Idecabtagene (Monograph)
Brand name: Abecma
Drug class: Gene Therapy
Warning
Warning: Cytokine Release Syndrome, Neurologic Toxicities, HLH/MAS, Prolonged Cytopenia, and Secondary Hematological Malignancies.1
See full prescribing information for complete boxed warning.1
-
Cytokine Release Syndrome (CRS), including fatal or life-threatening reactions, occurred in patients following treatment with idecabtagene vicleucel.1 Do not administer idecabtagene vicleucel to patients with active infection or inflammatory disorders.1 Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids.1
-
Neurologic toxicities, which may be severe or life-threatening, occurred following treatment with idecabtagene vicleucel, including concurrently with CRS, after CRS resolution, or in the absence of CRS.1 Monitor for neurologic events after treatment with idecabtagene vicleucel.1 Provide supportive care and/or corticosteroids as needed.1
-
Hemophagocytic lymphohistiocytosis/macrophage activation syndrome (HLH/MAS), including fatal and life-threatening reactions, occurred in patients following treatment with idecabtagene vicleucel.1 HLH/MAS can occur with CRS or neurologic toxicities.1
-
Prolonged cytopenia with bleeding and infection, including fatal outcomes following stem cell transplantation for hematopoietic recovery, occurred following treatment with idecabtagene vicleucel.1
-
T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19-directed genetically modified autologous T cell immunotherapies, including idecabtagene vicleucel.1
Introduction
Idecabtagene vicleucel is a B-cell maturation antigen (BCMA)-directed genetically modified autologous T cell immunotherapy.1
Uses for Idecabtagene
Idecabtagene vicleucel has the following uses:
Idecabtagene vicleucel is a chimeric antigen receptor (CAR) T-cell therapy indicated for the treatment of adult patients with relapsed or refractory multiple myeloma after 2 or more prior lines of therapy, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 monoclonal antibody.1 Idecabtagene vicleucel has been designated an orphan drug by FDA for this use.2
Idecabtagene vicleucel is an individualized cellular product prepared from autologous T cells obtained by leukopheresis.3 The patient's T-cells are sent to a commercial laboratory where they are genetically modified to express chimeric antigen receptors (CAR), and then infused back into the patient.3
Efficacy and safety of idecabtagene vicleucel in the treatment of patients with relapsed or refractory multiple myeloma after 2 to 4 prior lines of therapy were evaluated in an open-label, multicenter, randomized, controlled study (KarMMa-3 study).1 6 A total of 386 patients were randomized to receive idecabtagene vicleucel or 1 of 5 standard regimens (daratumumab, pomalidomide, dexamethasone [DPd], daratumumab, bortezomib, dexamethasone [DVd], ixazomib, lenalidomide, dexamethasone [IRd], carfilzomib, dexamethasone [Kd], or elotuzumab, pomalidomide, dexamethasone [EPd]).1 6 Patients in the idecabtagene vicleucel group received lymphodepleting chemotherapy (cyclophosphamide and fludarabine) starting 5 days prior to the infusion of idecabtagene vicleucel.1 The primary efficacy measure was progression-free survival (PFS).1 At a median follow-up of 18.6 months, median PFS was 13.3 months in patients receiving idecabtagene vicleucel compared with 4.4 months in patients receiving standard regimens.6 Overall response was achieved in 71% of patients in the idecabtagene vicleucel group and 42% of patients in the standard regimen group.1 6 The median duration of response was 14.8 months in the idecabtagene vicleucel group and 9.7 months in the standard regimen group.1 A higher proportion of patients in the idecabtagene vicleucel treatment arm compared to the standard treatment arm died within the first 9 months of randomization.1
Efficacy and safety of idecabtagene vicleucel in the treatment of patients with relapsed or refractory multiple myeloma after 3 or more prior lines of therapy were evaluated in a single arm, open-label, multicenter study (KarMMa study).1 3 4 5 Patients received lymphodepleting chemotherapy (cyclophosphamide and fludarabine), followed by a single IV infusion of idecabtagene vicleucel,1 In the efficacy population of 100 patients, the overall response rate was 72% and the stringent complete response (CR) rate was 28%.1 Of the 72 subjects who achieved an objective response, the median duration of response was 11 months.1 4 At a median follow up of 10.7 months, the median duration of response for stringent CR was 19 months.4
