Afatinib (Monograph)
Brand name: Gilotrif
Drug class: Antineoplastic Agents
- Kinase Inhibitors
- Receptor Tyrosine Kinase Inhibitors
- Tyrosine Kinase Inhibitors
Chemical name: (2E)-N-[4-[(3-Chloro-4-fluorophenyl)amino]-7-[[(3S)-tetrahydro-3-furanyl]oxy]-6-quinazolinyl]-4-(dimethylamino)-2-butenamide (2Z)-2-butenedioate (1:2)
Molecular formula: C24H25ClFN5O3•2C4H4O4
CAS number: 850140-73-7
Introduction
Antineoplastic agent; a second-generation inhibitor of receptor tyrosine kinases.
Uses for Afatinib
Non-small Cell Lung Cancer (NSCLC)
First-line treatment of metastatic NSCLC in patients with tumors positive for nonresistant epidermal growth factor receptor (EGFR) mutations (e.g., exon 19 deletions [del19], exon 21 substitution [L858R] mutations) as detected by an FDA-approved diagnostic test. Nonresistant EGFR mutations are those where efficacy of afatinib may be predicted by a clinically meaningful reduction in tumor size at the recommended dosage of the drug and/or inhibition of cellular proliferation or EGFR tyrosine kinase phosphorylation is expected at afatinib concentrations sustainable at the recommended dosage.
Treatment of metastatic squamous NSCLC that has progressed following therapy with platinum-based chemotherapy (designated an orphan drug by FDA for this use).
Safety and efficacy not established in patients with resistant EGFR mutations.
American Society of Clinical Oncology (ASCO)/Ontario Health (OH; formerly known as Cancer Care Ontario) guideline on treatment of stage IV NSCLC with driver alterations including EGFR mutations states that afatinib can be offered as a treatment option in patients with EGFR mutations when first-line treatment with osimertinib is not available.
ASCO guideline on systemic therapy for patients with stage IV NSCLC states that a recommendation for or against use of afatinib in patients with squamous cell carcinoma who are not eligible for further therapy cannot be made due to the minor survival gain compared with erlotinib and the potential benefit of therapy with immune checkpoint inhibitors.
Other Uses
Has been used for the treatment of malignant brain and central nervous system tumors† [off-label] and pancreatic cancer† [off-label].
Afatinib Dosage and Administration
General
Pretreatment Screening
-
Confirm nonresistant EGFR mutation-positive (e.g., del19, L858R) NSCLC by an FDA-approved diagnostic test prior to initiating therapy.
-
Verify pregnancy status in females of reproductive potential prior to initiating therapy.
Patient Monitoring
-
Periodically monitor liver function.
-
Monitor for diarrhea.
Administration
Oral Administration
Administer orally once daily. Administer on an empty stomach (at least 1 hour before or 2 hours after a meal).
If a dose of afatinib is missed, take the prescribed dose as soon as possible unless the next dose is within 12 hours; an additional dose should not be administered to replace the missed dose.
Dosage
Available as afatinib dimaleate; dosage expressed in terms of afatinib.
Adults
NSCLC
First-line Treatment of Metastatic NSCLC
Oral40 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Previously Treated Metastatic Squamous NSCLC
Oral40 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Dosage Modification
Dosage reduction, temporary interruption, or permanent discontinuance of therapy may be necessary.
Permanently discontinue therapy in patients who develop life-threatening bullous, blistering, or exfoliating skin lesions; interstitial lung disease; severe drug-induced hepatic impairment; GI perforation; persistent ulcerative keratitis; or symptomatic left ventricular dysfunction. Also permanently discontinue therapy if severe or intolerable adverse reactions occur at a dosage of 20 mg daily.
Grade 3 or 4 Toxicity
If grade 3 or 4 toxicity occurs, temporarily interrupt afatinib therapy. When toxicity resolves completely or improves to grade 1, resume therapy at a reduced dosage (i.e., 10 mg less than the daily dosage used prior to the event).
Diarrhea
If grade 2 diarrhea persists for 2 or more consecutive days despite anti-diarrheal therapy or grade 3 or greater diarrhea occurs, temporarily interrupt afatinib therapy. When diarrhea improves to grade 1 or less, resume therapy at a reduced dosage (i.e., 10 mg less than the daily dosage used prior to the event).
