Elbasvir and Grazoprevir (Monograph)
Brand name: Zepatier
Drug class: HCV Replication Complex Inhibitors
Warning
- Risk of HBV Reactivation in Patients Coinfected with HCV and HBV
-
HBV reactivation, including cases resulting in fulminant hepatitis, hepatic failure, and death, reported in patients coinfected with HCV and HBV who were receiving or had completed treatment with HCV direct-acting antivirals (DAAs) and were not receiving HBV antiviral therapy.
-
Test all patients for evidence of current or prior HBV infection before initiating fixed combination of elbasvir and grazoprevir (elbasvir/grazoprevir).
-
Monitor patients coinfected with HCV and HBV for hepatitis flare or HBV reactivation during and after HCV treatment. Initiate appropriate management for HBV infection as clinically indicated.
Introduction
Antiviral; fixed combination containing elbasvir (HCV NS5A replication complex inhibitor [NS5A inhibitor]) and grazoprevir (HCV NS3/4A protease inhibitor).
Uses for Elbasvir and Grazoprevir
Chronic HCV Infection
Treatment of chronic HCV genotype 1 or genotype 4 infection in treatment-naive (have not previously received HCV treatment) or previously treated adults and pediatric patients ≥12 years of age or weighing ≥30 kg without cirrhosis or with compensated cirrhosis (Child-Pugh class A), including those with HIV coinfection.
Used alone or in conjunction with ribavirin, depending on HCV genotype and certain patient factors (e.g., previous treatment experience, presence of baseline polymorphisms).
Efficacy of 12-week elbasvir/grazoprevir regimen for treatment of HCV genotype 1a infection reduced when 1 or more NS5A resistance-associated polymorphisms at certain amino acid positions (28, 30, 31, 93) are present at baseline. Screening for NS5A resistance-associated polymorphisms recommended prior to initiation of treatment in patients with HCV genotype 1a infection.
Treatment of chronic HCV infection is complex and rapidly evolving; consult a specialist to obtain the most up-to-date information. Information from the American Association for the Study of Liver Diseases (AASLD), Infectious Diseases Society of America (IDSA), and International Antiviral Society–USA (IAS–USA) regarding diagnosis and management of HCV infection, including recommendations for initial treatment, is available at [Web].
Elbasvir and Grazoprevir Dosage and Administration
General
Pretreatment Screening
-
Test for evidence of current or prior HBV infection by measuring hepatitis B surface antigen (HBsAg) and hepatitis B core antibody (anti-HBc).
-
Screen for the presence of HCV nonstructural 5A (NS5A) resistance-associated polymorphisms in patients with HCV genotype 1a infection to determine the appropriate treatment regimen and treatment duration.
-
Perform appropriate laboratory tests to evaluate liver function.
Patient Monitoring
-
Perform appropriate laboratory tests to evaluate liver function at treatment week 8 and as clinically indicated. For patients receiving 16 weeks of therapy, perform additional hepatic laboratory testing at treatment week 12.
-
In patients with compensated cirrhosis (Child-Pugh class A) or evidence of advanced liver disease (e.g., portal hypertension), more frequent hepatic laboratory testing may be warranted.
-
In all patients with evidence of current or prior HBV infection: Monitor for clinical and laboratory signs (i.e., HBsAg, HBV DNA levels, serum aminotransferase and bilirubin concentrations) of hepatitis flare or HBV reactivation during and after treatment.
-
Monitor for signs and symptoms of hepatic decompensation (e.g., jaundice, ascites, hepatic encephalopathy, variceal hemorrhage).
Other General Considerations
-
For the treatment of chronic HCV infection, elbasvir and grazoprevir (elbasvir/grazoprevir) is used alone or in conjunction with ribavirin.
-
Specific regimen and duration of treatment depend on HCV genotype and certain patient factors (e.g., presence of compensated or decompensated cirrhosis, liver transplantation). Consider that relapse rates following treatment are affected by baseline host and viral factors and differ between treatment durations for certain subgroups.
Administration
Oral Administration
Administer orally once daily without regard to food.
Dosage
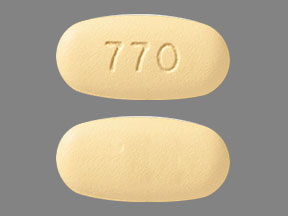
Available as fixed-combination tablets containing 50 mg of elbasvir and 100 mg of grazoprevir (elbasvir/grazoprevir).
Pediatric Patients
HCV Genotype 1a Infection
Oral
Pediatric patients ≥12 years of age or weighing ≥30 kg: 1 tablet (elbasvir 50 mg and grazoprevir 100 mg) once daily.
