Norfloxacin Side Effects
Medically reviewed by Drugs.com. Last updated on Mar 24, 2025.
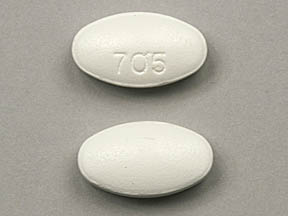
Applies to norfloxacin: oral tablet.
Important warnings
This medicine can cause some serious health issues
You should not use this medication if you have ever had swelling or tearing of a tendon caused by taking norfloxacin or similar antibiotics.
You may not be able to use norfloxacin if you have a muscle disorder. Tell your doctor if you have a history of myasthenia gravis.
Norfloxacin may cause swelling or tearing of a tendon (the fiber that connects bones to muscles in the body), especially in the Achilles' tendon of the heel. This effect may be more likely to occur if you are over 60, if you take steroid medication, or if you have had a kidney, heart, or lung transplant.
Stop taking norfloxacin and call your doctor at once if you have sudden pain, swelling, bruising, tenderness, stiffness, or movement problems in any of your joints. Rest the joint until you receive medical care or instructions.
Get emergency medical help if you have any of these signs of an allergic reaction while taking norfloxacin: hives, or the first sign of a skin rash; fast heartbeat, difficult breathing; swelling of your face, lips, tongue, or throat.
Norfloxacin may cause swelling or tearing of (rupture) a tendon. Norfloxacin can also have serious effects on your nerves, and may cause permanent nerve damage. Stop taking this medicine and call your doctor at once if you have:
-
signs of tendon rupture--sudden pain, swelling, bruising, tenderness, stiffness, movement problems, or a snapping or popping sound in any of your joints (rest the joint until you receive medical care or instructions); or
-
nerve symptoms--numbness, tingling, burning pain, or being more sensitive to temperature, light touch, or the sense of your body position.
Stop using norfloxacin and call your doctor at once if you have:
-
headache with chest pain and severe dizziness, fainting, fast or pounding heartbeats;
-
dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
-
muscle weakness or trouble breathing;
-
diarrhea that is watery or bloody;
-
sudden weakness or ill feeling, fever, chills, sore throat, mouth sores, easy bruising or bleeding;
-
depression, confusion, hallucinations, paranoia, tremors, feeling restless or anxious, unusual thoughts or behavior, insomnia, nightmares;
-
seizure (convulsions); or
-
increased pressure inside the skull-- severe headaches, ringing in your ears, dizziness, nausea, vision problems, pain behind your eyes.
Common side effects may include:
-
nausea, heartburn, stomach cramps, mild diarrhea;
-
vaginal itching or discharge;
-
mild dizziness; or
-
mild headache.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects.
See also:
For healthcare professionals
Applies to norfloxacin: oral tablet.
General adverse events
This drug was generally well tolerated and side effects were mild. Side effects were reported in 6.5% of subjects receiving single doses and 3.6% of subjects receiving multiple doses.[Ref]
Cardiovascular
- Uncommon (0.1% to 1%): Myocardial infarction, palpitation
- Frequency not reported: Tachycardia, ECG QT prolonged, cardiovascular collapse
- Postmarketing reports: Prolonged QTc interval, ventricular arrhythmia (including torsade de pointes)
Quinolones:
- Postmarketing reports: Postural hypotension[Ref]
Dermatologic
- Uncommon (0.1% to 1%): Rash, pruritus, hyperhidrosis, erythema, urticaria
- Rare (0.01% to 0.1%): Petechiae, hemorrhagic bullae/papules with vasculitis, skin reactions, exfoliative dermatitis, toxic epidermal necrolysis (Lyell's syndrome), erythema multiforme, Stevens-Johnson syndrome, photosensitivity, angioedema
- Frequency not reported: Systemic contact dermatitis
- Postmarketing reports: Leukocytoclastic vasculitis, drug rash with eosinophilia and systemic symptoms (DRESS syndrome), photosensitivity/phototoxicity reactions, periorbital erythema
Quinolones:
- Frequency not reported: Erythema nodosum, photosensitivity (phototoxic reactions, photosensitization with vesiculation, redness, swelling, discoloration)[Ref]
Rash, toxic epidermal necrolysis, Stevens-Johnson syndrome, erythema multiforme, pruritus, and exfoliative dermatitis have also been reported during postmarketing experience. Rash has been reported as the most common side effect during postmarketing experience.