Dermatologic Toxicity
If intolerable or prolonged (lasting >7 days) grade 2 cutaneous reactions or grade 3 cutaneous reactions occur, temporarily interrupt afatinib therapy. When cutaneous reactions improve to grade 1 or less, resume therapy at a reduced dosage (i.e., 10 mg less than the daily dosage used prior to the event).
If life-threatening bullous, blistering, or exfoliating lesions occur, permanently discontinue therapy.
Special Populations
Hepatic Impairment
Mild or moderate hepatic impairment (Child-Pugh class A or B): No adjustment of initial dosage needed.
Severe hepatic impairment (Child-Pugh class C): Monitor closely and adjust dosage if not tolerated.
Renal Impairment
Mild or moderate renal impairment (eGFR 30–89 mL/minute per 1.73 m2): No adjustment of initial dosage needed.
Severe renal impairment (eGFR 15–29 mL/minute per 1.73 m2): Reduce dosage to 30 mg once daily.
Geriatric Patients
No specific dosage recommendations at this time.
Cautions for Afatinib
Contraindications
-
Manufacturer states none known.
Warnings/Precautions
Diarrhea
Diarrhea resulting in dehydration with or without renal impairment, sometimes fatal, reported. Diarrhea occurred in up to 96% of patients and was severe (grade 3) in up to 15% of patients receiving afatinib. Diarrhea generally occurred within 6 weeks of initiating therapy.
If persistent or severe diarrhea occurs, temporarily interrupt therapy and reduce subsequent dosage.
Provide patients with antidiarrheal therapy (e.g., loperamide) for subsequent home use as needed. Advise patients to take antidiarrheal agent at onset of diarrhea and until loose bowel movements have ceased for 12 hours.
Dermatologic Effects
Cutaneous reactions (i.e., rash, erythema, acneiform rash) reported in up to 90% of patients receiving afatinib. Grade 3 cutaneous reactions (characterized by bullous, blistering, and exfoliating lesions) and grade 1–3 palmar-plantar erythrodysesthesia (hand-foot syndrome) also reported. Toxic epidermal necrolysis and Stevens-Johnson syndrome reported during postmarketing experience.
May manage afatinib-associated rash with topical or systemic corticosteroids, anti-infectives, or antihistamines.
If severe or persistent cutaneous reactions occur, temporarily interrupt therapy and reduce subsequent dosage.
Permanently discontinue afatinib in patients who develop life-threatening bullous, blistering, or exfoliating lesions, or if toxic epidermal necrolysis or Stevens-Johnson syndrome is suspected.
Pulmonary Effects
Interstitial lung disease or interstitial lung disease-like events (e.g., lung infiltration, pneumonitis, ARDS, allergic alveolitis), sometimes fatal, reported. Incidence of interstitial lung disease reportedly higher in Asian patients compared with non-Asian patients.
Temporarily interrupt therapy if interstitial lung disease is suspected. If diagnosis of interstitial lung disease is confirmed, permanently discontinue afatinib.
Hepatic Toxicity
Abnormal liver function tests, sometimes fatal, reported in up to 50% of patients. Serious, fatal reaction have been reported.
Perform liver function tests periodically during therapy. Temporarily interrupt therapy in patients who develop worsening of liver function. Permanently discontinue afatinib in patients who develop severe hepatic impairment.
GI Perforation
GI perforation has been reported.
Monitor patients at high risk. Permanently discontinue in patients who develop GI perforation.
Ocular Effects
Keratitis (characterized as acute or worsening eye inflammation, lacrimation, light sensitivity, blurred vision, eye pain, and/or red eye), including grade 3 keratitis, reported.
Temporarily interrupt therapy if keratitis is suspected; if diagnosis of keratitis is confirmed, weigh potential benefit against risks of continued therapy. Temporarily interrupt or discontinue therapy in patients with confirmed ulcerative keratitis; permanently discontinue afatinib in patients with persistent ulcerative keratitis.
Use with caution in patients with a history of keratitis, ulcerative keratitis, or severe dry eye. Contact lens use is a risk factor for development of keratitis and ulceration.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. Embryofetal toxicity (e.g., abortion) and teratogenicity demonstrated in animals. Verify pregnancy status of females of reproductive potential prior to initiating therapy. Pregnancy should be avoided during therapy and for ≥2 weeks after drug discontinuance. If used during pregnancy, apprise of potential fetal hazard.
