Heart Block
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is heart block?
Heart block is a problem with the flow of electrical signals in your heart. The electrical signals control the way your heart beats. With heart block, these signals are delayed or interrupted completely. This affects the way your heart beats.
What are the types of heart block?
- First-degree atrioventricular (AV) block slows the time it takes the electrical signal to travel from the atria to the ventricles.
- Second-degree AV block caues the electrical signal to slow with each beat until it stops completely. The block may happen from time to time. It may also happen when you are do a certain activity, such as exercise.
- Third-degree AV block is also known as Complete Heart Block (CHB). CHB prevents the signals from the atria from reaching the ventricles. The ventricles will beat on their own, but it is a very slow beat. This is a life-threatening condition.
What increases my risk for heart block?
- Past heart attack or heart failure
- Heart valve conditions or surgery on your heart valves
- Some medicines, or being exposed to toxins
- Lyme disease
- Older age
What are the signs and symptoms of heart block?
Signs and symptoms depend on how severe your heart block is. You may not have any symptoms or you may have any of the following:
- Fatigue or confusion
- Lightheadedness, dizziness, or fainting
- Shortness of breath
- Chest pain
Related medications
How is heart block diagnosed?
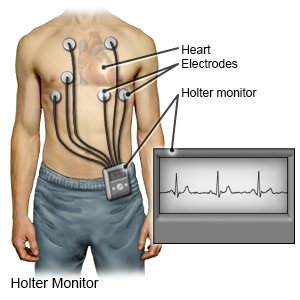
Healthcare providers will try to find the cause of your heart block. An EKG will be used to diagnose your heart block. An EKG is used to check the electrical activity in your heart. You may need to wear an EKG monitor for a few days while you do your daily activities. This monitor is also called a Holter monitor. You may need any of the following to find the cause of your heart block:
- Blood tests may be done to check for infection, measure your electrolyte levels, or check for other causes of heart block.
- A chest x-ray will show the size of your heart and check for fluid in your lungs.
- A stress test helps healthcare providers see the changes that take place in your heart while it is under stress. Healthcare providers may place stress on your heart with exercise or medicine.
 |
How is heart block treated?
Treatment depends on how severe your heart block is. You may not need any treatment. When symptoms are severe, you may need the following:
- Heart medicine may be given to help your heart beat correctly until a pacemaker can be placed.
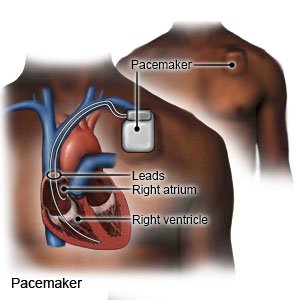
- A pacemaker is a small device that helps your heart beat at a normal speed and in a regular rhythm. You may need a temporary or permanent pacemaker. A temporary pacemaker is a short-term treatment in the hospital. The pacemaker is applied to your skin with sticky pads or placed into a vein in your neck or chest. A pacing device helps keep your heartbeat stable. A permanent pacemaker is put under the skin of your chest or abdomen during surgery. A tiny battery creates electrical impulses that keep your heart rate regular.
- Treatment of the cause of your heart block may be done if it can reverse the effects. For example, IV antibiotics may be given for Lyme Disease.
Call your local emergency number (911 in the US) if:
You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
When should I call my doctor?
- Your symptoms are worse or happen more often.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Heart Block
Treatment options
- Medications for Arrhythmia
- Medications for Heart Block
- Medications for Long QT Syndrome
- Medications for Preexcitation Syndrome
- Medications for Tachyarrhythmia
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