CAR T-cell therapies can be associated with severe toxicities; the American Society of Clinical Oncology (ASCO) and other experts have published guidelines on the management of these therapies and their associated toxicities.10 11 12 13
Idecabtagene Dosage and Administration
General
Idecabtagene vicleucel is available in the following dosage form(s) and strength(s):
-
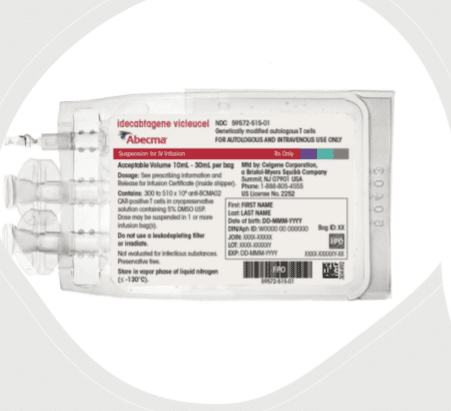
Idecabtagene vicleucel is a cell suspension for IV infusion.1
-
A single dose of idecabtagene vicleucel contains a cell suspension of 300 to 460 × 106 CAR-positive T cells in one or more infusion bags.1
Dosage
It is essential that the manufacturer's labeling be consulted for more detailed information on dosage and administration of this drug. Dosage summary:
Adults
Dosage and Administration
For autologous use only. For IV use only.1
-
Do NOT use a leukodepleting filter.1
-
Administer a lymphodepleting chemotherapy regimen of cyclophosphamide and fludarabine before infusion of idecabtagene vicleucel.1 Confirm the availability of idecabtagene vicleucel prior to starting the lymphodepleting chemotherapy regimen.1 Administer idecabtagene vicleucel 2 days after completion of lymphodepleting chemotherapy.1
-
Confirm the patient's identity prior to infusion.1 Check that the patient's identity matches patient identifiers on the idecabtagene vicleucel cassette(s) and infusion bag(s).1 Do not infuse idecabtagene vicleucel if the information on the patient-specific label(s) does not match the intended patient.1
-
Premedicate with acetaminophen and an H1-antihistamine approximately 30 to 60 minutes before infusion.1
-
Avoid prophylactic use of dexamethasone or other systemic corticosteroids as such use may interfere with the activity of idecabtagene vicleucel.1
-
Confirm availability of tocilizumab prior to infusion.1
-
Dosing of idecabtagene vicleucel is based on the number of chimeric antigen receptor (CAR)-positive T cells.1 The recommended dose range is 300 to 510 × 106 CAR-positive T cells.1
-
See Full Prescribing Information for detailed instructions on preparation and administration.1
Cautions for Idecabtagene
Contraindications
None.1
Warnings/Precautions
Early Death
In KarMMa-3, a randomized (2:1) controlled trial, a higher proportion of patients experienced death within 9 months after randomization in the idecabtagene vicleucel arm (45/254; 18%) compared to the standard regimens arm (15/132; 11%).1 Early deaths occurred in 8% (20/254) and 0% prior to idecabtagene vicleucel infusion and standard regimen administration, respectively, and 10% (25/254) and 11% (15/132) after idecabtagene vicleucel infusion and standard regimen administration, respectively.1 Out of the 20 deaths that occurred prior to infusion, 15 occurred from disease progression, 3 occurred from adverse events and 2 occurred from unknown causes.1 Out of the 25 deaths that occurred after idecabtagene vicleucel infusion, 10 occurred from disease progression, 11 occurred from adverse events, and 4 occurred from unknown causes.1
Cytokine Release Syndrome
Cytokine Release Syndrome (CRS), including fatal or life-threatening reactions, occurred following treatment with idecabtagene vicleucel.1 CRS occurred in 85% (108/127) of patients receiving idecabtagene vicleucel.1 Grade 3 or higher CRS (Lee grading system) occurred in 9% (12/127) of patients, with Grade 5 CRS reported in one (0.8%) patient.1 The median time-to-onset of CRS, any grade, was 1 day (range: 1 to 23 days), and the median duration of CRS was 7 days (range: 1 to 63 days) in all patients, including the patient who died.1 The most common manifestations of CRS (≥10%) included pyrexia (87%), hypotension (30%), tachycardia (26%), chills (19%), and hypoxia (16%).1 Grade 3 or higher events that may be associated with CRS include hypotension, hypoxia, hyperbilirubinemia, hypofibrinogenemia, ARDS, atrial fibrillation, hepatocellular injury, metabolic acidosis, pulmonary edema, coagulopathy, renal failure, multiple organ dysfunction syndrome and hemophagocytic lymphohistiocytosis/macrophage activation syndrome (HLH/MAS).1
Identify CRS based on clinical presentation.1 Evaluate for and treat other causes of fever, hypoxia, and hypotension.1 CRS has been reported to be associated with findings of HLH/MAS, and the physiology of the syndromes may overlap.1 HLH/MAS is a potentially life-threatening condition.1 In patients with progressive symptoms of CRS or refractory CRS despite treatment, evaluate for evidence of HLH/MAS.1