Cardiovascular Effects
Left ventricular dysfunction reported. Permanently discontinue afatinib if symptomatic left ventricular dysfunction occurs.
Substantial (i.e., >20 msec) increases in mean corrected QT (QTc) interval not observed in patients with relapsed or refractory solid tumors receiving multiple doses of afatinib (50 mg once daily).
Impairment of Fertility
Based on animal studies, may impair female and male fertility.
Specific Populations
Pregnancy
May cause fetal harm.
Lactation
Distributed into milk in rats; not known whether afatinib distributes into human milk or affects milk production or nursing infant. Discontinue nursing during therapy and for 2 weeks after drug is discontinued.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
First-line treatment of metastatic NSCLC: Insufficient experience to determine whether patients ≥65 years of age respond differently than younger adults.
Previously treated metastatic squamous NSCLC: No overall differences in safety compared with younger adults; however, overall survival benefit appears to be reduced.
Hepatic Impairment
Systemic exposure not affected by mild or moderate hepatic impairment (Child-Pugh class A or B).
Not studied in patients with severe hepatic impairment (Child-Pugh class C); therefore, monitor closely.
Renal Impairment
Peak plasma concentrations and systemic exposure increased by severe renal impairment (eGFR 15–29 mL/minute per 1.73 m2); dosage adjustment necessary.
Peak plasma concentrations not affected by moderate renal impairment (eGFR 30–59 mL/minute per 1.73 m2), but systemic exposure increased.
Not studied in patients with eGFR <15 mL/minute per 1.73 m2 or in those receiving dialysis.
Common Adverse Effects
Adverse reactions occurring in ≥20% of patients: Diarrhea, rash/acneiform dermatitis, stomatitis, paronychia, dry skin, decreased appetite, nausea, vomiting, pruritus.
Drug Interactions
Does not inhibit or induce CYP isoenzyme 1A2, 2B6, 2C8, 2C9, 2C19, or 3A4 in vitro. CYP-mediated mechanisms play a minor role in overall metabolism.
Substrate and inhibitor of P-glycoprotein (P-gp) and ABCG2 (breast cancer resistance protein [BCRP]) in vitro.
Drugs Affecting Hepatic Microsomal Enzymes
CYP inhibitors or inducers: Clinically important pharmacokinetic interactions unlikely.
Drugs Metabolized by Hepatic Microsomal Enzymes
CYP substrates: Clinically important pharmacokinetic interactions unlikely.
Drugs Affecting the P-glycoprotein Transport System
P-gp inhibitors: Possible pharmacokinetic interaction (increased systemic exposure to afatinib). Reduce dosage of afatinib if not tolerated.
P-gp inducers: Possible pharmacokinetic interaction (decreased systemic exposure to afatinib). Increase dosage of afatinib as tolerated.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amiodarone |
Possible increased systemic exposure to afatinib |
Reduce afatinib dosage by 10 mg daily if not tolerated If amiodarone (a P-gp inhibitor) is discontinued, resume afatinib at the dosage used prior to initiation of amiodarone as tolerated |
|
Antiangiogenic agents |
May increase risk of GI perforation |
|
|
Antifungals, azoles (e.g., itraconazole, ketoconazole) |
P-gp inhibitors: Possible increased systemic exposure to afatinib |
Reduce afatinib dosage by 10 mg daily if not tolerated If the P-gp inhibitor is discontinued, resume afatinib at the dosage used prior to initiation of the P-gp inhibitor as tolerated |
|
Antiretrovirals, HIV protease inhibitors (e.g., nelfinavir, ritonavir, saquinavir) |
P-gp inhibitors: Possible increased systemic exposure to afatinib Ritonavir: Afatinib AUC and peak plasma concentration increased by 48 and 39%, respectively, when ritonavir administered 1 hour prior to afatinib; no substantial effect on afatinib AUC when ritonavir administered concomitantly with or 6 hours following afatinib |
Reduce afatinib dosage by 10 mg daily if not tolerated If the P-gp inhibitor is discontinued, resume afatinib at the dosage used prior to initiation of the P-gp inhibitor as tolerated |
|
Carbamazepine |
Possible decreased systemic exposure to afatinib |
Increase afatinib dosage by 10 mg daily as tolerated If carbamazepine (a P-gp inducer) is discontinued, resume afatinib (2–3 days following discontinuance of carbamazepine) at the dosage used prior to initiation of carbamazepine |