A 70-year-old male developed systemic contact dermatitis, an itchy papulopustular eruption from the thighs to the abdomen, after 3 days of therapy with this drug. The patient was treated with prednisone for 15 days. A patch test 1 month later resulted in a reaction to quinolone mix.
Photosensitivity has been reported in patients extensively exposed to sunlight or sunbeds during ongoing therapy with quinolone-like agents.[Ref]
Gastrointestinal
- Common (1% to 10%): Nausea, abdominal cramping
- Uncommon (0.1% to 1%): Abdominal pain, anal/rectal pain, constipation, diarrhea, dry mouth, dyspepsia/heartburn, flatulence, loose stools, vomiting, abdominal swelling, mouth ulcer, pruritus ani
- Rare (0.01% to 0.1%): Pseudomembranous colitis, pancreatitis
- Frequency not reported: Clostridioides difficile-associated diarrhea, antibiotic-associated pseudomembranous colitis
- Postmarketing reports: Stomatitis
Quinolones:
- Frequency not reported: Intestinal perforation[Ref]
The onset of pseudomembranous colitis symptoms has been reported during or after antimicrobial treatment.
Pseudomembranous colitis and pancreatitis have also been reported during postmarketing experience.[Ref]
Genitourinary
- Common (1% to 10%): Increased urine protein
- Uncommon (0.1% to 1%): Dysmenorrhea, renal colic, crystalluria
- Rare (0.01% to 0.1%): Vaginal candidiasis
- Frequency not reported: Glycosuria, vaginal swelling
- Postmarketing reports: Proteinuria
Quinolones:
- Postmarketing reports: Crystalluria, albuminuria, candiduria, cylindruria, hematuria, vaginal candidiasis[Ref]
Crystalluria has occurred in patients taking doses greater than 1200 mg/day and whose urine pH was 7 to 7.8.
Crystalluria and vaginal candidiasis have also been reported during postmarketing experience.[Ref]
Hematologic
- Common (1% to 10%): Eosinophilia, decreased WBC, decreased neutrophil count, decreased platelet count
- Uncommon (0.1% to 1%): Decreased hematocrit, decreased hemoglobin, increased eosinophils, leukopenia, neutropenia, thrombocytopenia, prothrombin time prolongation
- Rare (0.01% to 0.1%): Hemolytic anemia
- Postmarketing reports: Agranulocytosis
Quinolones:
- Postmarketing reports: Agranulocytosis, prothrombin time prolongation[Ref]
Eosinophilia was reported in 7.5% of 1 study population. Leukopenia and neutropenia have been reported in up to 1% of patients. Hemolytic anemia has sometimes been associated with glucose-6-phosphate dehydrogenase deficiency.
