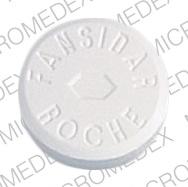
Pyrimethamine/sulfadoxine Disease Interactions
There are 12 disease interactions with pyrimethamine / sulfadoxine.
- Colitis
- Folate deficiency
- Hematologic toxicity
- Hypersensitivity reactions
- Liver disease
- Porphyria
- Renal dysfunction
- Liver disease
- Renal dysfunction
- Seizure disorders
- Crystalluria
- Urinary obstruction
Antibiotics (applies to pyrimethamine/sulfadoxine) colitis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Colitis/Enteritis (Noninfectious)
Clostridioides difficile-associated diarrhea (CDAD), formerly pseudomembranous colitis, has been reported with almost all antibacterial drugs and may range from mild diarrhea to fatal colitis. The most common culprits include clindamycin and lincomycin. Antibacterial therapy alters the normal flora of the colon, leading to overgrowth of C difficile, whose toxins A and B contribute to CDAD development. Morbidity and mortality are increased with hypertoxin-producing strains of C difficile; these infections can be resistant to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea after antibacterial use. Since CDAD has been reported to occur more than 2 months after antibacterial use, careful medical history is necessary. Therapy with broad-spectrum antibacterials and other agents with significant antibacterial activity should be administered cautiously in patients with history of gastrointestinal disease, particularly colitis; pseudomembranous colitis (generally characterized by severe, persistent diarrhea and severe abdominal cramps, and sometimes associated with the passage of blood and mucus), if it occurs, may be more severe in these patients and may be associated with flares in underlying disease activity. Antibacterial drugs not directed against C difficile may need to be stopped if CDAD is suspected or confirmed. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C difficile, and surgical evaluation should be started as clinically indicated.
Pyrimethamine (applies to pyrimethamine/sulfadoxine) folate deficiency
Major Potential Hazard, High plausibility. Applicable conditions: Malabsorption Syndrome, Acute Alcohol Intoxication, Anemia Associated with Folate Deficiency
Pyrimethamine is a folate antagonist. The use of pyrimethamine is contraindicated in patients with megaloblastic anemia caused by folate deficiency. Pyrimethamine should be used with caution in patients with malabsorption syndrome, alcoholism, pregnancy, and in those receiving other folate depleting drugs. Monitoring CBCs and platelet counts are recommended. If signs of folic acid deficiency occur, the drug dosage should be reduced or discontinued. Leucovorin may need to be administered to reverse folic acid deficiency.
Sulfonamides (applies to pyrimethamine/sulfadoxine) hematologic toxicity
Major Potential Hazard, Moderate plausibility. Applicable conditions: Bone Marrow Depression/Low Blood Counts, G-6-PD Deficiency
The use of sulfonamides has been associated with hematologic toxicity, including methemoglobinemia, sulfhemoglobinemia, leukopenia, granulocytopenia, eosinophilia, hemolytic anemia, aplastic anemia, purpura, clotting disorder, thrombocytopenia, hypofibrinogenemia, and hypoprothrombinemia. Acute dose-related hemolytic anemia may occur during the first week of therapy due to sensitization, while chronic hemolytic anemia may occur with prolonged use. Patients with glucose-6-phosphate dehydrogenase (G-6-PD) deficiency should be observed closely for signs of hemolytic anemia. Therapy with sulfonamides should be administered cautiously in patients with preexisting blood dyscrasias or bone marrow suppression. Complete blood counts should be obtained regularly, especially during prolonged therapy (>2 weeks), and patients should be instructed to immediately report any signs or symptoms suggestive of blood dyscrasia such as fever, sore throat, local infection, bleeding, pallor, dizziness, or jaundice.
Sulfonamides (applies to pyrimethamine/sulfadoxine) hypersensitivity reactions
Major Potential Hazard, Moderate plausibility. Applicable conditions: Asthma, HIV Infection, Allergies
The use of sulfonamides is associated with large increases in the risk of Stevens-Johnson syndrome, toxic epidermal necrolysis and other serious dermatologic reactions, although these phenomena are rare as a whole. Hepatitis, pneumonitis, and interstitial nephritis have also occurred in association with sulfonamide hypersensitivity. Therapy with sulfonamides should be administered cautiously in patients with severe allergies, bronchial asthma or AIDS, since these patients may be at increased risk for potentially severe hypersensitivity reactions. Patients should be instructed to promptly report signs and symptoms that may precede the onset of cutaneous manifestations of the Stevens-Johnson syndrome, such as high fever, severe headache, stomatitis, conjunctivitis, rhinitis, urethritis, and balanitis. Sulfonamide therapy should be stopped at once if a rash develops.