|
Cisplatin |
No substantial effect on pharmacokinetics of cisplatin |
|
|
Corticosteroids |
May increase risk of GI perforation |
|
|
Cyclosporine |
Possible increased systemic exposure to afatinib |
Reduce afatinib dosage by 10 mg daily if not tolerated If cyclosporine (a P-gp inhibitor) is discontinued, resume afatinib at the dosage used prior to initiation of cyclosporine as tolerated |
|
Erythromycin |
Possible increased systemic exposure to afatinib |
Reduce afatinib dosage by 10 mg daily if not tolerated If erythromycin (a P-gp inhibitor) is discontinued, resume afatinib at the dosage used prior to initiation of erythromycin as tolerated |
|
Fluorouracil |
No substantial effect on pharmacokinetics of fluorouracil |
|
|
Nonsteroidal anti-inflammatory agents (NSAIAs) |
May increase risk of GI perforation |
|
|
Paclitaxel |
No substantial effect on pharmacokinetics of paclitaxel |
|
|
Phenobarbital |
Possible decreased systemic exposure to afatinib |
Increase afatinib dosage by 10 mg daily as tolerated If phenobarbital (a P-gp inducer) is discontinued, resume afatinib (2–3 days following discontinuance of phenobarbital) at the dosage used prior to initiation of phenobarbital |
|
Phenytoin |
Possible decreased systemic exposure to afatinib |
Increase afatinib dosage by 10 mg daily as tolerated If phenytoin (a P-gp inducer) is discontinued, resume afatinib (2–3 days following discontinuance of phenytoin) at the dosage used prior to initiation of phenytoin |
|
Quinidine |
Possible increased systemic exposure to afatinib |
Reduce afatinib dosage by 10 mg daily if not tolerated If quinidine (a P-gp inhibitor) is discontinued, resume afatinib at the dosage used prior to initiation of quinidine |
|
Rifampin |
Afatinib AUC and peak plasma concentration decreased by 34 and 22%, respectively |
Increase afatinib dosage by 10 mg daily as tolerated If rifampin (a P-gp inducer) is discontinued, resume afatinib (2–3 days following discontinuance of rifampin) at the dosage used prior to initiation of rifampin |
|
St. John's wort (Hypericum perforatum) |
Possible decreased systemic exposure to afatinib |
Increase afatinib dosage by 10 mg daily as tolerated If St. John's wort (a P-gp inducer) is discontinued, resume afatinib (2–3 days following discontinuance of the herbal supplement) at the dosage used prior to initiation of the herbal supplement |
|
Tacrolimus |
Possible increased systemic exposure to afatinib |
Reduce afatinib dosage by 10 mg daily if not tolerated If tacrolimus (a P-gp inhibitor) is discontinued, resume afatinib at the dosage used prior to initiation of tacrolimus as tolerated |
|
Verapamil |
Possible increased systemic exposure to afatinib |
Reduce afatinib dosage by 10 mg daily if not tolerated If verapamil (a P-gp inhibitor) is discontinued, resume afatinib at the dosage used prior to initiation of verapamil as tolerated |
Afatinib Pharmacokinetics
Absorption
Bioavailability
Geometric mean bioavailability of afatinib tablets compared to the oral solution is 92%.
Peak plasma afatinib concentrations are attained about 2–5 hours after oral administration.
AUC and peak plasma concentration increase slightly more than dose proportionally over a dosage range of 20–50 mg.
Steady-state concentrations are achieved within 8 days of repeated administration, resulting in an accumulation of 2.8 fold (for AUC) and 2.1 fold (for peak plasma concentration).
Food
Administration with a high-fat meal decreased peak plasma concentration and AUC by 50 and 39%, respectively, compared with fasted state.
Special Populations
Mild or moderate hepatic impairment (Child-Pugh class A or B) does not affect exposure to afatinib.
Severe renal impairment (eGFR 15–29 mL/minute per 1.73 m2) increases peak plasma concentrations and AUC by 22 and 50%, respectively.
Moderate renal impairment (eGFR 30–59 mL/minute per 1.73 m2) increases AUC by 22% but does not affect peak plasma concentrations.
Distribution
Extent
Not known whether afatinib is distributed into milk.
Plasma Protein Binding
Approximately 95%.
Elimination
Metabolism
CYP-mediated mechanisms have a minor role in overall metabolism.
