Xigris: Package Insert / Prescribing Info
Package insert / product label
Generic name: drotrecogin alfa (activated)
Dosage form: injection, powder, lyophilized, for solution
Drug class: Miscellaneous coagulation modifiers
Medically reviewed by Drugs.com. Last updated on Mar 25, 2025.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- References
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
XIGRIS (drotrecogin alfa (activated)) injection, powder, lyophilized, for solution for intravenous use
Initial U.S. Approval: 2001
Recent Major Changes
Indications and Usage for Xigris
Xigris Dosage and Administration
- Infuse intravenously at 24 mcg/kg/hr (based on actual body weight) for a total duration of 96 hours. (2)
Dosage Forms and Strengths
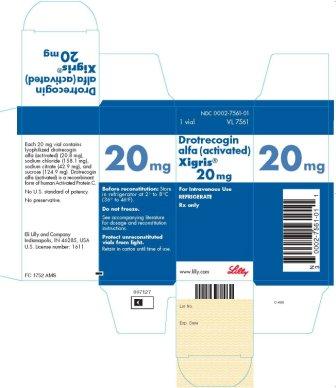
Single-use vials of 5 mg and 20 mg Xigris as a sterile, preservative-free, lyophilized powder for reconstitution. (3)
Contraindications
Xigris is contraindicated in clinical situations where bleeding could lead to significant morbidity or death. (4)
Warnings and Precautions
- Bleeding: Weigh the increased risk of bleeding against benefits of Xigris for patients with certain conditions. Stop Xigris infusion if clinically important bleeding occurs. (5.1)
- Mortality in patients with single organ dysfunction and recent surgery: These patients may not be at a high risk of death and may not be among the indicated population. (5.2)
- Use in patients on prophylactic heparin: Consider continuing heparin prophylaxis when initiating Xigris, unless discontinuation is medically necessary. (5.3)
- Invasive procedures: Minimize invasive procedures during Xigris infusion. Discontinue Xigris 2 hours prior to major invasive procedures. (5.4)
Adverse Reactions/Side Effects
Bleeding is the most commonly reported adverse reaction. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Eli Lilly and Company at 1-800-LillyRx (1-800-545-5979) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
Drug Interactions
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 11/2009
Full Prescribing Information
1. Indications and Usage for Xigris
Xigris® is indicated for the reduction of mortality in adult patients with severe sepsis (sepsis associated with acute organ dysfunction) who have a high risk of death (e.g., as determined by APACHE II score ≥25) [see Clinical Studies (14.1)].
2. Xigris Dosage and Administration
2.1 Recommended Dosing and Administration Overview
Xigris should be administered intravenously at an infusion rate of 24 mcg/kg/hr (based on actual body weight) for a total duration of infusion of 96 hours. Dose adjustment based on clinical or laboratory measurements is not recommended [see Drug Interactions (7.3)]. Dose escalation or bolus doses of Xigris are not recommended.
If the infusion is interrupted, Xigris should be restarted at the 24 mcg/kg/hr infusion rate.
In the event of clinically important bleeding, immediately stop the infusion [see Warnings and Precautions (5.1)].
Xigris should be administered via a dedicated intravenous line or a dedicated lumen of a multilumen venous catheter. The ONLY other solutions that can be administered through the same line are 0.9% Sodium Chloride Injection, USP; Lactated Ringer's Injection, USP; Dextrose Injection, USP; and Dextrose and Sodium Chloride Injection, USP.
Avoid exposing Xigris solutions to heat and/or direct sunlight. Studies conducted at the recommended concentrations indicate the Xigris intravenous solution to be compatible with glass infusion bottles, and infusion bags and syringes made of polyvinylchloride, polyethylene, polypropylene, or polyolefin.
2.2 Preparation of the Concentrated Solution
Note: Reconstitute vials of lyophilized Xigris only with Sterile Water for Injection, USP.
- Use appropriate aseptic technique during the preparation of Xigris for intravenous administration.
- Calculate the approximate amount of Xigris needed based upon the patient's actual body weight and duration of infusion period. The maximum duration of infusion from one infusion bag or syringe is 12 hours. Multiple infusion periods will be needed to cover the entire 96-hour duration of administration.
-
mg of Xigris = (patient weight, kg) x (24 mcg/kg/hr) x (hours of infusion) ÷ (1000)
- Determine the number of vials of Xigris needed to make up this amount.
- Reconstitute each vial of Xigris only with Sterile Water for Injection, USP. The 5 mg vials must be reconstituted with 2.5 mL. The 20 mg vials must be reconstituted with 10 mL. Slowly add the Sterile Water for Injection, USP to the vial and avoid inverting or shaking the vial. Gently swirl each vial until the powder is completely dissolved. The resulting Xigris concentration of the solution is 2 mg/mL.
- Xigris contains no antibacterial preservatives; the intravenous solution should be prepared immediately after reconstitution of the Xigris in the vial(s). If the vial of reconstituted Xigris is not used immediately, it may be held at controlled room temperature 20° to 25°C (68° to 77°F), but must be used within 3 hours.
- Inspect the reconstituted Xigris in the vials for particulate matter and discoloration before further dilution. Do not use vials if particulate matter is visible or the solution is discolored.
2.3 Dilution and Administration Instructions for an Intravenous Infusion Pump Using an Infusion Bag
Complete “Preparation of Concentrated Solution” steps 1-6 above, then complete the next 7 steps [see Dosage and Administration (2.2)].