Use alone in patients without baseline NS5A polymorphisms who are treatment-naive or previously treated with peginterferon alfa and ribavirin; use in conjunction with ribavirin in those with baseline NS5A polymorphisms or in those previously treated with peginterferon alfa, ribavirin, and an HCV protease inhibitor. Treatment duration of 12 weeks recommended in most patients; treatment duration of 16 weeks recommended in those with baseline NS5A polymorphisms. (See Table 1.)
Previously treated defined as patients who failed treatment with peginterferon alfa and ribavirin.
NS5A resistance-associated polymorphisms at amino acid positions 28, 30, 31, or 93.
Use weight-based ribavirin dosage in patients with creatinine clearance >50 mL/minute (800 mg daily in those <66 kg, 1 g daily in those 66–80 kg, 1.2 g daily in those 81–105 kg, 1.4 g daily in those >105 kg); give ribavirin daily dosage in 2 divided doses with food.
Previously treated with an HCV protease inhibitor defined as patients who failed treatment with a regimen of peginterferon alfa, ribavirin, and an HCV NS3/4A protease inhibitor (e.g., boceprevir, simeprevir, telaprevir; drugs no longer commercially available).
The optimal elbasvir/grazoprevir-based regimen and duration of treatment not established for patients with HCV genotype 1a infection who previously failed treatment with peginterferon alfa, ribavirin, and an HCV protease inhibitor and have 1 or more baseline NS5A resistance-associated polymorphisms at positions 28, 30, 31, and 93.
|
Patient Type |
Multiple-drug Regimen |
Duration of Treatment |
|---|---|---|
|
Treatment-naive or previously treated without baseline NS5A polymorphisms |
Elbasvir/grazoprevir |
12 weeks |
|
Treatment-naive or previously treated with baseline NS5A polymorphisms |
Elbasvir/grazoprevir with ribavirin |
16 weeks |
|
Previously treated with an HCV protease inhibitor |
Elbasvir/grazoprevir with ribavirin |
12 weeks |
HCV Genotype 1b Infection
Oral
Pediatric patients ≥12 years of age or weighing ≥30 kg: 1 tablet (elbasvir 50 mg and grazoprevir 100 mg) once daily.
Use alone in patients who are treatment-naive or previously treated with peginterferon alfa and ribavirin; use in conjunction with ribavirin in those previously treated with peginterferon alfa, ribavirin, and an HCV protease inhibitor. Treatment duration of 12 weeks recommended. (See Table 2.)
Previously treated defined as patients who failed treatment with peginterferon alfa and ribavirin.
Previously treated with an HCV protease inhibitor defined as patients who failed treatment with a regimen of peginterferon alfa, ribavirin, and an HCV NS3/4A protease inhibitor (e.g., boceprevir, simeprevir, telaprevir; no longer commercially available).
Use weight-based ribavirin dosage in patients with Clcr >50 mL/minute (800 mg daily in those <66 kg, 1 g daily in those 66–80 kg, 1.2 g daily in those 81–105 kg, 1.4 g daily in those >105 kg); give ribavirin daily dosage in 2 divided doses with food.
|
Patient Type |
Multiple-drug Regimen |
Duration of Treatment |
|---|---|---|
|
Treatment-naive or previously treated |
Elbasvir/grazoprevir |
12 weeks |
|
Previously treated with an HCV protease inhibitor |
Elbasvir/grazoprevir with ribavirin |
12 weeks |
HCV Genotype 4 Infection
Oral
Pediatric patients ≥12 years of age or weighing ≥30 kg : 1 tablet (elbasvir 50 mg and grazoprevir 100 mg) once daily.
Use alone in patients who are treatment-naive; use in conjunction with ribavirin in those previously treated with peginterferon alfa and ribavirin. Treatment duration of 12 weeks recommended in treatment-naive patients; treatment duration of 16 weeks recommended in those previously treated with peginterferon alfa and ribavirin. (See Table 3.)
Previously treated defined as patients who failed treatment with peginterferon alfa and ribavirin.
Use weight-based ribavirin dosage in patients with Clcr >50 mL/minute (800 mg daily in those <66 kg, 1 g daily in those 66–80 kg, 1.2 g daily in those 81–105 kg, 1.4 g daily in those >105 kg); give ribavirin daily dosage in 2 divided doses with food.
|
Patient Type |
Multiple-drug Regimen |
Duration of Treatment |
|---|---|---|
|
Treatment-naive |
Elbasvir/grazoprevir |
12 weeks |
|
Previously treated |
Elbasvir/grazoprevir with ribavirin |
16 weeks |
HCV-infected with HIV Coinfection
Oral
Pediatric patients ≥12 years of age or weighing ≥30 kg: Use same elbasvir/grazoprevir dosage and same HCV genotype-specific multiple-drug regimen and duration of treatment recommended for HCV-infected patients without HIV coinfection. (See Table 1, Table 2, and Table 3.)