Of the 349 patients who received idecabtagene vicleucel in clinical trials, 226 (65%) patients received tocilizumab; 39% (135/349) received a single dose, while 26% (91/349) received more than 1 dose of tocilizumab.1 Overall, 24% (82/349) of patients received at least 1 dose of corticosteroids for treatment of CRS.1 Almost all patients who received corticosteroids for CRS also received tocilizumab.1 For patients treated in dose range of 460 to 510 x 106 CAR-positive T cells, 76% (54/71) of patients received tocilizumab and 35% (25/71)received at least 1 dose of corticosteroids for treatment of CRS.1 For patients treated in dose range of 300 to 460 x 106 CAR-positive T cells, 63% (152/241) of patients received tocilizumab and 20% (49/241) received at least 1 dose of corticosteroid for treatment of CRS.1
Ensure that a minimum of 2 doses of tocilizumab are available prior to infusion of idecabtagene vicleucel.1
Monitor patients at least daily for 7 days following idecabtagene vicleucel infusion at the healthcare facility for signs and symptoms of CRS.1 Monitor patients for signs or symptoms of CRS for at least 4 weeks after infusion.1 At the first sign of CRS, institute treatment with supportive care, tocilizumab and/or corticosteroids as indicated.1
Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time.1
Neurologic Toxicities
Neurologic toxicities, including immune-effector cell-associated neurotoxicity (ICANS), which may be severe or life-threatening, occurred concurrently with CRS, after CRS resolution, or in the absence of CRS following treatment with idecabtagene vicleucel.1
In patients receiving idecabtagene vicleucel in the KarMMa and KarMMa-3 studies, CAR T cell-associated neurotoxicity occurred in 40% (139/349), including Grade 3 in 4% (14/349) and Grade 4 in 0.6% (2/349) of patients.1 The median time to onset of neurotoxicity was 2 days (range: 1 to 148 days).1 The median duration of CAR T cell-associated neurotoxicity was 8 days (range: 1 to 720 days) in all patients including those with ongoing neurologic events at the time of death or data cut off.1 CAR T cell-associated neurotoxicity resolved in 123 of 139 (88%) patients and median time to resolution was 5 days (range: 1 to 245 days).1 One-hundred and thirty four out of 349 (38%) patients with neurotoxicity had CRS.1 The onset of neurotoxicity during CRS was observed in 93 patients, before the onset of CRS in 12 patients, and after the CRS event in 29 patients.1 The rate of Grade 3 or 4 CAR T cell-associated neurotoxicity was 5.6% (4/71) and 3.7% (9/241) for patients treated in dose range of 460 to 510 x 106 CAR-positive T cells and 300 to 460 x 106 CAR-positive T cells, respectively.1 The most frequent (≥5%) manifestations of CAR T cell-associated neurotoxicity include encephalopathy (21%), headache (15%), dizziness (8%), delirium (6%), and tremor (6%).1
At the safety update for the KarMMa-3 study, one patient developed fatal neurotoxicity 43 days after idecabtagene vicleucel.1 In KarMMa, one patient had ongoing Grade 2 neurotoxicity at the time of death.1 Two patients had ongoing Grade 1 tremor at the time of data cutoff.1
Cerebral edema has been associated with idecabtagene vicleucel in a patient in another study in multiple myeloma.1 Grade 3 myelitis and Grade 3 parkinsonism have occurred after treatment with idecabtagene vicleucel in another study in multiple myeloma.1
Monitor patients at least daily for 7 days following idecabtagene vicleucel infusion at the healthcare facility for signs and symptoms of neurologic toxicities.1 Rule out other causes of neurologic symptoms.1 Monitor patients for signs or symptoms of neurologic toxicities for at least 4 weeks after infusion and treat promptly.1 Neurologic toxicity should be managed with supportive care and/or corticosteroids as needed.1
Counsel patients to seek immediate medical attention should signs or symptoms of neurologic toxicity occur at any time.1
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage Activation Syndrome (MAS)
In patients receiving idecabtagene vicleucel in the KarMMa and KarMMa-3 studies, HLH/MAS occurred in 2.9% (10/349) of patients.1 All events of HLH/MAS had onset within 10 days of receiving idecabtagene vicleucel, with a median onset of 6.5 days (range: 4 to 10 days) and occurred in the setting of ongoing or worsening CRS.1 Five patients with HLH/MAS had overlapping neurotoxicity.1 The manifestations of HLH/MAS include hypotension, hypoxia, multiple organ dysfunction, renal dysfunction, and cytopenia.1