Leukopenia, neutropenia, hemolytic anemia, prothrombin time prolongation, and thrombocytopenia have also been reported during postmarketing experience.[Ref]
Hepatic
- Common (1% to 10%): Elevated ALT, elevated AST, cholestatic hepatitis, hepatitis
- Frequency not reported: Eosinophilic necrotizing granulomatous hepatitis
- Postmarketing reports: Jaundice (including cholestatic jaundice), elevated liver function tests, hepatic failure (including fatal cases)
Quinolones:
- Frequency not reported: Hepatic necrosis[Ref]
Hepatitis has also been reported during postmarketing experience.[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Allergies/allergic reactions
- Rare (0.01% to 0.1%): Anaphylactic/anaphylactoid reactions
- Postmarketing reports: Hypersensitivity reactions (including anaphylactoid reactions, anaphylaxis, angioedema, dyspnea, vasculitis, urticaria, arthritis, arthralgia, myalgia, interstitial nephritis, DRESS syndrome)[Ref]
Metabolic
- Uncommon (0.1% to 1%): Anorexia
- Rare (0.01% to 0.1%): Loss of appetite
- Postmarketing reports: Dysglycemia
Quinolones:
- Frequency not reported: Acidosis
- Postmarketing reports: Symptomatic hypoglycemia, elevated blood glucose[Ref]
Musculoskeletal
- Common (1% to 10%): Rhabdomyolysis
- Uncommon (0.1% to 1%): Bursitis, back pain
- Rare (0.01% to 0.1%): Tendinitis, tendosynovitis, myalgia/muscle pains, joint pains, joint inflammation
- Very rare (less than 0.01%): Tendon rupture (e.g., Achilles tendon)
- Frequency not reported: Bilateral arthritis of the ankles
- Postmarketing reports: Elevated creatine kinase, muscle spasms[Ref]
Quinolones, including this drug, have been associated with ruptures of the shoulder, hand, Achilles, and other tendons resulting in disability or requiring surgical repair. Elderly patients and patients concomitantly using corticosteroids may be at increased risk.
Renal transplant patients have an increased risk of Achilles tendinitis and rupture over the general population. Quinolone use has been shown to increase that risk further in this population (12% in quinolone-treated patients versus 7% in patients not treated).
There have been 23 reports of tendinitis submitted to the Australian Adverse Drug Reactions Committee (ADRAC) between 2006 and 2008, including reports of Achilles tendonitis, tendon rupture, and tendon pain and swelling. The reports were primarily in male patients (15 cases) older than 56 years who used ciprofloxacin for 2 to 14 days. In 19 of the reported cases, a fluoroquinolone (generally ciprofloxacin) was the primary suspect; however, details of concomitant serious medical conditions were not documented in most of the reports.
Tendinitis and tendon rupture have also been reported during postmarketing experience.[Ref]
Nervous system
- Common (1% to 10%): Headache, dizziness
- Uncommon (0.1% to 1%): Tingling of the fingers, somnolence/drowsiness, bitter taste
- Rare (less than 0.1%): Peripheral sensory neuropathy/sensory axonal polyneuropathy, peripheral sensory motor neuropathy/sensorimotor axonal polyneuropathy, paresthesia, polyneuropathy, Guillain-Barre syndrome, seizures, tinnitus, exacerbation of myasthenia gravis
- Frequency not reported: Dysesthesia, altered taste
- Postmarketing reports: Generalized seizures, convulsions, myoclonus, tremors, peripheral neuropathy (may be irreversible), ataxia, hypoesthesia, hearing loss, dysgeusia, hypertonia, dysarthria, dysphasia
Quinolones:
- Postmarketing reports: Dysphasia[Ref]
Cases of sensory or sensorimotor axonal polyneuropathy (affecting small and/or large axons) resulting in paresthesias, hypoesthesias, dysesthesias, and weakness have been reported.
Seizures reported in association with this drug have occurred, generally in older patients. A patient with myasthenia gravis had her condition deteriorate during 2 different courses of this drug.