Adults
Treatment of Chronic HCV Infection
HCV Genotype 1a Infection
Oral1 tablet (elbasvir 50 mg and grazoprevir 100 mg) once daily.
Use alone in patients without baseline NS5A polymorphisms who are treatment-naive or previously treated with peginterferon alfa and ribavirin; use in conjunction with ribavirin in those with baseline NS5A polymorphisms or in those previously treated with peginterferon alfa, ribavirin, and an HCV protease inhibitor. Treatment duration of 12 weeks recommended in most patients; treatment duration of 16 weeks recommended in those with baseline NS5A polymorphisms. (See Table 4.)
Previously treated defined as patients who failed treatment with peginterferon alfa and ribavirin.
NS5A resistance-associated polymorphisms at amino acid positions 28, 30, 31, or 93.
Use weight-based ribavirin dosage in patients with Clcr >50 mL/minute (800 mg daily in those <66 kg, 1 g daily in those 66–80 kg, 1.2 g daily in those 81–105 kg, 1.4 g daily in those >105 kg); give ribavirin daily dosage in 2 divided doses with food.
Previously treated with an HCV protease inhibitor defined as patients who failed treatment with a regimen of peginterferon alfa, ribavirin, and an HCV NS3/4A protease inhibitor (e.g., boceprevir, simeprevir, telaprevir; no longer commercially available).
The optimal elbasvir/grazoprevir-based regimen and duration of treatment not established for patients with HCV genotype 1a infection who were previously treated with peginterferon alfa, ribavirin, and an HCV protease inhibitor and have 1 or more baseline NS5A resistance-associated polymorphisms at positions 28, 30, 31, and 93.
|
Patient Type |
Multiple-drug Regimen |
Duration of Treatment |
|---|---|---|
|
Treatment-naive or previously treated without baseline NS5A polymorphisms |
Elbasvir/grazoprevir |
12 weeks |
|
Treatment-naive or previously treated with baseline NS5A polymorphisms |
Elbasvir/grazoprevir with ribavirin |
16 weeks |
|
Previously treated with an HCV protease inhibitor, |
Elbasvir/grazoprevir with ribavirin |
12 weeks |
HCV Genotype 1b Infection
Oral1 tablet (elbasvir 50 mg and grazoprevir 100 mg) once daily.
Use alone in patients who are treatment-naive or previously treated with peginterferon alfa and ribavirin; use in conjunction with ribavirin in those previously treated with peginterferon alfa, ribavirin, and an HCV protease inhibitor. Treatment duration of 12 weeks recommended. (See Table 5.)
Previously treated defined as patients who failed treatment with peginterferon alfa and ribavirin.
Previously treated with an HCV protease inhibitor defined as patients who failed treatment with a regimen of peginterferon alfa, ribavirin, and an HCV NS3/4A protease inhibitor (e.g., boceprevir, simeprevir, telaprevir; no longer commercially available).
Use weight-based ribavirin dosage in patients with Clcr >50 mL/minute (800 mg daily in those <66 kg, 1 g daily in those 66–80 kg, 1.2 g daily in those 81–105 kg, 1.4 g daily in those >105 kg); give ribavirin daily dosage in 2 divided doses with food.
|
Patient Type |
Multiple-drug Regimen |
Duration of Treatment |
|---|---|---|
|
Treatment-naive or previously treated |
Elbasvir/grazoprevir |
12 weeks |
|
Previously treated with an HCV protease inhibitor |
Elbasvir/grazoprevir with ribavirin |
12 weeks |
HCV Genotype 4 Infection
Oral1 tablet (elbasvir 50 mg and grazoprevir 100 mg) once daily.
Use alone in patients who are treatment-naive; use in conjunction with ribavirin in those previously treated with peginterferon alfa and ribavirin. Treatment duration of 12 weeks recommended in treatment-naive patients; treatment duration of 16 weeks recommended in those previously treated with peginterferon alfa and ribavirin. (See Table 6.)
Previously treated defined as patients who failed treatment with peginterferon alfa and ribavirin.