Elimination Route
Eliminated in feces (85%) and urine (4%), mostly (88%) as unchanged drug.
Half-life
37 hours.
Special Populations
Age, weight, sex, and race do not substantially affect exposure to afatinib.
Stability
Storage
Oral
Tablets
25°C (excursions permitted between 15–30°C). Store in original container and protect from excessive humidity and light.
Actions
-
Covalently binds to the kinase domains of epidermal growth factor receptor (EGFR/HER1/ErbB1), HER2/ErbB2, and HER4/ErbB4, and irreversibly inhibits tyrosine kinase phosphorylation, resulting in downregulation of ErbB signaling.
-
Inhibits phosphorylation and in vitro proliferation of cell lines expressing wild-type EGFR and cell lines expressing del19 or L858R mutations, including other less common EGFR-activating (nonresistant) mutations.
-
Inhibits proliferation of cell lines that overexpress HER2 in vitro.
-
Inhibits tumor growth in mice with tumors overexpressing wild-type EGFR, HER2, or the EGFR L858R/T790M mutation.
-
Appears to be approximately 100 times more potent than gefitinib against EGFR L858R-T790M EGFR mutations and as potent as lapatinib against HER2 in vitro.
Advice to Patients
-
Importance of advising patients to take afatinib on an empty stomach, at least 1 hour before or 2 hours after a meal. If a dose is missed, instruct patients to take the missed dose as soon as it is remembered unless it is within 12 hours of the next scheduled dose, in which case they should not take the missed dose. Advise patients to not take 2 doses at the same time to make up for a missed dose.
-
Risk of diarrhea; importance of advising patient about appropriate countermeasures to manage diarrhea. Importance of informing clinician if diarrhea develops and promptly seeking medical attention if severe or persistent diarrhea occurs.
-
Risk of cutaneous reactions. Importance of limiting exposure to sunlight by wearing protective clothing and using sunscreen (minimum SPF of 15).
-
Risk of interstitial lung disease. Importance of immediately informing clinician if new or worsening respiratory symptoms occur or if any combination of the following symptoms occur: difficulty breathing, shortness of breath, cough, and/or fever.
-
Risk of hepatotoxicity and importance of periodic liver function test monitoring. Importance of immediately reporting any manifestations of hepatotoxicity (e.g., jaundice, unusually dark or “tea-colored” urine, right upper quadrant pain, fatigue, bleeding or bruising more easily than normal).
-
Instruct patients to seek medical attention if severe abdominal pain occurs.
-
Risk of ocular effects. Importance of immediately informing clinician if ocular problems (e.g., eye pain, swelling, redness, blurred vision, other vision changes) occur.
-
Risk of left ventricular dysfunction; importance of immediately informing clinicians if new-onset or worsening shortness of breath, exercise intolerance, cough, fatigue, peripheral edema, palpitations, or sudden weight gain occurs.
-
Risk of fetal harm. Necessity of advising females of reproductive potential to use adequate methods of contraception while receiving afatinib and for at least 2 weeks after the drug is discontinued. Importance of patients informing their clinicians if they are pregnant or think they may be pregnant.
-
Risk of impaired female and male fertility.
-
Importance of advising females to avoid breast-feeding while receiving afatinib therapy and for 2 weeks after discontinuance of therapy.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Afatinib is available only be obtained through specialty distributors. Consult the manufacturer's website for specific availability information.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
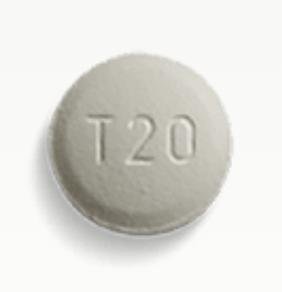
Oral |
Tablets, film-coated |
20 mg (of afatinib) |
Gilotrif |
Boehringer Ingelheim |
|
30 mg (of afatinib) |
Gilotrif |
Boehringer Ingelheim |
||
|
40 mg (of afatinib) |
Gilotrif |
Boehringer Ingelheim |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 15, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- How long can I take Gilotrif (afatinib) for?
- Is Gilotrif (afatinib) a chemotherapy drug?
- How does Gilotrif (afatinib) work?
More about afatinib
- Check interactions
- Compare alternatives
- Reviews (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: multikinase inhibitors
- Breastfeeding
- En español