- The solution of reconstituted Xigris must be further diluted into an infusion bag containing 0.9% Sodium Chloride Injection, USP to a final concentration of between 0.1 mg/mL and 0.2 mg/mL. Bag volumes between 50 mL and 250 mL are typical.
- Confirm that the intended bag volume will result in an acceptable final concentration.
-
Final concentration, mg/mL = (actual Xigris amount, mg) ÷ (bag volume, mL)
- Slowly withdraw the reconstituted Xigris solution from the vial(s) and add the reconstituted Xigris into the infusion bag of 0.9% Sodium Chloride Injection, USP. When injecting the Xigris into the infusion bag, direct the stream to the side of the bag to minimize the agitation of the solution. Gently invert the infusion bag to obtain a homogeneous solution. Do not transport the infusion bag using mechanical transport systems such as pneumatic-tube systems that may cause vigorous agitation of the solution.
- Calculate the actual duration of the infusion period for the diluted Xigris.
-
Infusion period, hours = (actual Xigris amount, mg) x (1000) ÷ (patient weight, kg) ÷ (24 mcg/kg/hr)
- Account for the added volume of reconstituted Xigris (0.5 mL per mg of Xigris used) and the volume of bag saline solution removed (if saline solution is removed prior to adding the reconstituted Xigris).
-
Final bag volume, mL = (starting bag volume, mL) + (reconstituted Xigris volume, mL) - [saline volume removed (if any), mL]
- Calculate the actual infusion rate of the diluted Xigris.
-
Infusion rate, mL/hr = (final bag volume, mL) ÷ (infusion period, hours)
- After preparation in an infusion bag, the intravenous solution should be used at controlled room temperature 20° to 25°C (68° to 77°F) within 12 hours. If the intravenous solution is not administered immediately, the solution should be refrigerated at 2° to 8°C (36° to 46°F) for up to 12 hours. If the prepared solution is refrigerated prior to administration, the maximum time limit for use of the intravenous solution, including dilution, refrigeration, and administration, is 24 hours.
2.4 Dilution and Administration Instructions for a Syringe Pump
Complete “Preparation of Concentrated Solution” steps 1-6 above, then complete the next 7 steps [see Dosage and Administration (2.2)].
- The solution of reconstituted Xigris must be further diluted with 0.9% Sodium Chloride Injection, USP to a final concentration of between 0.1 mg/mL and 0.2 mg/mL.
-
Confirm that the intended solution volume will result in an acceptable final concentration.
-
Final concentration, mg/mL = (actual Xigris amount, mg) ÷ (solution volume, mL)
- Slowly withdraw the reconstituted Xigris solution from the vial(s) into a syringe that will be used in the syringe pump. Into the same syringe, slowly withdraw 0.9% Sodium Chloride Injection, USP to obtain the desired final volume of diluted Xigris. Gently invert and/or rotate the syringe to obtain a homogeneous solution.
- Calculate the actual duration of the infusion period for the diluted Xigris.
-
Infusion period, hours = (actual Xigris amount, mg) x (1000) ÷ (patient weight, kg) ÷ (24 mcg/kg/hr)
- Calculate the actual infusion rate of the diluted Xigris.
-
Infusion rate, mL/hr = (solution volume, mL) ÷ (infusion period, hours)
- When administering Xigris using a syringe pump at low flow rates (less than approximately 5 mL/hr), the infusion set must be primed for approximately 15 minutes at a flow rate of approximately 5 mL/hr.
- After preparation in a syringe, the intravenous solution should be used at controlled room temperature 20° to 25°C (68° to 77°F) within 12 hours. If the intravenous solution is not administered immediately, the solution should be refrigerated at 2° to 8°C (36° to 46°F) for up to 12 hours. If the prepared solution is refrigerated prior to administration, the maximum time limit for use of the intravenous solution, including dilution, refrigeration, and administration, is 24 hours.
3. Dosage Forms and Strengths
Xigris is supplied in single-use vials of 5 mg and 20 mg drotrecogin alfa (activated) as a sterile, preservative-free, lyophilized white to off-white powder for reconstitution.
4. Contraindications
Xigris increases the risk of bleeding. Xigris is contraindicated in the following clinical situations where bleeding could lead to significant morbidity or death:
- Active internal bleeding
- Recent (within 3 months) hemorrhagic stroke
- Recent (within 2 months) intracranial or intraspinal surgery, or severe head trauma
- Trauma with an increased risk of life-threatening bleeding
- Presence of an epidural catheter
- Intracranial neoplasm or mass lesion or evidence of cerebral herniation
5. Warnings and Precautions
5.1 Bleeding
Bleeding is the most common serious adverse reaction experienced by patients receiving Xigris. Each patient being considered for therapy with Xigris should be carefully evaluated and anticipated benefits weighed against potential risks associated with therapy.
Certain conditions, many of which led to exclusion from Study 1 [see Clinical Studies (14.1)], are likely to increase the risk of bleeding with Xigris therapy. For individuals with one or more of the following conditions, the increased risk of bleeding should be carefully considered when deciding whether to use Xigris therapy:
- Concurrent therapeutic dosing of heparin to treat an active thrombotic or embolic event [see Drug Interactions (7.1)]
- Platelet count <30,000 x 106/L, even if the platelet count is increased after transfusions
- Prothrombin time-INR >3.0
- Recent (within 6 weeks) gastrointestinal bleeding
- Recent administration (within 3 days) of thrombolytic therapy
- Recent administration (within 7 days) of oral anticoagulants or glycoprotein IIb/IIIa inhibitors
- Recent administration (within 7 days) of aspirin >650 mg per day or other platelet inhibitors
- Recent (within 3 months) ischemic stroke [see Contraindications (4)]
- Intracranial arteriovenous malformation or aneurysm
- Known bleeding diathesis
- Chronic severe hepatic disease
- Any other condition in which bleeding constitutes a significant hazard or would be particularly difficult to manage because of its location
Should clinically important bleeding occur, immediately stop the infusion of Xigris. Continued use of other agents affecting the coagulation system should be carefully assessed. Once adequate hemostasis has been achieved, continued use of Xigris may be reconsidered.