Use weight-based ribavirin dosage in patients with Clcr >50 mL/minute (800 mg daily in those <66 kg, 1 g daily in those 66–80 kg, 1.2 g daily in those 81–105 kg, 1.4 g daily in those >105 kg); give ribavirin daily dosage in 2 divided doses with food.
|
Patient Type |
Multiple-drug Regimen |
Duration of Treatment |
|---|---|---|
|
Treatment-naive |
Elbasvir/grazoprevir |
12 weeks |
|
Previously treated |
Elbasvir/grazoprevir with ribavirin |
16 weeks |
HCV-infected with HIV Coinfection.
OralHCV genotype 1 or 4: Use same elbasvir/grazoprevir dosage and same HCV genotype-specific multiple-drug regimen and duration of treatment recommended for HCV-infected patients without HIV coinfection. (See Table 4, Table 5, and Table 6.)
Special Populations
Hepatic Impairment
Mild hepatic impairment (Child-Pugh class A): Dosage adjustments not needed. Monitor for signs and symptoms of hepatic decompensation.
Moderate or severe hepatic impairment (Child-Pugh class B or C) or any history of hepatic decompensation: Contraindicated.
Renal Impairment
Mild, moderate, or severe renal impairment, including those requiring hemodialysis: Dosage adjustments not needed.
Geriatric Patients
Dosage adjustments not needed.
Cautions for Elbasvir and Grazoprevir
Contraindications
-
Moderate or severe hepatic impairment (Child-Pugh class B or C) or any history of hepatic decompensation.
-
Concomitant use with certain drugs (e.g., inhibitors of organic anion transporting polypeptide [OATP] 1B1 and 1B3, potent inducers of CYP3A, efavirenz).
-
If elbasvir/grazoprevir used in conjunction with ribavirin, the contraindications to ribavirin also apply.
Warnings/Precautions
Warnings
Risk of HBV Reactivation in Patients Coinfected with HCV and HBV
Postmarketing reports of reactivation of HBV infection when DAAs were used for treatment of HCV infection in patients with HBV coinfection; fulminant hepatitis, hepatic failure, and death reported in some cases.
HBV reactivation (abrupt increase in HBV replication manifested as rapid increase in serum HBV DNA levels or detection of HBsAg in an individual who was previously HBsAg negative and anti-HBc positive) reported in patients with HCV and HBV coinfection receiving HCV treatment with a regimen that included HCV DAAs without interferon alfa. HBV reactivation usually occurred within 4–8 weeks after initiation of HCV treatment.
Patients with HBV reactivation heterogeneous in terms of HCV genotype and baseline HBV disease. Some patients were HBsAg positive; others had serologic evidence of resolved HBV infection (i.e., HBsAg negative and anti-HBc positive).
HBV reactivation also reported in patients receiving certain immunosuppressant or chemotherapeutic drugs; risk of reactivation associated with HCV DAAs may be increased in such patients.
Mechanism for HBV reactivation in coinfected patients receiving HCV DAAs unknown. Although HCV DAAs not known to cause immunosuppression, HBV reactivation in coinfected patients may result from a complex interplay of host immunologic responses in the setting of infection with 2 hepatitis viruses.
Prior to initiating treatment with an HCV DAA, including elbasvir/grazoprevir, screen all patients for evidence of current or prior HBV infection by measuring HBsAg, anti-HBs, and anti-HBc. Initiate appropriate management for HBV infection as clinically indicated.
In all patients with evidence of current or prior HBV infection, monitor for clinical and laboratory signs (i.e., HBsAg, HBV DNA levels, serum aminotransferase and bilirubin concentrations) of hepatitis flare or HBV reactivation during and after treatment with HCV DAAs. Initiate appropriate management for HBV infection as clinically indicated.
Advise coinfected patients to immediately contact a clinician if they develop any signs or symptoms of serious liver injury.
When making decisions regarding HBV monitoring or HBV treatment in coinfected patients, consult a clinician with expertise in managing HBV infection.
Other Warnings/Precautions
Risk of Hepatic Decompensation or Failure in Patients with Evidence of Advanced Liver Disease
Postmarketing reports of hepatic decompensation or failure, including some fatalities, in patients receiving HCV treatment regimens containing an HCV NS3/4A protease inhibitor, including elbasvir/grazoprevir. Data insufficient to estimate frequency of such events; causal relationship not established. Hepatic decompensation or failure usually occurred within first 4 weeks of HCV treatment.
