Wolff-Parkinson-White Syndrome
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is Wolff-Parkinson-White syndrome?
Wolff-Parkinson-White (WPW) syndrome is a condition that causes tachycardia (fast heartbeat). A normal heartbeat is about 60 to 100 beats per minute. WPW causes 100 or more heartbeats per minute. WPW develops because an extra piece of heart muscle causes more electrical activity within your heart. WPW can develop for no known reason. Congenital heart disease or a family history of WPW can increase your risk.
What are the signs and symptoms of WPW?
You may have no symptoms, or you may have any of the following:
- Fast, irregular, fluttering, or pounding heartbeats
- Chest pain or trouble breathing
- Dizziness or feeling like you are going to faint
- Urinating more than usual, or sweating heavily
How is WPW diagnosed?
- An EKG is a test that measures the electrical activity of your heart. This may be the only way your healthcare provider knows you have WPW.
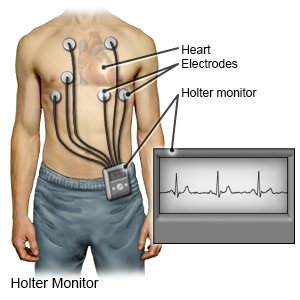
- A Holter monitor is also called a portable EKG monitor. It shows your heart's electrical activity while you do your usual activities. The monitor is a small battery-operated device that you wear. It will show how fast your heart beats and if it beats in a regular pattern.
- Electrophysiologic studies (EPS) test the electrical activity of your heart.
How is WPW treated?
Treatment will depend on how severe your symptoms are, and how often you have them. You may only need to be observed by your healthcare provider if you are not having symptoms. You may need any of the following:
- Medicines may be given to slow or regulate your heartbeat.
- Radiofrequency ablation is a procedure used to send energy to the area of your heart that has an electrical problem. The energy causes an area of the heart muscle to scar. This stops the electrical problem and allows your heart to beat normally.
- Cardioversion is a procedure used to give your heart an electrical shock. The shock may help put your heartbeat back into a normal rhythm. Cardioversion may be needed if other treatments do not work.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How can I stop an episode of WPW?
Your healthcare provider will teach you methods called vagal maneuvers that can slow your heartbeat during an episode. The methods may include coughing, gagging, holding your breath, or putting ice on your face.
What can I do to manage my WPW?
- Do not smoke. Smoking narrows blood vessels in your heart. Narrow blood vessels make your heart work harder. Smoking can also damage your heart. Ask your healthcare provider for information if you currently smoke and need help quitting.
- Carry medical alert identification. Wear jewelry or carry a card that says you have WPW. Ask your healthcare provider where to get these items.
- Exercise as directed. Exercise can cause WPW episodes. Ask your healthcare provider how much exercise you need each day and which exercises are safe for you. Ask if you can play sports.
- Limit caffeine. Caffeine can make your heartbeat faster.
When should I seek immediate care?
- You have chest pain.
- You have fast or abnormal heartbeats even after treatment.
- You feel dizzy or faint.
When should I contact my healthcare provider?
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Wolff-Parkinson-White Syndrome
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