5.2 Mortality in Patients with Single Organ Dysfunction and Recent Surgery
In Study 1, among the small number of patients with single organ dysfunction and recent surgery (surgery within 30 days prior to study treatment), all-cause mortality was numerically higher in the Xigris group (28-day: 10/49; in-hospital: 14/48) compared with the placebo group (28-day: 8/49; in-hospital: 8/47).
In an analysis of the subset of patients with single organ dysfunction and recent surgery from Study 2, which enrolled septic patients not at high risk of death, all-cause mortality was also higher in the Xigris group (28-day: 67/323; in-hospital: 76/325) compared with the placebo group (28-day: 44/313; in-hospital: 62/314). Single organ dysfunction patients with recent surgery may not be at high risk of death irrespective of APACHE II score. Therefore, these patients may not be among the indicated population.
5.3 Patients on Prophylactic Heparin when Xigris is Initiated
Clinicians should consider continuing heparin for venous thromboembolism (VTE) prophylaxis when initiating Xigris, unless discontinuation is medically necessary. In a randomized study of prophylactic heparin versus placebo in 1935 adult severe sepsis patients treated with Xigris, mortality and the rate of serious adverse events were increased in the subgroup of 434 patients whose heparin was stopped on study entry by randomization to placebo-plus-Xigris. This finding was based on prospectively defined exploratory subgroup analyses; however, the explanation for the finding is unclear. The safety of prophylactic heparin when concomitantly administered with Xigris in adult patients with severe sepsis was evaluated with low molecular weight heparin enoxaparin (40 mg every 24 hours) and unfractionated sodium heparin (5000 U every12 hours), but was not evaluated with unfractionated sodium heparin 5000 U when dosed every 8 hours [see Clinical Studies (14.5)].
5.4 Invasive Procedures
Invasive procedures increase the risk for bleeding with Xigris. Such procedures, including arterial and central venous punctures, should be minimized during the Xigris infusion. Puncture of a noncompressible site should be avoided during the infusion. Xigris should be discontinued 2 hours prior to undergoing an invasive surgical procedure or procedures with an inherent risk of bleeding. Once adequate hemostasis has been achieved, Xigris may be restarted 12 hours after surgery and major invasive procedures or immediately after uncomplicated less invasive procedures.
5.5 Laboratory Tests for Coagulopathy
Most patients with severe sepsis have a coagulopathy that is commonly associated with prolongation of the activated partial thromboplastin time (APTT) and the prothrombin time (PT). The activated partial thromboplastin time (APTT) cannot be reliably used to assess the degree of the coagulopathy during Xigris infusion since Xigris variably prolongs the APTT [see Drug Interactions (7.3)].
The prothrombin time (PT) may be used to monitor the degree of the coagulopathy in patients treated with Xigris because Xigris has minimal effect on the PT [see Drug Interactions (7.3)].
Drotrecogin alfa (activated) present in plasma samples may interfere with one-stage coagulation assays based on the APTT (such as factor VIII, IX, and XI assays). This interference will result in a measured factor concentration that is lower than the actual concentration. Drotrecogin alfa (activated) present in plasma samples does not interfere with one-stage factor assays based on the PT (such as factor II, V, VII, and X assays) [see Drug Interactions (7.3)].
6. Adverse Reactions/Side Effects
Bleeding is the most commonly reported adverse reaction in patients receiving Xigris therapy [see Contraindications (4) and Warnings and Precautions (5.1)]. Patients administered Xigris as treatment for severe sepsis experience many events which are potential sequelae of severe sepsis and may or may not be attributable to Xigris therapy. In severe sepsis clinical trials, there were no types of non-bleeding adverse events suggesting a causal association with Xigris.
6.1 Clinical Trial Experience
The data below describe the population of 8639 adult severe sepsis patients exposed to study drug (6506 Xigris and 2133 placebo) in 2 placebo-controlled and 2 open-label studies of Xigris. The population was 18-99 years of age, of whom 42% were female and 58% were male. The ethnic/racial origin of these patients was the following: Caucasian 79.5%, African descent 5.8%, Hispanic 5.3%, East/Southeast Asian 3.4%, and Other origin 6.0%. These studies used the standard dose regimen of 24 mcg/kg/hr for 96 hours total duration of infusion.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In Study 1 [see Clinical Studies (14.1)], serious bleeding events were observed during the 28-day study period in 3.5% of Xigris-treated and 2.0% of placebo-treated patients, respectively. The difference in serious bleeding between Xigris and placebo occurred primarily during the infusion period and is shown in Table 1. Serious bleeding events included any intracranial hemorrhage, any life-threatening or fatal bleed, any bleeding event requiring the administration of ≥3 units of packed red blood cells per day for 2 consecutive days or any bleeding event assessed as a serious adverse event.