Many of the reported cases of hepatic decompensation or failure occurred in patients with evidence of advanced liver disease with moderate or severe hepatic impairment (Child-Pugh class B or C) prior to initiation of HCV treatment. Some cases occurred in patients reported as noncirrhotic or as having compensated cirrhosis with mild liver impairment (Child-Pugh class A) at baseline, but with a history of a decompensation event or evidence of portal hypertension or decreased platelet counts at baseline. Some cases also reported in patients who had confounding factors (e.g., serious liver-related comorbidities).
If elbasvir/grazoprevir used in patients who have compensated cirrhosis (Child-Pugh class A) or evidence of advanced liver disease (e.g., portal hypertension), perform hepatic function tests as clinically indicated and monitor for signs and symptoms of hepatic decompensation (e.g., jaundice, ascites, hepatic encephalopathy, variceal hemorrhage).
Discontinue elbasvir/grazoprevir in patients who develop evidence of hepatic decompensation or failure.
Advise patients to contact a clinician if they develop any signs or symptoms of worsening liver disease.
Hepatic Effects
Increased ALT concentrations (>5 times ULN) reported in 1% of patients in clinical trials. Generally occurs at ≥8 weeks after initiation of treatment (mean onset 10 weeks; range 6–12 weeks); typically asymptomatic and resolved with ongoing treatment or completion of treatment. Increased rates of late-onset ALT elevations reported in patients with increased grazoprevir plasma concentrations and in certain patient groups (e.g., ≥65 years of age, Asian descent, females). Incidence of late-onset ALT elevations apparently not affected by presence of cirrhosis or treatment duration.
Increased bilirubin (>2.5 times ULN) reported in 6% of patients in clinical trials receiving elbasvir/grazoprevir in conjunction with ribavirin compared with <1% of patients receiving elbasvir/grazoprevir alone. Bilirubin increases were predominately indirect bilirubin and typically not associated with increased ALT concentrations.
Perform hepatic laboratory testing prior to treatment, at treatment week 8, at treatment week 12 (in those receiving 16 weeks of therapy), and as clinically indicated.
Consider discontinuance of elbasvir/grazoprevir if ALT concentrations remain persistently >10 times ULN. Discontinue if ALT elevations are accompanied by signs or symptoms of liver inflammation or increasing conjugated bilirubin, alkaline phosphatase, or INR. Advise patients to immediately contact clinician if onset of fatigue, weakness, lack of appetite, nausea and vomiting, jaundice, or discolored feces is observed.
Interactions
Concomitant use of elbasvir/grazoprevir and certain drugs is contraindicated or not recommended. Some drug interactions may result in loss of therapeutic effect and possible development of resistance to elbasvir/grazoprevir; other interactions may lead to adverse reactions from increased exposures of concomitant drugs or elbasvir/grazoprevir.
Consider potential for drug interactions prior to and during treatment. Review concomitant drugs during treatment; monitor patient for adverse reactions associated with the concomitant drugs.
Precautions Related to Fixed Combinations and Multiple-drug Treatment Regimens
Consider cautions, precautions, contraindications, and drug interactions associated with both drugs in the fixed combination. Consider cautionary information applicable to specific populations (e.g., pregnant or nursing women, individuals with hepatic or renal impairment, geriatric patients) for both elbasvir and grazoprevir.
When elbasvir/grazoprevir is used in conjunction with ribavirin, consider the usual cautions, precautions, and contraindications associated with ribavirin in addition to those associated with elbasvir/grazoprevir .
Specific Populations
Pregnancy
Adequate data regarding use of elbasvir/grazoprevir in pregnant women not available. In animal studies using elbasvir or grazoprevir, no evidence of fetal harm at exposures greater than those attained with recommended human dosage.
When used in conjunction with ribavirin, consider that ribavirin is contraindicated in pregnant women and male partners of pregnant women.
Lactation
Not known whether elbasvir/grazoprevir distributes into human milk, affects human milk production, or affects breast-fed infant; both elbasvir and grazoprevir are distributed into milk in rats.
Consider benefits of breast-feeding and importance of the drug to the woman; also consider potential adverse effects on the breast-fed child from the drug or underlying maternal condition.
When used in conjunction with ribavirin, consider potential for adverse reactions to ribavirin in nursing infants in addition to those associated with elbasvir/grazoprevir.
Pediatric Use
Safety and efficacy not established in pediatric patients <12 years of age or who weigh <30 kg.
Geriatric Use
Increased rate of late-onset ALT elevations reported in adults ≥65 years of age.
Elbasvir and grazoprevir AUCs reported in individuals ≥65 years of age increased compared with AUCs reported in younger adults.
Hepatic Impairment
Mild hepatic impairment or compensated cirrhosis (Child-Pugh class A): Monitor for signs and symptoms of hepatic decompensation (e.g., jaundice, ascites, hepatic encephalopathy, variceal hemorrhage).