Paresthesia, polyneuropathy (including Guillain-Barre syndrome), tinnitus, and exacerbation of myasthenia gravis have also been reported during postmarketing experience.[Ref]
Ocular
- Uncommon (0.1% to 1%): Blurred vision
- Rare (0.01% to 0.1%): Visual disturbance, increased lacrimation
- Postmarketing reports: Diplopia, uveitis, nystagmus, conjunctivitis, eye pain/irritation, hemophthalmia
Quinolones:
- Postmarketing reports: Nystagmus, visual disturbances[Ref]
Visual disturbances have also been reported during postmarketing experience.[Ref]
Other
- Common (1% to 10%): Asthenia, elevated alkaline phosphatase
- Uncommon (0.1% to 1%): Fever, fatigue, chest pain, foot or hand swelling, chills, edema
- Rare (0.01% to 0.1%): Tiredness
- Frequency not reported: Weakness, elevated LDH
Quinolones:
- Postmarketing reports: Elevated serum triglycerides, elevated serum cholesterol, elevated serum potassium[Ref]
Psychiatric
- Uncommon (0.1% to 1%): Anxiety, depression, insomnia, sleep disturbances
- Rare (0.01% to 0.1%): Mood changes, nervousness, irritability, euphoria, disorientation, hallucinations, confusion, psychic disturbances, psychotic reactions
Quinolones:
- Frequency not reported: Manic reactions[Ref]
Psychic disturbances (including psychotic reactions) and confusion have also been reported during postmarketing experience.[Ref]
Renal
- Rare (0.01% to 0.1%): Interstitial nephritis
- Frequency not reported: Decreased renal function, nephrotic syndrome (which has occurred in patients treated with high doses), increased BUN/serum urea, increased serum creatinine
- Postmarketing reports: Renal failure
Quinolones:
- Frequency not reported: Renal calculi[Ref]
Interstitial nephritis has also been reported during postmarketing experience.[Ref]
Respiratory
Quinolones:
- Frequency not reported: Hiccough[Ref]
References
1. Sabbour MS, El Bokl MA, Osman LM (1984) "Experiences on the efficacy and safety of nalidixic acid, oxolinic acid, cinoxacin and norfloxacin in the treatment of urinary tract infections (UTI)." Infection, 12, p. 377-80
2. (1987) "Norfloxacin (noroxin)." Med Lett Drugs Ther, 29, p. 25-7
3. Walker RC, Wright AJ (1987) "The quinolones." Mayo Clin Proc, 62, p. 1007-12
4. Wolfson JS, Hooper DC (1988) "Norfloxacin: a new targeted fluoroquinolone antimicrobial agent." Ann Intern Med, 108, p. 238-51
5. (2001) "Product Information. Noroxin (norfloxacin)." Merck & Co., Inc
6. Cerner Multum, Inc. "UK Summary of Product Characteristics."
7. Roujeau JC, Kelly JP, Naldi L, et al. (1995) "Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis." N Engl J Med, 333, p. 1600-7
8. Silvestre JF, Alfonso R, Moragon M, Ramon R, Botella R (1998) "Systemic contact dermatitis due to norfloxacin with a positive patch test to quinoline mix." Contact Dermatitis, 39, p. 83
9. Sahin MT, Ozturkcan S, Inanir I, Filiz EE (2005) "Norfloxacin-induced toxic epidermal necrolysis." Ann Pharmacother, 39, p. 768-70
10. Waites KB, Canupp KC, DeVivo MJ (1991) "Efficacy and tolerance of norfloxacin in treatment of complicated urinary tract infection in outpatients with neurogenic bladder secondary to spinal cord injury." Urology, 38, p. 589-96
11. Ehrenpreis ED, Lievens MW, Craig RM (1990) "Clostridium difficile-associated diarrhea after norfloxacin." J Clin Gastroenterol, 12, p. 188-9
12. The Urinary Tract Infection Study Group (1987) "Coordinated mulicenter study of norfloxacin versus trimethoprim-sulfamethoxazole treatment of symptomatic urinary tract infection." J Infect Dis, 155, p. 170-7