|
a Study drug infusion period is defined as the date of initiation of study drug to the date of study drug discontinuation plus the next calendar day. |
||
|
b Patients requiring the administration of ≥3 units of packed red blood cells per day for 2 consecutive days without an identified site of bleeding. |
||
| Xigris
N=850 | Placebo
N=840 |
|
| Total | 20 (2.4%) | 8 (1.0%) |
| Site of Hemorrhage | ||
| Gastrointestinal | 5 | 4 |
| Intra-abdominal | 2 | 3 |
| Intra-thoracic | 4 | 0 |
| Retroperitoneal | 3 | 0 |
| Intracranial | 2 | 0 |
| Genitourinary | 2 | 0 |
| Skin/soft tissue | 1 | 0 |
| Otherb | 1 | 1 |
In Study 1, two cases of intracranial hemorrhage (ICH) occurred during the infusion period for Xigris-treated patients and no cases were reported in the placebo patients. The incidence of ICH during the 28-day study period was 0.2% for Xigris-treated patients and 0.1% for placebo-treated patients. ICH has been reported in patients receiving Xigris in non-placebo controlled trials with an incidence of approximately 1% during the infusion period. The risk of ICH may be increased in patients with risk factors for bleeding such as severe coagulopathy and severe thrombocytopenia [see Warnings and Precautions (5.1)].
In Study 1, 25% of the Xigris-treated patients and 18% of the placebo-treated patients experienced at least one bleeding event during the 28-day study period. In both treatment groups, the majority of bleeding events were ecchymoses or gastrointestinal tract bleeding.
Additional information on adverse events has been obtained in the controlled study of patients not at a high risk of death (Study 2) [see Clinical Studies (14.3)] and an open label, uncontrolled study of 2378 adult patients with severe sepsis that enrolled both patients at high risk of death and not at high risk of death. The incidence rates and nature of treatment-associated adverse events in Study 2 were generally similar to that seen on Study 1. In the open label, uncontrolled study, serious bleeding occurred in 3.6% of patients during the infusion period, and 6.5% during the 28 day study period. Intracranial hemorrhage occurred among 0.6% of patients during the infusion period and 1.5% within 28 days. Most of the post-infusion ICH events occurred within 1 week of the Xigris infusion; the relationship of these events to Xigris is uncertain.
In Study 4 [see Clinical Studies (14.5)], a randomized trial of prophylactic heparin versus placebo in Xigris-treated severe sepsis patients, rates of serious bleeding, including ICH, were consistent with rates observed in previous studies. Prophylactic heparin did not increase the risk of serious bleeding, including ICH, in patients receiving Xigris. Non-serious bleeding was increased in patients receiving prophylactic heparin compared with placebo over the treatment period of 0-6 days (see Table 2).
|
a Serious bleeding events included any fatal bleed, any life-threatening bleed, any CNS bleed, or any bleeding event assessed as serious by the investigator. |
||
|
b ICH includes any bleed in the central nervous system, including the following types of hemorrhage — petechial, parenchymal, subarachnoid, subdural, and stroke with hemorrhagic transformation. |
||
| Heparin-plus-Xigris
N=976 | Placebo-plus-Xigris
N=959 |
|
| Serious Bleeding Eventsa(%) | ||
| Days 0-6 | 22 (2.3%) | 24 (2.5%) |
| Days 0-28 | 38 (3.9%) | 50 (5.2%) |
| ICHb(%) | ||
| Days 0-6 | 3 (0.3%) | 3 (0.3%) |
| Days 0-28 | 10 (1.0%) | 7 (0.7%) |
| Overall Bleeding (Serious and Non-serious) Events (%) | ||
| Days 0-6 | 105 (10.8%) | 78 (8.1%) |
| Days 0-28 | 121 (12.4%) | 105 (10.9%) |
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity.
In severe sepsis clinical studies (Study 1, 2, 4 and the open-label, uncontrolled study), serum samples were collected from 1493 adult patients who received placebo or no study drug and 1855 adult patients who received Xigris for evaluation of anti-human activated protein C IgA/IgG/IgM antibodies with an enzyme-linked immunosorbent assay (ELISA). Plasma samples from patients positive in this detection assay were also tested for their ability to neutralize Xigris activity in an in vitro assay.
In the 4 clinical studies, 1.6% (24/1493) placebo- and 1.5% (27/1855) Xigris-treated patients had negative baseline and positive post-baseline anti-human activated protein C antibodies. Three of the 24 placebo- and 5 of the 27 Xigris-treated patients tested positive for neutralizing IgG antibodies in the in vitro APTT assay. Positive rates were comparable for both anti-human activated protein C and neutralizing antibody between Xigris- and placebo-treated patients by sampling time. No apparent correlation of antibody development to adverse reactions was observed among this limited number of patients. There was no evidence anti-human activated protein C antibodies detected represented a specific immune response to Xigris therapy.
Immunogenicity data are highly dependent on the sensitivity and specificity of the assay. The observed incidence of antibody positivity in an assay may be influenced by several factors including assay design, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to Xigris with the incidence of antibodies to other products may be misleading.
Re-administration— There have been no company-sponsored clinical trials in severe sepsis specifically studying Xigris re-administration. Neither safety nor efficacy has been demonstrated in this use. In Study 2 and Study 4, no hypersensitivity reactions were reported in 10 patients who received a second course of Xigris. Samples available from six adult severe sepsis patients (Study 2) who had received a prior course of Xigris were subsequently tested and all were negative for anti-human activated protein C antibody.