In KarMMa-3, one patient had Grade 5, two patients had Grade 4 and two patients had Grade 3 HLH/MAS.1 The patient with Grade 5 HLH/MAS also had Grade 5 candida sepsis and Grade 5 CRS.1 In another patient who died due to stroke, the Grade 4 HLH/MAS resolved prior to death.1 Two cases of Grade 3 and one case of Grade 4 HLH/MAS resolved.1
In KarMMa, one patient treated in the 300 x 106 CAR-positive T cells dose cohort developed fatal multi-organ HLH/MAS with CRS.1 In another patient with fatal bronchopulmonary aspergillosis, HLH/MAS was contributory to the fatal outcome.1 Three cases of Grade 2 HLH/MAS resolved.1
HLH/MAS is a potentially life-threatening condition with a high mortality rate if not recognized early and treated.1 Treatment of HLH/MAS should be administered per institutional standards.1
Hypersensitivity Reactions
Allergic reactions may occur with the infusion of idecabtagene vicleucel.1 Serious hypersensitivity reactions, including anaphylaxis, may be due to dimethyl sulfoxide (DMSO) in idecabtagene vicleucel.1
Infections
Idecabtagene vicleucel should not be administered to patients with active infections or inflammatory disorders.1 In all patients receiving idecabtagene vicleucel in KarMMa and KarMMa-3, infections (all grades) occurred in 61% of patients.1 Grade 3 or 4 infections occurred in 21% of patients.1 Grade 3 or 4 infections with an unspecified pathogen occurred in 12%, viral infections in 7%, bacterial infections in 4.3%, and fungal infections in 1.4% of patients.1 Overall, 15 patients had Grade 5 infections (4.3%); 8 patients (2.3%) with infections of pathogen unspecified, 3 patients (0.9%) with fungal infections, 3 patients (0.9%) with viral infections, and 1 patient (0.3%) with bacterial infection.1 Monitor patients for signs and symptoms of infection before and after idecabtagene vicleucel infusion and treat appropriately.1 Administer prophylactic, pre-emptive, and/or therapeutic antimicrobials according to standard institutional guidelines.1
Febrile neutropenia was observed in 38% (133/349) of patients after idecabtagene vicleucel infusion and may be concurrent with CRS.1 In the event of febrile neutropenia, evaluate for infection and manage with broad-spectrum antibiotics, fluids, and other supportive care as medically indicated.1
Viral Reactivation
Cytomegalovirus (CMV) infection resulting in pneumonia and death has occurred following idecabtagene vicleucel administration.1 Monitor and treat for CMV reactivation in accordance with clinical guidelines.1
Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, can occur in patients treated with drugs directed against plasma cells.1
Perform screening for CMV, HBV, hepatitis C virus (HCV), and human immunodeficiency virus (HIV) in accordance with clinical guidelines before collection of cells for manufacturing.1
Consider antiviral therapy to prevent viral reactivation per local institutional guidelines/clinical practice.1
Prolonged Cytopenias
Patients may exhibit prolonged cytopenias following lymphodepleting chemotherapy and idecabtagene vicleucel infusion.1
In patients receiving idecabtagene vicleucel in the KarMMa and KarMMa-3 studies, 40% of patients (139/349) experienced prolonged Grade 3 or 4 neutropenia and 42% (145/349) experienced prolonged Grade 3 or 4 thrombocytopenia that had not resolved by Month 1 following infusion.1 In 89% (123/139) of patients who recovered from Grade 3 or 4 neutropenia after Month 1, the median time to recovery from idecabtagene vicleucel infusion was 1.9 months.1 In 76% (110/145) of patients who recovered from Grade 3 or 4 thrombocytopenia, the median time to recovery was 1.9 months.1 Five patients underwent stem cell therapy for hematopoietic reconstitution due to prolonged cytopenia.1 The rate of Grade 3 or 4 thrombocytopenia was 62% (44/71) and 56% (135/241) for patients treated in dose range of 460 to 510 x 106 CAR-positive T cells and 300 to 460 x 106 CAR-positive T cells, respectively.1
Monitor blood counts prior to and after idecabtagene vicleucel infusion.1 Manage cytopenia with myeloid growth factor and blood product transfusion support according to local institutional guidelines.1
Hypogammaglobulinemia
Plasma cell aplasia and hypogammaglobulinemia can occur in patients receiving treatment with idecabtagene vicleucel.1 In all patients receiving idecabtagene vicleucel in the KarMMa and KarMMa-3 studies, hypogammaglobulinemia was reported as an adverse event in 13% (46/349) of patients; laboratory IgG levels fell below 500 mg/dL after infusion in 37% (130/349) of patients treated with idecabtagene vicleucel.