Moderate or severe hepatic impairment (Child-Pugh class B or C) or any history of hepatic decompensation: Contraindicated. Postmarketing reports of hepatic decompensation or failure in such patients.
Efficacy and safety not established in liver transplant recipients or pretransplant patients.
Mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, or C) without HCV infection: Elbasvir AUCs similar but grazoprevir AUCs increased (12-fold higher in those with severe hepatic impairment) compared with AUCs in individuals with normal hepatic function.
Compensated cirrhosis in HCV-infected adults: Elbasvir AUCs similar but grazoprevir AUCs slightly higher compared with those reported in HCV-infected adults without cirrhosis.
Renal Impairment
Severe renal impairment (including those requiring dialysis): Increased elbasvir and grazoprevir exposures compared with exposures in individuals without severe renal impairment. Not considered clinically important.
Elbasvir and grazoprevir not removed by hemodialysis; unlikely to be removed by peritoneal dialysis.
Race
Asian patients: Higher rate of late-onset ALT elevations reported in clinical trials. Elbasvir and grazoprevir AUCs estimated to be increased by 15 and 50%, respectively, compared with AUCs reported in white individuals; dosage adjustments not needed based on race.
Black or African American individuals: Estimated elbasvir and grazoprevir exposures are comparable to those in white individuals.
Gender
Females: Higher rate of late-onset ALT elevations reported in clinical trials. Elbasvir and grazoprevir AUCs estimated to be increased by 50 and 30%, respectively, compared with AUCs reported in males; dosage adjustments not needed based on gender.
Common Adverse Effects
Elbasvir/grazoprevir: Fatigue, headache, nausea.
Elbasvir/grazoprevir in conjunction with ribavirin: Anemia, headache.
Drug Interactions
Elbasvir and grazoprevir are substrates of CYP3A; grazoprevir is a weak inhibitor of CYP3A. Elbasvir and grazoprevir inhibit CYP1A2, 2B6, 2C8, 2C9, 2C19, and 2D6.
Elbasvir inhibits P-gp transport system; elbasvir and grazoprevir are substrates of P-gp.
Elbasvir and grazoprevir inhibit intestinal breast cancer resistance protein (BCRP).
Grazoprevir is a substrate and inhibitor of OATP1B1 and 1B3.
The following drug interactions based on studies using elbasvir/grazoprevir, elbasvir alone, or grazoprevir alone, or are predicted drug interactions that may occur with elbasvir/grazoprevir. When elbasvir/grazoprevir is used, consider interactions associated with both drugs in the fixed combination.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Potent CYP3A inducers: Possible pharmacokinetic interactions (decreased elbasvir and grazoprevir concentrations and possible loss of therapeutic effect); concomitant use contraindicated.
Moderate CYP3A inducers: Possible pharmacokinetic interactions (decreased elbasvir and grazoprevir concentrations and possible reduced therapeutic effect); concomitant use not recommended.
Potent CYP3A inhibitors: Possible pharmacokinetic interactions (increased elbasvir and grazoprevir concentrations); concomitant use not recommended.
Drugs Affecting or Affected by Breast Cancer Resistance Protein
BCRP substrates: Possible pharmacokinetic interactions (increased concentrations of BCRP substrate).