Related/similar drugs
7. Drug Interactions
7.1 Coadministration of Drugs that Affect Hemostasis
Since there is an increased risk of bleeding with Xigris, caution should be employed when Xigris is used with other drugs that affect hemostasis [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
7.2 Coadministration of Prophylactic Heparin
Heparin for venous thromboembolism (VTE) prophylaxis may be coadministered with Xigris [see Warnings and Precautions (5.3) and Clinical Studies (14.5)]. No dosage adjustment of Xigris is recommended when coadministered with prophylactic heparin [see Clinical Pharmacology (12.3)].
7.3 Interference with Coagulation Assays
Xigris has minimal effect on the prothrombin time (PT). Prolongation of the activated partial thromboplastin time (APTT) in patients with severe sepsis receiving Xigris may be due to the underlying coagulopathy, the pharmacodynamic effect of Xigris, and/or the pharmacodynamic effect of other concurrent medications. The effect of Xigris on the APTT assay is dependent on the reagent and instrument used to perform the assay and the time that elapses between sample acquisition and assay performance. Drotrecogin alfa (activated) present in a plasma sample will be gradually neutralized by endogenous inhibitors. Due to these biological and analytical variables, the APTT should not be used to assess the pharmacodynamic effect of Xigris. The interpretation of sequential determination of the PT and/or APTT should take these variables into consideration.
Because Xigris may affect the APTT assay, drotrecogin alfa (activated) present in plasma samples may interfere with one-stage coagulation assays based on the APTT (such as factor VIII, IX, and XI assays). This interference may result in a measured factor concentration that is lower than the actual concentration. Drotrecogin alfa (activated) present in plasma samples does not interfere with one-stage factor assays based on the PT (such as factor II, V, VII, and X assays).
8. Use In Specific Populations
8.1 Pregnancy
Pregnancy Category C— Animal reproduction studies have not been conducted with Xigris. It is also not known whether Xigris can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. In published case reports, there were no major malformations or other adverse outcomes reported following treatment with Xigris during pregnancy. Due to the limited number of exposed pregnancies, these postmarketing data do not reliably estimate the frequency or absence of adverse outcomes. Xigris should be given to a pregnant woman only if clearly needed.
8.3 Nursing Mothers
It is not known whether drotrecogin alfa (activated) is excreted in human milk or absorbed systemically after ingestion. Because many drugs are excreted in human milk, and because of the potential for serious adverse reactions in nursing infants from Xigris, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
A placebo-controlled trial in pediatric patients (Study 3) did not establish safety and effectiveness of Xigris in the pediatric patient population [see Indications and Usage (1) and Clinical Studies (14.4)].
8.5 Geriatric Use
In Study 1, which evaluated 1690 patients with severe sepsis, 48 percent were 65 years and over, while 23 percent were 75 and over. No overall difference in safety was observed between these patients and younger patients. Reduction in mortality was observed in both geriatric and younger patients.
10. Overdosage
There is no known antidote for Xigris. In case of overdose, immediately stop the infusion and monitor closely for hemorrhagic complications [see Clinical Pharmacology (12.3)].
In postmarketing experience there have been a limited number of medication error reports of excessive rate of Xigris infusion for short periods of time (median 2 hours). No unexpected adverse events were observed during the overdose period. However, this information is insufficient to assess whether Xigris overdose is associated with an increased hemorrhage risk beyond that observed with Xigris administered at the recommended dose.
11. Xigris Description
Xigris (drotrecogin alfa (activated)) is a recombinant form of human activated protein C. An established human cell line possessing the complementary DNA for the inactive human protein C zymogen secretes the protein into the fermentation medium. Fermentation is carried out in a nutrient medium containing the antibiotic geneticin sulfate. Geneticin sulfate is not detectable in the final product. Human protein C is enzymatically activated by cleavage with thrombin and subsequently purified.
Drotrecogin alfa (activated) is a serine protease with the same amino acid sequence as human plasma-derived activated protein C. Drotrecogin alfa (activated) is a glycoprotein of approximately 55 kilodalton molecular weight, consisting of a heavy chain and a light chain linked by a disulfide bond. Drotrecogin alfa (activated) and human plasma-derived activated protein C have the same sites of glycosylation, although some differences in the glycosylation structures exist.
Xigris is supplied as a sterile, lyophilized, white to off-white powder for intravenous infusion. The 5 and 20 mg vials of Xigris contain 5.3 mg and 20.8 mg of drotrecogin alfa (activated), respectively. The 5 and 20 mg vials of Xigris also contain 40.3 and 158.1 mg of sodium chloride, 10.9 and 42.9 mg of sodium citrate, and 31.8 and 124.9 mg of sucrose, respectively.
12. Xigris - Clinical Pharmacology
12.1 Mechanism of Action
Activated protein C exerts an antithrombotic effect by inhibiting Factors Va and VIIIa. In vitro data indicate that activated protein C may have indirect profibrinolytic activity through its ability to inhibit plasminogen activator inhibitor-1 (PAI-1) and may exert an anti-inflammatory effect by limiting the chemotactic response of leukocytes to inflammatory cytokines, an inhibitory process mediated by leukocyte cell surface activated protein C receptor. In addition, in vivo data suggest activated protein C may reduce interactions between leukocytes and the microvascular endothelium. In vitro bacterial phagocytosis by neutrophils and monocytes is not affected.
