcinoid hormonal crisis. Importance of informing clinician if manifestations of carcinoid hormonal crisis (e.g., severe flushing, diarrhea, bronchospasm, hypotension) occur.
-
Risk of fetal harm. Necessity of advising women of reproductive potential that they should use effective methods of contraception while receiving lutetium Lu 177 dotatate and for 7 months after the final dose. Necessity of advising male patients with female partners of reproductive potential that they should use effective methods of contraception while receiving the drug and for 4 months after the final dose. Importance of women informing clinicians if they are or plan to become pregnant. Apprise patient of potential fetal hazard if used during pregnancy.
-
Importance of advising women to avoid breast-feeding while receiving lutetium Lu 177 dotatate and for 2.5 months after the last dose.
-
Risk of impaired male and female fertility.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant diseases.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care. For further information on the handling of antineoplastic agents, see the ASHP Guidelines on Handling Hazardous Drugs at [Web].
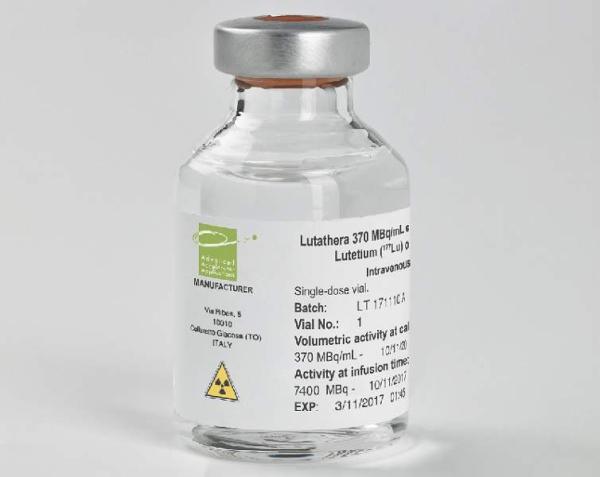
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for IV infusion only |
370 MBq/mL (equivalent to 10 mCi/mL) |
Lutathera (available in a lead-shielded container) |
Advanced Accelerator Applications |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about lutetium lu 177 dotatate
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: therapeutic radiopharmaceuticals
- Breastfeeding
- En español