Sulfonamides (applies to pyrimethamine/sulfadoxine) liver disease
Major Potential Hazard, Moderate plausibility.
Hepatotoxicity, including jaundice, diffuse hepatocellular necrosis, hypersensitivity hepatitis and hepatic failure, has rarely been reported in patients receiving sulfonamides. In addition, sulfonamides are partially metabolized by the liver and may accumulate in patients with hepatic impairment. Therapy with sulfonamides should be administered cautiously in patients with liver disease.
Sulfonamides (applies to pyrimethamine/sulfadoxine) porphyria
Major Potential Hazard, High plausibility.
The use of sulfonamides is contraindicated in patients with porphyria, since these drugs can precipitate an acute attack.
Sulfonamides (applies to pyrimethamine/sulfadoxine) renal dysfunction
Major Potential Hazard, High plausibility.
Sulfonamides and their metabolites are eliminated by the kidney. Patients with renal impairment may be at greater risk for adverse effects from sulfonamides due to decreased drug clearance. Dosage adjustments may be necessary and modifications should be based on the degree of renal impairment and severity of infection. Additionally, sulfonamides may cause renal toxicity secondary to crystalluria, including uro- and nephrolithiasis, nephritis, toxic nephrosis, hematuria, proteinuria, and elevated BUN and creatinine. Hydration (8 oz. glass of water with each dose and throughout the day) and adequate urinary output (> 1.5 L/day) should be maintained during sulfonamide administration. Renal function tests and urinalysis should be performed weekly or as often as indicated by the patient's status. Rarely, alkalinization of the urine is necessary.
Pyrimethamine (applies to pyrimethamine/sulfadoxine) liver disease
Moderate Potential Hazard, Moderate plausibility.
Pyrimethamine is extensively metabolized by the liver. Therapy with pyrimethamine should be administered cautiously in patients with liver disease.
Pyrimethamine (applies to pyrimethamine/sulfadoxine) renal dysfunction
Moderate Potential Hazard, Moderate plausibility.
Pyrimethamine and its metabolites are excreted in the urine. Therapy with pyrimethamine should be administered cautiously in patients with renal dysfunction.
Pyrimethamine (applies to pyrimethamine/sulfadoxine) seizure disorders
Moderate Potential Hazard, High plausibility. Applicable conditions: Seizures
The use of pyrimethamine has been associated with ataxia, tremors, and seizures. Therapy with pyrimethamine should be administered cautiously and in lower dosages in patients with seizure disorders.
Sulfonamides (applies to pyrimethamine/sulfadoxine) crystalluria
Moderate Potential Hazard, High plausibility. Applicable conditions: Dehydration, Diarrhea, Vomiting
Crystalluria can occur during sulfonamide therapy due to precipitation of the sulfonamide and/or its N4-acetyl metabolite in the urinary tract. Renal toxicity such as uro- and nephrolithiasis, nephritis, toxic nephrosis, hematuria, proteinuria, and elevated BUN and creatinine has been reported. Hydration (8 oz. glass of water with each dose and throughout the day) and adequate urinary output (> 1.5 L/day) should be maintained during sulfonamide administration. Patients who are dehydrated (e.g., due to severe diarrhea or vomiting) may be at increased risk for the development of crystalluria and lithiasis and should be encouraged to consume additional amounts of liquid or given intravenous fluid. Renal function tests and urinalysis should be performed weekly during prolonged therapy (> 2 weeks). Rarely, alkalinization of the urine is necessary.
Sulfonamides (applies to pyrimethamine/sulfadoxine) urinary obstruction
Moderate Potential Hazard, High plausibility. Applicable conditions: Urinary Retention
Sulfonamides are excreted and concentrated in the urine. Therapy with sulfonamides should be administered cautiously in patients with urinary obstruction or retention, since excessive drug accumulation may occur. These patients may also be at increased risk for sulfonamide crystalluria, which may be associated with renal toxicity such as uro- and nephrolithiasis, nephritis, toxic nephrosis, hematuria, proteinuria, and elevated BUN and creatinine. A urinary output of at least 1.5 L/day should be maintained during sulfonamide administration. Renal function tests and urinalysis should be performed weekly, especially during prolonged therapy (> 2 weeks).
Switch to professional interaction data
Pyrimethamine/sulfadoxine drug interactions
There are 153 drug interactions with pyrimethamine / sulfadoxine.
More about pyrimethamine / sulfadoxine
- pyrimethamine/sulfadoxine consumer information
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antimalarial combinations
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.