12.2 Pharmacodynamics
The specific pharmacologic effects by which Xigris exerts its effect on survival in patients with severe sepsis are not completely understood. In patients with severe sepsis, Xigris infusions of 48 or 96 hours produced dose-dependent declines in D-dimer and IL-6. Compared with placebo, Xigris-treated patients experienced more rapid declines in D-dimer, PAI-1 levels, thrombin-antithrombin levels, prothrombin F1.2, IL-6, more rapid increases in protein C and antithrombin levels, and normalization of plasminogen. As assessed by infusion duration, the maximum observed pharmacodynamic effect of drotrecogin alfa (activated) on D-dimer levels occurred at the end of 96 hours of infusion for the 24 mcg/kg/hr treatment group.
12.3 Pharmacokinetics
Drotrecogin alfa (activated) and endogenous activated protein C are inactivated by endogenous plasma protease inhibitors. Plasma concentrations of endogenous activated protein C in healthy subjects and patients with severe sepsis are usually below detection limits.
In patients with severe sepsis, Xigris infusions of 12 mcg/kg/hr to 30 mcg/kg/hr produce steady-state concentrations (Css) that are proportional to infusion rates. In Study 1 [see Clinical Studies (14.1)], the median clearance of drotrecogin alfa (activated) was 40 L/hr (interquartile range of 27 to 52 L/hr) in adults with severe sepsis. The median Css of 45 ng/mL (interquartile range of 35 to 62 ng/mL) was attained within 2 hours after starting the infusion. In the majority of patients, plasma concentrations of drotrecogin alfa (activated) fell below the assay's quantitation limit of 10 ng/mL within 2 hours after stopping the infusion. Plasma clearance of drotrecogin alfa (activated) in patients with severe sepsis is approximately 50% higher than that in healthy subjects.
Patients with Renal Impairment— Patients with end stage renal disease requiring chronic renal replacement therapy were excluded from Study 1 [see Clinical Studies (14.1)]. In patients without sepsis undergoing hemodialysis (n=6), plasma clearance (mean ± SD) of drotrecogin alfa (activated) administered on non-dialysis days was 30 ± 8 L/hr. Plasma clearance of drotrecogin alfa (activated) was 23 ± 4 L/hr in patients without sepsis undergoing peritoneal dialysis (n=5). These clearance rates did not meaningfully differ from those in normal healthy subjects (28 ± 9 L/hr) (n=190). No dosage adjustment is necessary for patients with renal impairment requiring hemodialysis or peritoneal dialysis.
Other Subpopulations— In adult patients with severe sepsis, small differences were detected in the plasma clearance of drotrecogin alfa (activated) with regard to age, gender, hepatic impairment, and obesity. No dose adjustment is required based on these factors alone or in combination.
Prophylactic Heparin— In a randomized, double-blind, placebo-controlled trial in adult patients with severe sepsis (Study 4), coadministration of Xigris (24 mcg/kg/hr for 96 hours) and prophylactic heparin (enoxaparin 40 mg every 24 hours or unfractionated sodium heparin 5000 U every 12 hours administered subcutaneously) did not alter the clearance and steady-state concentrations of drotrecogin alfa (activated). No dosage adjustment of Xigris is recommended when coadministered with prophylactic heparin [see Clinical Studies (14.5)].
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies in animals to evaluate potential carcinogenicity of Xigris have not been performed.
Xigris was not mutagenic in an in vivo micronucleus study in mice or in an in vitro chromosomal aberration study in human peripheral blood lymphocytes with or without rat liver metabolic activation.
The potential of Xigris to impair fertility has not been evaluated in male or female animals.
14. Clinical Studies
14.1 Study 1: Treatment of Adult Severe Sepsis Patients
The efficacy of Xigris was studied in an international, multi-center, randomized, double-blind, placebo-controlled trial (“PROWESS”) of 1690 patients with severe sepsis. Entry criteria included a systemic inflammatory response presumed due to infection and at least one associated acute organ dysfunction. Acute organ dysfunction was defined as one of the following: cardiovascular dysfunction (shock, hypotension, or the need for vasopressor support despite adequate fluid resuscitation); respiratory dysfunction (relative hypoxemia [PaO2/FiO2 ratio <250]); renal dysfunction (oliguria despite adequate fluid resuscitation); thrombocytopenia (platelet count <80,000/mm3 or 50% decrease from the highest value the previous 3 days); or metabolic acidosis with elevated lactic acid concentrations. Patients received a 96-hour infusion of Xigris at 24 mcg/kg/hr or placebo starting within 48 hours after the onset of the first sepsis-induced organ dysfunction. The median duration of organ dysfunction prior to treatment was 18 hours, and 89% of patients received study drug within 24 hours after onset of the first organ dysfunction. Exclusion criteria encompassed patients at high risk for bleeding [see Contraindications (4) and Warnings and Precautions (5.1)], patients who were not expected to survive for 28 days due to a preexisting, non-sepsis related medical condition, HIV-positive patients whose most recent CD4 count was ≤50/mm3, patients on chronic dialysis, and patients who had undergone bone marrow, lung, liver, pancreas, or small bowel transplantation.
All-cause mortality was assessed 28 days after the start of study drug administration. Prospectively defined subsets for mortality analyses included groups defined by APACHE II score [see References (15)] (a score designed to assess risk of mortality based on acute physiology and chronic health evaluation), protein C activity, and the number of acute organ dysfunctions at baseline. The APACHE II score was calculated from physiologic and laboratory data obtained within the 24-hour period immediately preceding the start of study drug administration irrespective of the preceding length of stay in the intensive care unit.
The study was terminated after a planned interim analysis due to significantly lower mortality in patients on Xigris than in patients on placebo. At 28 days, the overall mortality rates were 25% for the Xigris-treated group and 31% for the placebo-treated group (p=0.005) (see Table 3).