Drugs Affecting or Affected by Organic Anion Transport Polypeptides
OATP1B1 or 1B3 inhibitors: Possible pharmacokinetic interactions (increased grazoprevir concentrations); concomitant use contraindicated with drugs known or suspected to increase grazoprevir concentrations.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids |
Dosage adjustments not needed if used concomitantly with antacids |
|
|
Anticonvulsants (carbamazepine, phenytoin) |
Carbamazepine, phenytoin: Possible decreased elbasvir and grazoprevir concentrations; possible loss of virologic response to the HCV antiviral |
Carbamazepine, phenytoin: Concomitant use contraindicated |
|
Antidiabetic agents |
Altered blood glucose control resulting in serious symptomatic hypoglycemia reported when DAAs used in diabetic patients receiving antidiabetic agents |
Frequently monitor glucose concentrations; dosage adjustment of antidiabetic agent may be needed |
|
Antifungals, azoles (ketoconazole) |
Ketoconazole: Increased elbasvir and grazoprevir concentrations and AUC; may increase risk of hepatotoxicity |
Concomitant use not recommended |
|
Antimycobacterials, rifamycins (rifampin) |
Rifampin: Multiple doses result in clinically important decreases in grazoprevir concentrations and is expected to result in clinically important decreases in elbasvir concentrations; may lead to loss of virologic response to the HCV antiviral |
Concomitant use contraindicated |
|
Antiretrovirals, HIV entry and fusion inhibitors |
Maraviroc: No effect on maraviroc pharmacokinetics expected |
Maraviroc: Dosage adjustments not needed |
|
Antiretrovirals, HIV integrase inhibitors (INSTIs) |
Bictegravir: No effect on bictegravir pharmacokinetics expected Dolutegravir: No clinically important effects on elbasvir, grazoprevir, or dolutegravir pharmacokinetics Cobicistat-boosted elvitegravir: Increased elbasvir and grazoprevir concentrations expected Fixed combination of elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate (EVG/c/FTC/TDF): Increased elbasvir and grazoprevir concentrations Fixed combination of elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide fumarate (EVG/c/FTC/TAF): Possible increased elbasvir and grazoprevir concentrations Raltegravir: No clinically important effects on elbasvir, grazoprevir, or raltegravir pharmacokinetics |
Bictegravir: Dosage adjustments not needed Dolutegravir: Dosage adjustments not needed Cobicistat-boosted elvitegravir, including EVG/c/FTC/TDF or EVG/c/FTC/TAF: Concomitant use with elbasvir/grazoprevir not recommended Raltegravir: Dosage adjustments not needed |
|
Antiretrovirals, HIV nonnucleoside reverse transcriptase inhibitors (NNRTIs) |
Doravirine: No clinically important effect on pharmacokinetics of elbasvir or grazoprevir; possible increased doravirine AUC Efavirenz: Substantially decreased elbasvir and grazoprevir concentrations; possible loss of virologic response to the HCV antiviral Etravirine: Possible decreased elbasvir and grazoprevir concentrations; possible reduced therapeutic effect of the HCV antiviral Nevirapine: Decreased elbasvir and grazoprevir concentrations expected Rilpivirine: No clinically important effects on elbasvir, grazoprevir, or rilpivirine pharmacokinetics |
Doravirine: Dosage adjustments not needed Efavirenz: Concomitant use contraindicated Etravirine: Concomitant use not recommended Nevirapine: Concomitant use not recommended Rilpivirine: Dosage adjustments not needed |
|
Antiretrovirals, HIV nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs) |
Abacavir: Clinically important pharmacokinetic interactions not expected Emtricitabine: Clinically important pharmacokinetic interactions not expected Lamivudine: Clinically important pharmacokinetic interactions not expected TDF: No clinically important effects on elbasvir, grazoprevir, or tenofovir pharmacokinetics |
TDF: Dosage adjustments not needed |
|
Antiretrovirals, HIV protease inhibitors (PIs) |
Ritonavir-boosted atazanavir: Increased elbasvir concentrations and substantially increased grazoprevir concentrations; may increase risk of ALT elevations Ritonavir-boosted darunavir: Increased elbasvir concentrations and substantially increased grazoprevir concentrations; may increase risk of ALT elevations Fixed combination of lopinavir and ritonavir (lopinavir/ritonavir): Increased elbasvir concentrations and substantially increased grazoprevir concentrations; may increase risk of ALT elevations Ritonavir: Increased grazoprevir concentrations Saquinavir: Substantially increased grazoprevir concentrations expected; may increase risk of ALT elevations Tipranavir: Substantially increased grazoprevir concentrations expected; may increase risk of ALT elevations |
Ritonavir-boosted, cobicistat-boosted, or unboosted atazanavir: Concomitant use with elbasvir/grazoprevir contraindicated Ritonavir-boosted or cobicistat-boosted darunavir: Concomitant use with elbasvir/grazoprevir contraindicated Lopinavir/ritonavir: Concomitant use contraindicated Saquinavir or ritonavir-boosted saquinavir: Concomitant use with elbasvir/grazoprevir contraindicated Ritonavir-boosted tipranavir: Concomitant use with elbasvir/grazoprevir contraindicated |