Hypogammaglobulinemia either as an adverse reaction or laboratory IgG level below 500 mg/dL after infusion occurred in 45% (158/349) of patients treated with idecabtagene vicleucel.1 Forty-one percent of patients received IV immunoglobulin (IVIG) post-idecabtagene vicleucel for serum IgG <400 mg/dL.1
Monitor immunoglobulin levels after treatment with idecabtagene vicleucel and administer IVIG for IgG <400 mg/dL.1 Manage per local institutional guidelines, including infection precautions and antibiotic or antiviral prophylaxis.1
Use of Live Vaccines
The safety of immunization with live viral vaccines during or following idecabtagene vicleucel treatment has not been studied.1 Vaccination with live virus vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during idecabtagene vicleucel treatment, and until immune recovery following treatment with idecabtagene vicleucel.1
Secondary Malignancies
Patients treated with idecabtagene vicleucel may develop secondary malignancies.1 In KarMMa-3, myeloid neoplasms (4 cases of myelodysplastic syndrome and 1 case of acute myeloid leukemia) occurred in 2.2% (5/222) of patients following treatment with idecabtagene vicleucel compared to none in the standard regimens arm at the time of the safety update.1 The median time to onset of myeloid neoplasm from idecabtagene vicleucel infusion was 338 days (range: 277 to 794 days).1 Three of these 5 patients died following the development of myeloid neoplasm.1 One out of the 5 cases of myeloid neoplasm occurred after initiation of subsequent antimyeloma therapy.1
T cell malignancies have occurred following treatment of hematologic malignancies with BCMA- and CD19‑directed genetically modified autologous T cell immunotherapies, including idecabtagene vicleucel.1 Mature T cell malignancies, including CAR-positive tumors, may present as soon as weeks following infusion, and may include fatal outcomes.1
Monitor life-long for secondary malignancies.1 In the event that a secondary malignancy occurs, contact Bristol-Myers Squibb at 1‑888‑805‑4555 for reporting and to obtain instructions on collection of patient samples for testing of secondary malignancy.1
Effects on Ability to Drive and Use Machines
Due to the potential for neurologic events, including altered mental status or seizures, patients receiving idecabtagene vicleucel are at risk for altered or decreased consciousness or coordination in the 8 weeks following treatment.1 Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, during this initial period.1
Specific Populations
Pregnancy
There are no available data with idecabtagene vicleucel use in pregnant women.1 No animal reproductive and developmental toxicity studies have been conducted with idecabtagene vicleucel to assess whether it can cause fetal harm when administered to a pregnant woman.1
It is not known if idecabtagene vicleucel has the potential to be transferred to the fetus.1 Based on the mechanism of action, if the transduced cells cross the placenta, they may cause fetal toxicity, including plasma cell aplasia or hypogammaglobulinemia.1 Therefore, idecabtagene vicleucel is not recommended for women who are pregnant, and pregnancy after idecabtagene vicleucel infusion should be discussed with the treating physician.1 Assess immunoglobulin levels in newborns of mothers treated with idecabtagene vicleucel.1
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown.1 The estimated background risk in the U.S. general population of major birth defects is 2% to 4% and of miscarriage is 15% to 20% of clinically recognized pregnancies.1
Lactation
There is no information regarding the presence of idecabtagene vicleucel in human milk, the effect on the breastfed infant, and the effects on milk production.1 The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for idecabtagene vicleucel and any potential adverse effects on the breastfed infant from idecabtagene vicleucel or from the underlying maternal condition.1
Females and Males of Reproductive Potential
Pregnancy status of sexually-active females with reproductive potential should be verified via pregnancy testing prior to starting treatment with idecabtagene vicleucel.1
