Minimally Invasive Maze Procedure
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
WHAT YOU NEED TO KNOW:
A minimally invasive maze procedure is used to treat atrial fibrillation.
 |
HOW TO PREPARE:
The week before your procedure:
- Arrange to have someone drive you home after the procedure.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine for the procedure, and when to stop. He or she will tell you which medicines to take or not take on the day of the procedure.
- Contrast liquid may be used during your procedure to help your surgeon see the blood vessels better. Tell him or her if you have ever had an allergic reaction to contrast liquid.
- You may need to stop driving, lifting anything heavy, or doing strenuous or tiring activities.
- You may need to have an EKG, electrophysiologic studies (EPS), or transthoracic and transesophageal electrocardiogram (TEE). You may also need to have a cardiac catheterization, CT scan, chest x-ray, and blood tests.
- Your surgeon may give you heart medicines to help control your irregular heartbeat. Ask him or her for more information about these medicines.
The night before your procedure:
You may be told not to eat or drink anything after midnight.
The day of your procedure:
- You or a close family member will be asked to sign a legal document called a consent form. It gives healthcare providers permission to do the procedure or surgery. It also explains the problems that may happen, and your choices. Make sure all your questions are answered before you sign this form.
- Take only the medicines your surgeon told you to take.
- An IV will be put into a vein. You may get medicine or liquids through the IV.
- An anesthesiologist will talk to you before your surgery. You may need medicine to keep you asleep or numb an area of your body during surgery. Tell healthcare providers if you or anyone in your family has had a problem with anesthesia in the past.
WHAT WILL HAPPEN:
What will happen:
- A catheter (tube) will be threaded into your heart through a blood vessel in your chest, neck, arm, or leg. Another tube with a small ultrasound sensor on the end may also be moved down into your esophagus. This will allow your surgeon to see your heart clearly.
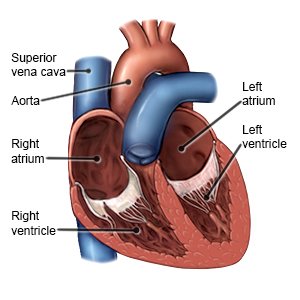
- Your surgeon will make a small incision in your chest to insert the endoscope through. Two smaller incisions will also be made between the ribs to insert the other instruments. Small incisions will be made in the right and left atria (upper chambers) of your heart and then sewn closed. This will form scar tissue and a maze where the impulses can travel in only 1 direction.
- The openings and incisions in your chest will be closed. A bandage will be placed over your incision to control bleeding.
After your procedure:
You will be taken to a room to rest until you are fully awake. Healthcare providers will monitor you closely for any problems. Do not get out of bed until your healthcare provider says it is okay. When your healthcare provider sees that you are okay, you will be able to go home or be taken to your hospital room. The catheter used during the procedure will be removed. A tight pressure bandage will cover the incision. A healthcare provider may remove the bandages soon after the procedure to check the area.
CONTACT YOUR HEALTHCARE PROVIDER IF:
- You have a fever.
- You get a cold or the flu.
- You have questions or concerns about your procedure.
Seek Care Immediately if
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
Risks
Problems may happen during this procedure that may lead to an open chest surgery. During this procedure, your heartbeat may stop. This may decrease blood flow more and lead to a heart attack. A blood vessel or your atria may get injured, causing a large amount of blood loss. You could also have trouble breathing, an infection, or bleed more than expected after this procedure. You may develop a life-threatening blood clot.
Related medications
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