Baseline APACHE II score was correlated with risk of death; among patients receiving placebo, those with the lowest APACHE II scores had a 12% mortality rate, while those in the 2nd, 3rd, and 4th APACHE quartiles had mortality rates of 26%, 36%, and 49%, respectively. The observed mortality difference between Xigris and placebo was limited to the half of patients with higher risk of death, i.e., APACHE II score ≥25, the 3rd and 4th quartile APACHE II scores, where the 28-day mortality rates were 31% for the Xigris-treated group and 44% for the placebo-treated group (p=0.0002) (see Table 3). The efficacy of Xigris has not been established in patients with lower risk of death, e.g., APACHE II score <25.
|
a Total N=Total number of patients in group. |
|||||||
| Xigris | Placebo | Absolute Mortality Difference (%) | Relative Risk (RR) | 95% CI for RR | |||
| Total Na | Deaths | Total Na | Deaths | ||||
| Overall | 850 | 210 (25%) | 840 | 259 (31%) | -6 | 0.81 | 0.70, 0.93 |
| APACHE II quartile (score) | |||||||
| 1st + 2nd (3-24) | 436 | 82 (19%) | 437 | 83 (19%) | 0 | 0.99 | 0.75, 1.30 |
| 3rd + 4th (25-53) | 414 | 128 (31%) | 403 | 176 (44%) | -13 | 0.71 | 0.59, 0.85 |
Of measures used, the APACHE II score was most effective in classifying patients by risk of death within 28 days and by likelihood of benefit from Xigris, but other important indicators of risk or severity also supported an association between likelihood of Xigris benefit and risk of death. For patients with 1, 2, 3, and 4 or more organ dysfunctions, absolute reductions in mortality of 2%, 5%, 8%, and 11% with Xigris were observed (relative risk of 0.92, 0.80, 0.76, and 0.78, respectively).
Similarly, each of the three major components of the APACHE II score (acute physiology score, chronic health score, age score) identified a higher risk population with larger mortality differences associated with treatment. That is, the reduction in mortality was greater in patients with more severe physiologic disturbances, in patients with serious underlying disease predating sepsis, and in older patients.
Treatment-associated reductions in mortality were observed in patients with normal protein C levels and those with low protein C levels. No substantial differences in Xigris treatment effects were observed in subgroups defined by gender, ethnic origin, or infectious agent.
14.2 Long-Term Follow-up of Patients in Study 1
The one-year survival status was provided for 93% of the 1690 Study 1 subjects. For patients with APACHE II score ≥25, mortality was lower for the Xigris group compared with the placebo group through 90 days (41% versus 52%; RR: 0.72, 95% CI: 0.59-0.88) and through 1 year (48% versus 59%; RR: 0.73, 95% CI: 0.60-0.88).
However, for patients with APACHE II score <25, mortality was higher for the Xigris group compared with the placebo group through 90 days (27% versus 25%; RR: 1.09, 95% CI: 0.84-1.42) and through 1 year (35% versus 28%; RR: 1.24, 95% CI: 0.97-1.58).
14.3 Study 2: Benefit Not Demonstrated in Treatment of Adult Severe Sepsis Patients Not at High Risk of Death
A randomized, double-blind, placebo-controlled trial (“ADDRESS”) of Xigris (96-hour infusion of Xigris at 24 mcg/kg/hr) was performed in adult patients with severe sepsis who were not at high risk of death. Most patients had APACHE II score <25 or only one sepsis-induced organ failure. The study was stopped at an interim analysis after enrollment of 2640 patients due to no observed benefit. All-cause mortality at 28 days after randomization was 18% (243/1333) in patients randomized to Xigris and 17% (221/1307) in patients randomized to placebo (RR: 1.08, 95% CI: 0.91-1.27).
The results of Studies 1 and 2 do not provide evidence of benefit of Xigris in patients with severe sepsis who are not at high risk of death (e.g., patients with single-organ dysfunction or APACHE II score <25). Xigris is not indicated for such patients.
14.4 Study 3: Benefit Not Demonstrated in Treatment of Pediatric Severe Sepsis Patients
A randomized, double-blind, placebo-controlled trial (“RESOLVE”) of Xigris (96-hour infusion at 24 mcg/kg/hr) was conducted in 477 pediatric patients with severe sepsis (age limits ≥38 weeks corrected gestational age to <18 years). Patients were required to have both sepsis-induced cardiovascular and respiratory organ dysfunction (defined as treatment with vasoactive agents despite adequate fluid resuscitation and invasive mechanical ventilation).
The study was stopped after a planned interim analysis showed Xigris was unlikely to show statistically significant improvement over placebo, a composite endpoint based on time to resolution of organ dysfunction (cardiovascular, respiratory, and renal), incorporating also unresolved organ dysfunction and mortality.
Central nervous system bleeding occurred in a greater number of Xigris-treated patients during the 28-day study period; this difference was most pronounced in patients aged 60 days or younger (≤60 days: 4/24 Xigris-treated patients versus 0/26 placebo-treated patients; >60 days: 7/216 Xigris-treated patients versus 5/211 placebo-treated patients).
All-cause mortality at 28 days was similar in the Xigris and placebo groups, as were the rates of all serious bleeding events, all serious adverse events, fatal CNS bleeding events, and major amputations.
The results of this study do not provide evidence of benefit of Xigris in pediatric patients with severe sepsis.
