Methocarbamol (Monograph)
Brand name: Robaxin
Drug class: Centrally Acting Skeletal Muscle Relaxants
VA class: MS200
Chemical name: 1-Carbamate-3-(2-methoxyphenoxy)-1,2-propanediol
Molecular formula: C11H15NO5
CAS number: 532-03-6
Introduction
Centrally acting skeletal muscle relaxant.
Uses for Methocarbamol
Muscular Conditions
Adjunct to rest, physical therapy, analgesics, and other measures for the relief of discomfort associated with acute, painful musculoskeletal conditions.
If pharmacologic therapy is required for acute low back pain (usually a benign and self-limiting condition), experts state that an NSAIA or skeletal muscle relaxant may be considered. Skeletal muscle relaxants may provide small improvements in pain relief, but are associated with a high incidence of adverse effects (e.g., CNS effects). Use with caution after weighing risks against benefits.
Various skeletal muscle relaxants appear to have comparable efficacy for low back pain relief.
Methocarbamol is ineffective in the treatment of skeletal muscle hyperactivity secondary to chronic neurologic disorders (e.g., cerebral palsy) and other dyskinesias.
Tetanus
Has been used as an adjunct to debridement, tetanus antitoxin, penicillin, tracheotomy, fluid and electrolyte replacement, and supportive therapy in the management of tetanus. However, most authorities prefer other sedatives or muscle relaxants (e.g., diazepam) and, in severe cases, neuromuscular blocking agents.
Methocarbamol Dosage and Administration
Administration
Administer orally; may administer IV or IM when oral administration is not feasible or for severe musculoskeletal pain. Do not administer sub-Q.
Oral Administration
NG Tube
For administration via NG tube, crush tablets and suspend in water or saline solution.
IV Administration
For solution compatibility information, see Compatibility under Stability.
Administer undiluted by direct IV injection (at a rate not exceeding 3 mL/minute), or dilute and administer by IV infusion.
Patient should be recumbent during and for 10–15 minutes following IV administration.
Avoid extravasation; solution is hypertonic.
Blood aspirated into syringe does not mix with methocarbamol injection; either inject any blood in the syringe or stop the injection when the plunger reaches the blood.
Dilution
For IV infusion, dilute 1 g with up to 250 mL of 5% dextrose or 0.9% sodium chloride injection.
Rate of Administration
For direct IV injection, maximum rate of 3 mL/minute.
IM Administration
Administer no more than 500 mg (5 mL of the 100-mg/mL injection) into each gluteal region.
Dosage
Pediatric Patients
Tetanus
IV
Recommended minimum initial dose is 15 mg/kg or 500 mg/m2; may give additional doses of 15 mg/kg or 500 mg/m2 by direct IV injection or IV infusion every 6 hours, if necessary (maximum 1.8 g/m2 daily for 3 consecutive days).
Adults
Muscular Conditions
Oral
Usual initial dosage is 1.5 g 4 times daily for 2–3 days. For maintenance, decrease dosage to 4–4.5 g daily in 3–6 divided doses.
Patients with severe symptoms may require initial dosage of 8 g daily in divided doses.
IV or IM
Usually, 1 g as a single dose, followed by oral methocarbamol to maintain relief.
For more severe conditions or when oral administration is not feasible, additional doses of 1 g may be administered every 8 hours (maximum 3 g daily for 3 consecutive days). If necessary, may readminister IM or IV after a 48-hour drug-free interval.
Tetanus
IV, then Oral
Recommended initial dose is 1–2 g by direct IV injection; may administer additional 1–2 g by IV infusion (for total initial dose of up to 3 g).
Repeat dosage regimen every 6 hours until NG tube can be inserted. May then administer crushed tablets suspended in water or saline through NG tube. Up to 24 g daily (via NG tube) may be required.
Prescribing Limits
Pediatric Patients
Tetanus
IV
Maximum 1.8 g/m2 daily for 3 consecutive days.
Adults
Muscular Conditions
IV or IM
Maximum 3 g daily for 3 consecutive days.
Cautions for Methocarbamol
Contraindications
-
Injection contraindicated in patients with impaired renal function. (See Renal Impairment under Cautions.)
-
Known hypersensitivity to methocarbamol or any ingredient in the formulation.
Warnings/Precautions
Warnings
CNS Depression
Performance of activities requiring mental alertness or physical coordination may be impaired.
Possible additive effect with other CNS depressants and/or alcohol. (See Specific Drugs and Laboratory Tests under Interactions.)
Sensitivity Reactions
Anaphylactic reactions, angioedema, urticaria, pruritus, rash, skin eruptions, and conjunctivitis with nasal congestion have occurred.
General Precautions
Seizure Disorders
Although causal relationship not established, seizures reported during IV administration. Use injection with caution in patients with known or suspected seizure disorders.
Specific Populations
Pregnancy
Not known whether the drug can cause fetal harm or affect reproductive capacity. Fetal and congenital abnormalities reported following in utero exposure; animal reproductive studies not conducted. Do not use during pregnancy, particularly during early pregnancy, unless potential benefits outweigh possible risks.
Lactation
Distributed into milk in dogs; not known whether distributed into human milk. Use caution.
Pediatric Use
Safety and efficacy (other than IV use in the management of tetanus) not established in pediatric patients <16 years of age.
Geriatric Use
Because of risk of injury, skeletal muscle relaxants should generally be avoided in geriatric patients.
Renal Impairment
Polyethylene glycol vehicle of methocarbamol injection may worsen preexisting acidosis and urea retention; although amount present in preparation is well within limits of safety, caution is advised. Do not administer to patients with impaired renal function. (See Contraindications under Cautions.)