See the prescribing information for fludarabine and cyclophosphamide for information on the need for effective contraception in patients who receive the lymphodepleting chemotherapy.1
There are insufficient exposure data to provide a recommendation concerning duration of contraception following treatment with idecabtagene vicleucel.1
There are no data on the effect of idecabtagene vicleucel on fertility.1
Pediatric Use
The safety and efficacy of idecabtagene vicleucel in patients under 18 years of age have not been established.1
Geriatric Use
In the clinical trial of idecabtagene vicleucel, 141 (40%) of the 349 patients in the KarMMa study were 65 years of age or older and 16/349 (4.6%) patients were 75 years of age or older.1 In the KarMMa study, all 5 cases of Grade 3 neurotoxicity occurred in patients ≥65 years of age (66 to 74 years).1 No clinically important differences in effectiveness of idecabtagene vicleucel were observed between these patients and patients younger than 65 years of age.1
Common Adverse Effects
The most common nonlaboratory adverse reactions (≥20%) include pyrexia, CRS, hypogammaglobulinemia, infections (pathogen unspecified), musculoskeletal pain, fatigue, febrile neutropenia, hypotension, tachycardia, diarrhea, nausea, headache, chills, upper respiratory tract infection, encephalopathy, edema, dyspnea, and viral infections.1
The most common Grade 3 or 4 laboratory adverse reactions (incidence ≥50%) include decreased leukocyte count, neutrophil count, lymphocyte count, platelet count, and hemoglobin.1
Drug Interactions
Specific Drugs
It is essential that the manufacturer's labeling be consulted for more detailed information on interactions with this drug, including possible dosage adjustments. Interaction highlights:
Please see product labeling for drug interaction information.
Actions
Mechanism of Action
Idecabtagene vicleucel is a chimeric antigen receptor (CAR)-positive T cell therapy targeting B-cell maturation antigen (BCMA), which is expressed on the surface of normal and malignant plasma cells.1 The CAR construct includes an anti-BCMA scFv-targeting domain for antigen specificity, a transmembrane domain, a CD3-zeta T cell activation domain, and a 4-1BB costimulatory domain.1 Antigen-specific activation of idecabtagene vicleucel results in CAR-positive T cell proliferation, cytokine secretion, and subsequent cytolytic killing of BCMA-expressing cells.1
Advice to Patients
-
Advise the patient to read the FDA-approved patient labeling (Medication Guide).1
-
Advise patients that the risk of manufacturing failure is 2.1% (8/384 in the clinical studies).1 In case of a manufacturing failure, a second manufacturing of idecabtagene vicleucel may be attempted.1 In addition, while the patient awaits the product, additional anticancer treatment (not the lymphodepletion) may be necessary and may increase the risk of adverse events during the pre-infusion period, which could delay or prevent the administration of idecabtagene vicleucel.1
-
Inform patients of the risk of early death.1 In a clinical study, a higher proportion of patients experienced death within the first 9 months from randomization in the idecabtagene vicleucel arm compared to the standard regimens arm.1 This higher rate of early death was mainly observed before receiving idecabtagene vicleucel with the main reason being progression of multiple myeloma.1 There was also an increase in the rate of death from adverse events after idecabtagene vicleucel.1
-
Advise patients to seek immediate attention if Cytokine Release Syndrome (CRS) occurs.1 Signs or symptoms associated with CRS include fever, hypotension, tachycardia, chills, hypoxia, headache, and fatigue.1
-
Advise patients to seek immediate attention if neurologic toxicities occur.1 Signs or symptoms associated with neurologic events include encephalopathy, confusion, seizures, tremor, aphasia, delirium, and somnolence.1
-
Advise patients to seek immediate attention if signs or symptoms of infection occur.1
-
Advise patients to seek immediate attention if prolonged cytopenias occur.1 Signs or symptoms associated with bone marrow suppression include neutropenia, anemia, thrombocytopenia, and febrile neutropenia.1