14.5 Study 4: Coadministration of Heparin for VTE Prophylaxis in Xigris-Treated Patients
A randomized, double-blind, placebo-controlled trial (“XPRESS”) investigated the safety of heparin for VTE prophylaxis when concomitantly administered with Xigris (96-hour infusion at 24 mcg/kg/hr) in adult patients with severe sepsis who were at high risk of death (n=1935).
Patients were randomized 1:1:2 to receive low molecular weight heparin enoxaparin (40 mg every 24 hours), unfractionated sodium heparin (5000 U every 12 hours), or placebo administered concomitantly with the Xigris infusion. The XPRESS trial did not evaluate the safety of dosing unfractionated heparin every 8 hours in adult patients with severe sepsis when concomitantly administered with Xigris. Outside the Xigris treatment period (prior to study entry and following Xigris infusion), the use of commercially available heparin was left to the discretion of the investigator.
The 28-day all-cause mortality was similar between the heparin-plus-Xigris group (enoxaparin and unfractionated heparin combined) and placebo-plus-Xigris group (28.2%, 275/976, and 31.8%, 305/959, respectively; RR: 0.89, 95% CI: 0.77-1.02). There were no significant differences between the heparin-plus-Xigris and placebo-plus-Xigris groups in the rate of either venous thrombotic or serious bleeding events, including intracranial hemorrhage. Prophylactic heparin increased the risk of non-serious bleeding compared with placebo over the treatment period of 0-6 days. The rate of ischemic stroke was lower in the heparin-plus-Xigris group over days 0-6 (heparin-plus-Xigris 3/976, 0.3% versus placebo-plus-Xigris, 12/959, 1.3%).
In the subgroup of 889 patients receiving commercially available heparin at study entry, those patients randomized to placebo had higher mortality [placebo-plus-Xigris 35.5% (154/434) versus heparin-plus-Xigris 26.8% (122/455)] and higher rate of serious adverse events [placebo-plus-Xigris 18.0% (78/434) versus heparin-plus-Xigris 11.6% (53/455)] compared with patients in whom commercial heparin was replaced by study heparin [see Warnings and Precautions (5.3)]. Increased serious adverse events in this subgroup included cardiac, gastrointestinal, and venous thrombotic events. In patients not receiving commercial heparin at study entry, mortality and the rate of serious adverse events were similar between heparin-plus-Xigris and placebo-plus-Xigris groups.
15. References
Knaus WA, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818-829.
16. How is Xigris supplied
16.1 How Supplied
Xigris is supplied in 5 mg and 20 mg single-use vials containing sterile, preservative-free, lyophilized drotrecogin alfa (activated).
- 5 mg vial individually packaged in a carton — NDC 0002-7559-01
- 20 mg vial individually packaged in a carton — NDC 0002-7561-01
16.2 Storage and Handling
Lyophilized Powder
Xigris vials should be stored in a refrigerator 2° to 8°C (36° to 46°F). Do not freeze. Protect vials of Xigris from light. Retain in carton until time of use.
Reconstituted Solution
Avoid exposing Xigris solutions to heat and/or direct sunlight. The intravenous solution should be prepared immediately after reconstitution of the Xigris in the vial(s). If the vial of reconstituted Xigris is not used immediately, it may be held at controlled room temperature 20° to 25°C (68° to 77°F), but must be used within 3 hours [see Dosage and Administration (2.2)].
Intravenous infusion pump using an infusion bag — After final dilution and preparation, the intravenous solution should be used at controlled room temperature 20° to 25°C (68° to 77°F) within 12 hours. If the intravenous solution is not administered immediately, the solution should be refrigerated at 2° to 8°C (36° to 46°F) for up to 12 hours. If the prepared solution is refrigerated prior to administration, the maximum time limit for use of the intravenous solution with an infusion bag, including dilution, refrigeration, and administration, is 24 hours[see Dosage and Administration (2.3)].
Intravenous infusion using a syringe pump — After final dilution and preparation, the intravenous solution should be used at controlled room temperature 20° to 25°C (68° to 77°F) within 12 hours. If the intravenous solution is not administered immediately, the solution should be refrigerated at 2° to 8°C (36° to 46°F) for up to 12 hours. If the prepared solution is refrigerated prior to administration, the maximum time limit for use of the intravenous solution with a syringe pump, including dilution, refrigeration, and administration, is 24 hours[see Dosage and Administration (2.4)].
17. Patient Counseling Information
Xigris is administered in the intensive care unit, and in this setting, patients may be unresponsive or may have difficulty comprehending counseling information.
Patients and patients' caregivers should be informed by their healthcare provider of the potential benefits and risks associated with Xigris, including the most common side effect, bleeding. Patients with clinical conditions likely to increase the risk of bleeding should be carefully evaluated and anticipated benefits weighed against potential risks associated with Xigris therapy [see Contraindications (4), Warnings and Precautions (5.1), and Adverse Reactions (6)].
| XIGRIS
drotrecogin alfa (activated) injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| XIGRIS
drotrecogin alfa (activated) injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Eli Lilly and Company (006421325) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Lonza Biologics Inc. | 093149750 | API MANUFACTURE, ANALYSIS | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Eli Lilly and Company | 006421325 | ANALYSIS | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| DSM Pharmaceuticals, Inc. | 076301910 | MANUFACTURE, ANALYSIS | |
More about Xigris (drotrecogin alfa)
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous coagulation modifiers
Related treatment guides
Copyright © 2001, 2008, Eli Lilly and Company. All rights reserved.