13. Anonymous. (1991) "Prevention of bacterial infection in neutropenic patients with hematologic malignancies." Ann Intern Med, 115, p. 7-12
14. Patoia L, Guerciolini R, Menichetti F, Bucaneve G, Del Favero A (1987) "Norfloxacin and neutropenia." Ann Intern Med, 107, p. 788-9
15. Kaplan DS (1990) "Norfloxacin and protime elevation." Am J Gastroenterol, 85, p. 901
16. Mofredj A, Boudjema H, Cadranel JF (2002) "Norfloxacin-induced eosinophilia in a cirrhotic patient." Ann Pharmacother, 36, p. 1107-8
17. Lopez-Navidad A, Domingo P, Cadafalch J, Farrerons J (1990) "Norfloxacin-induced hepatotoxicity." J Hepatol, 11, p. 277-8
18. Davoren P, Mainstone K (1993) "Norfloxacin-induced hepatitis." Med J Aust, 159, 423,
19. Lucena MI, Andrade RJ, SanchezMartinez H, PerezSerrano JM, GomezOutes A (1998) "Norfloxacin-induced cholestatic jaundice." Am J Gastroenterol, 93, p. 2309-11
20. RomeroGomez M, Garcia ES, Fernandez MC (1999) "Norfloxacin-induced acute cholestatic hepatitis in a patient with alcoholic liver cirrhosis." Am J Gastroenterol, 94, p. 2324-5
21. Bjornsson E, Olsson R, Remotti H (2000) "Norfloxacin-induced eosinophilic necrotizing granulomatous hepatitis." Am J Gastroenterol, 95, p. 3662-4
22. Shelley ED, Shelley WB (1988) "The subcorneal pustular drug eruption: an example induced by norfloxacin." Cutis, 42, p. 24-7
23. Alonso MD, Martin JA, Quirce S, Davila I, Lezaun A, Sanchez Cano M (1993) "Fixed eruption caused by ciprofloxacin with cross-sensitivity to norfloxacin." Allergy, 48, p. 296-7
24. Ferguson J, Johnson BE (1993) "Clinical and laboratory studies of the photosensitizing potential of norfloxacin, a 4-quinolone broad-spectrum antibiotic." Br J Dermatol, 128, p. 285-95
25. Jeandel C, Manciaux MA, Bannwarth B, et al. (1989) "Arthritis induced by norfloxacin." J Rheumatol, 16, p. 560-1
26. Donck JB, Segaert MF, Vanrenterghem YF (1994) "Fluoroquinolones and achilles tendinopathy in renal transplant recipients." Transplantation, 58, p. 736-7
27. Terry JB (1995) "Norfloxacin induced arthralgia." J Rheumatol, 22, p. 793-4
28. Guis S, Jouglard J, Kozak-Ribbens G, et al. (2001) "Malignant hyperthermia susceptibility revealed by myalgia and rhabdomyolysis during fluoroquinolone treatment." J Rheumatol, 28, p. 1405-6
29. Khaliq Y, Zhanel GG (2003) "Fluoroquinolone-Associated Tendinopathy: A Critical Review of the Literature." Clin Infect Dis, 36, p. 1404-1410
30. Adverse Drug Reactions Advisory Committee (ADRAC) and the Adverse Drug Reactions Unit of the TGA (2008) Australian Adverse Drug Reactions Bulletin. http://www.tga.gov.au/adr/aadrb/aadr0810.htm
31. Rauser EH, Ariano RE, Anderson BA (1990) "Exacerbation of myasthenia gravis by norfloxacin." DICP, 24, p. 207-8
32. Anastasio GD, Menscer D, Little JM (1988) "Norfloxacin and seizures." Ann Intern Med, 109, p. 169-70
33. Boelaert J, de Jaegere PP, Daneels R, Schurgers M, Gordts B (1986) "Case report of renal failure during norfloxacin therapy." Clin Nephrol, 25, p. 272
34. Hestin D, Hanesse B, Frimat L, Renaudin JM, Netter P, Kessler M (1995) "Norfloxacin-induced nephrotic syndrome." Lancet, 345, p. 732-3
35. Hanson B, Dhondt A, Depierreux M, Lustman F (1996) "Nephrotic syndrome after norfloxacin." Nephron, 74, p. 446
More about norfloxacin
- Check interactions
- Compare alternatives
- Reviews (5)
- Dosage information
- During pregnancy
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
Patient resources
Other brands
Related treatment guides
Further information
Norfloxacin side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.