-
Advise patients that secondary malignancies, including T cell malignancies, have occurred.1 Advise patients to contact Bristol-Myers Squibb at 1-888-805-4555 if they are diagnosed with a secondary malignancy.1
-
Advise patients of the need to have periodic monitoring of blood counts before and after idecabtagene vicleucel infusion.1
-
Advise patients of the need to refrain from driving or operating heavy or potentially dangerous machines until at least 8 weeks after idecabtagene vicleucel administration.1
Additional Information
AHFSfirstRelease™. For additional information until a more detailed monograph is developed and published, the manufacturer's labeling should be consulted. It is essential that the manufacturer's labeling be consulted for more detailed information on usual uses, dosage and administration, cautions, precautions, contraindications, potential drug interactions, laboratory test interferences, and acute toxicity.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Suspension, for IV infusion |
300 to 510 × 106 CAR-positive T cells |
Abecma (supplied in one or more infusion bags containing a frozen suspension of genetically modified autologous T cells in 5% DMSO) |
Celgene Corporation |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
References
1. Celgene Corporation. Abecma (idecabtagene vicleucel) INTRAVENOUS prescribing information. 2025 Mar. http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=b90c1fe7-f5cc-464e-958a-af36e9c26d7c
2. Food and Drug Administration. Orphan designations pursuant to Section 526 of the Federal Food and Cosmetic Act as amended by the Orphan Drug Act (P.L. 97-414). Rockville, MD; from FDA website
3. Idecabtagene vicleucel (Abecma) for multiple myeloma. Med Lett Drugs Ther. 2022 Nov 14;64(1663):e190-e191. PMID: 36384767.
4. Food and Drug Administration. BLA Clinical Review for idecabtagene vicleucel (bb2121). From FDA website. https://www.fda.gov/vaccines-blood-biologics/abecma-idecabtagene-vicleucel
5. Munshi NC, Anderson LD Jr, Shah N et al. Idecabtagene Vicleucel in Relapsed and Refractory Multiple Myeloma. N Engl J Med. 2021 Feb 25;384(8):705-716. doi: 10.1056/NEJMoa2024850. PMID: 33626253.
6. Rodriguez-Otero P, Ailawadhi S, Arnulf B et al. Ide-cel or Standard Regimens in Relapsed and Refractory Multiple Myeloma. N Engl J Med. 2023 Mar 16;388(11):1002-1014. doi: 10.1056/NEJMoa2213614. Epub 2023 Feb 10. PMID: 36762851.
10. Santomasso BD, Nastoupil LJ, Adkins S et al. Management of Immune-Related Adverse Events in Patients Treated With Chimeric Antigen Receptor T-Cell Therapy: ASCO Guideline. J Clin Oncol. 2021 Dec 10;39(35):3978-3992. doi: 10.1200/JCO.21.01992. Epub 2021 Nov 1. Erratum in: J Clin Oncol. 2022 Mar 10;40(8):919. PMID: 34724386.
11. Shahid Z, Jain T, Dioverti V et al. Best Practice Considerations by The American Society of Transplant and Cellular Therapy: Infection Prevention and Management After Chimeric Antigen Receptor T Cell Therapy for Hematological Malignancies. Transplant Cell Ther. 2024 Oct;30(10):955-969. doi: 10.1016/j.jtct.2024.07.018. Epub 2024 Jul 30. PMID: 39084261.
12. Dhakal B, Shah N, Kansagra A et al. ASTCT Clinical Practice Recommendations for Transplantation and Cellular Therapies in Multiple Myeloma. Transplant Cell Ther. 2022 Jun;28(6):284-293. doi: 10.1016/j.jtct.2022.03.019. Epub 2022 Mar 17. PMID: 35306217.
13. Lin Y, Qiu L, Usmani S et al. Consensus guidelines and recommendations for the management and response assessment of chimeric antigen receptor T-cell therapy in clinical practice for relapsed and refractory multiple myeloma: a report from the International Myeloma Working Group Immunotherapy Committee. Lancet Oncol. 2024 Aug;25(8):e374-e387. doi: 10.1016/S1470-2045(24)00094-9. Epub 2024 May 28. Erratum in: Lancet Oncol. 2024 Aug;25(8):e336. doi: 10.1016/S1470-2045(24)00337-1. PMID: 38821074.
Related/similar drugs
Biological Products Related to idecabtagene vicleucel
Find detailed information on biosimilars for this medication.
Frequently asked questions
More about idecabtagene vicleucel
- Check interactions
- Compare alternatives
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- En español