Common Adverse Effects
Drowsiness, dizziness, lightheadedness.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Anticholinesterase agents (e.g., pyridostigmine) |
Potential for severe weakness |
Use with caution in patients with myasthenia gravis |
|
CNS depressants (e.g., alcohol) |
Potential for additive CNS depression |
Use caution to avoid overdosage |
|
Tests for 5-hydroxyindolacetic acid (5-HIAA) in urine (nitrosonaphthol reagent in quantitative method of Udenfriend) |
False-positive results (color interference) |
|
|
Tests for vanillylmandelic acid (VMA) in urine by the screening method of Gitlow |
False-positive results (color interference) |
Methocarbamol Pharmacokinetics
Absorption
Bioavailability
Rapidly and almost completely absorbed following oral administration.
Onset
Usually within 30 minutes following oral administration.
Almost immediate after IV administration.
Distribution
Extent
Widely distributed in dogs, with highest concentrations in the kidney and liver.
Methocarbamol and/or its metabolites cross the placenta in dogs.
Distributed into milk in dogs; not known whether distributed into human milk.
Plasma Protein Binding
46–50%.
Elimination
Metabolism
Extensively metabolized, presumably in the liver, by dealkylation and hydroxylation.
Elimination Route
Eliminated principally in urine as metabolites (40–50% as glucuronide and sulfate conjugates, remainder as unidentified metabolites); small amount (10–15%) eliminated unchanged in urine. Very small amounts excreted in feces.
Half-life
0.9–1.8 hours.
Special Populations
In geriatric patients, half-life slightly prolonged.
In patients with renal impairment on maintenance dialysis, clearance decreased by 40% but no apparent increase in half-life.
In patients with cirrhosis secondary to alcohol abuse, clearance decreased by 70% and half-life increased to about 3.4 hours.
Stability
Storage
Oral
Tablets
Tight containers at 20–25°C. Protect from light and moisture.
Parenteral
Injection
20–25°C (may be exposed to 15–30°C).
Do not refrigerate after dilution. Precipitation and haze formation may occur if diluted solution is refrigerated. Haze formation in diluted solutions may be unpredictable; visually inspect all diluted solutions prior to administration regardless of storage conditions.
Compatibility
Parenteral
Solution Compatibility
|
Compatible |
|---|
|
Dextrose 5% in water |
|
Sodium chloride 0.9% |
Actions
-
CNS depressant with sedative and skeletal muscle relaxant effects.
-
Precise mechanism of action is not known; does not directly relax skeletal muscle and has minimal skeletal muscle relaxant effects. Beneficial effect probably is related to the drug’s sedative effect.
-
Unlike neuromuscular blocking agents, does not depress neuronal conduction, neuromuscular transmission, or muscle excitability.
Advice to Patients
-
Potential to impair mental alertness or physical coordination, especially with concomitant use of alcohol or other CNS depressants; use caution when driving or operating machinery.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
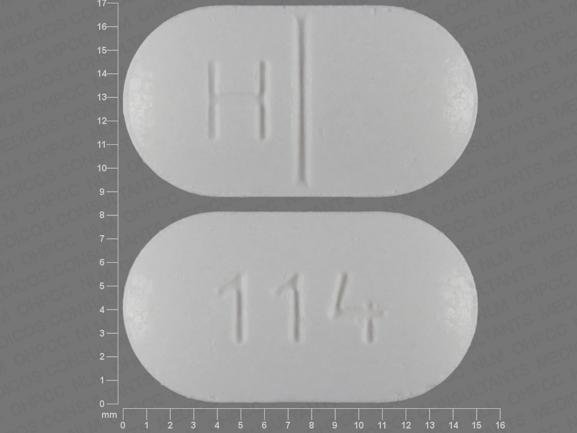
Oral |
Tablets |
500 mg* |
Methocarbamol Tablets |
|
|
750 mg* |
Methocarbamol Tablets |
|||
|
Tablets, film-coated |
500 mg |
Robaxin |
Endo |
|
|
750 mg |
Robaxin-750 |
Endo |
||
|
Parenteral |
Injection |
100 mg/mL |
Robaxin |
West-ward |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 24, 2020. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Flexeril
Flexeril (cyclobenzaprine) is a muscle relaxant used to treat skeletal muscle conditions such as ...
Valium
Valium is used to treat anxiety disorders, alcohol withdrawal symptoms, or muscle spasms. Learn ...
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
Robaxin
Robaxin (methocarbamol) is used to treat skeletal muscle conditions such as pain or injury ...
Zanaflex
Zanaflex (tizanidine) is a short-acting muscle relaxer used to treat spasticity by temporarily ...
Soma
Soma (carisoprodol) is used treat injuries and other painful muscle conditions. Includes Soma side ...
Carisoprodol
Carisoprodol is a muscle relaxer that works by blocking pain sensations. Learn about side effects ...
Diazepam
Diazepam is used to treat anxiety disorders, alcohol withdrawal symptoms, or muscle spasms. Learn ...
Baclofen
Baclofen is a muscle relaxant used to treat spasticity and muscle pain in conditions like multiple ...
Tizanidine
Tizanidine is a short-acting muscle relaxant and is used to treat spasticity. Learn about side ...
Frequently asked questions
- What is Ardosons called in the U.S?
- What is Miderizone used for?
- What is the maximum dose of methocarbamol?
More about methocarbamol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (299)
- Drug images
- Latest FDA alerts (8)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: skeletal muscle relaxants
- En español