|
Benzodiazepines (midazolam) |
Midazolam: Increased midazolam exposures |
|
|
Bosentan |
Possible decreased elbasvir and grazoprevir concentrations; possible reduced therapeutic effect of the HCV antiviral |
Concomitant use not recommended |
|
Buprenorphine |
Fixed combination of buprenorphine and naloxone (buprenorphine/naloxone): No clinically important effects on elbasvir or grazoprevir pharmacokinetics |
Dosage adjustments not needed |
|
Corticosteroids (prednisone) |
Prednisone: No clinically important effects on elbasvir, grazoprevir, or prednisone pharmacokinetics |
Dosage adjustments not needed |
|
Digoxin |
No clinically important effects on digoxin pharmacokinetics |
Dosage adjustments not needed |
|
Entecavir |
Clinically important pharmacokinetic interactions not expected |
|
|
Estrogens/progestins |
Oral contraceptive containing ethinyl estradiol and levonorgestrel: No clinically important effects on pharmacokinetics of ethinyl estradiol or levonorgestrel |
Dosage adjustments not needed |
|
Histamine H2-receptor antagonists (famotidine) |
Famotidine: No clinically important effects on elbasvir or grazoprevir pharmacokinetics |
Histamine H2-receptor antagonists: Dosage adjustments not needed |
|
HMG-CoA reductase inhibitors (statins) |
Atorvastatin: Increased atorvastatin concentrations and AUC Fluvastatin, lovastatin, simvastatin: Possible increased statin concentrations Pitavastatin, pravastatin: No clinically important effects on pitavastatin or pravastatin pharmacokinetics Rosuvastatin: Increased rosuvastatin concentrations and AUC |
Atorvastatin: Do not exceed atorvastatin dosage of 20 mg once daily Fluvastatin, lovastatin, simvastatin: Use lowest necessary statin dosage; monitor for statin-associated adverse effects (e.g., myopathy) Pitavastatin, pravastatin: Dosage adjustments not needed Rosuvastatin: Do not exceed rosuvastatin dosage of 10 mg once daily |
|
Immunosuppressants (cyclosporine, tacrolimus) |
Cyclosporine: Increased elbasvir concentrations and AUC; substantially increased grazoprevir concentrations and AUC; may increase risk of ALT elevations Tacrolimus: Increased tacrolimus concentrations; no effect on elbasvir and grazoprevir concentrations |
Cyclosporine: Concomitant use contraindicated Tacrolimus: Frequently monitor tacrolimus whole blood concentrations, renal function, and tacrolimus-associated adverse effects |
|
Methadone |
No clinically important effects on elbasvir or grazoprevir pharmacokinetics |
Dosage adjustments not needed |
|
Modafinil |
Possible decreased elbasvir and grazoprevir concentrations; possible reduced therapeutic effect of the HCV antiviral |
Concomitant use not recommended |
|
Montelukast |
No clinically important effects on montelukast pharmacokinetics |
|
|
Mycophenolate mofetil |
No clinically important effects on elbasvir, grazoprevir, or mycophenolic acid pharmacokinetics |
Dosage adjustments not needed |
|
Nafcillin |
Possible decreased elbasvir and grazoprevir concentrations; possible reduced therapeutic effect of the HCV antiviral |
Concomitant use not recommended |
|
Phosphate binders (calcium acetate, sevelamer) |
Calcium acetate, sevelamer: No clinically important effects on elbasvir or grazoprevir pharmacokinetics |
Phosphate binders: Dosage adjustments not needed |
|
Proton-pump inhibitors (pantoprazole) |
Pantoprazole: No clinically important effects on elbasvir or grazoprevir pharmacokinetics |
Proton-pump inhibitors: Dosage adjustments not needed |
|
Ribavirin |
No clinically important effects on elbasvir or grazoprevir pharmacokinetics No in vitro evidence of antagonistic anti-HCV effects |
Dosage adjustments not needed |
|
Sofosbuvir |
No clinically important effects on sofosbuvir pharmacokinetics |
Dosage adjustments not needed |
|
St. John's wort (Hypericum perforatum) |
Substantially decreased elbasvir and grazoprevir concentrations; may lead to loss of virologic response to the HCV antiviral |
Concomitant use contraindicated |
|
Warfarin |
INR fluctuations reported in patients receiving elbasvir/grazoprevir |
Frequently monitor INR; warfarin dosage adjustment may be needed |
Elbasvir and Grazoprevir Pharmacokinetics
Absorption
Bioavailability
Following oral administration of elbasvir/grazoprevir in HCV-infected adults, peak plasma concentrations of elbasvir and grazoprevir occur approximately 3 and 2 hours, respectively, after the dose.
Steady-state concentrations of elbasvir and grazoprevir attained within approximately 6 days with once-daily administration.
Elbasvir: Pharmacokinetics similar in healthy and HCV-infected adults; exposures increase in a dose-proportional manner over dosage range of 5–200 mg once daily.
Grazoprevir: Exposures approximately twofold higher in HCV-infected adults compared with healthy adults; studies using grazoprevir dosages of 10–800 mg once daily in HCV-infected adults indicate peak plasma concentrations and AUC increase in a more-than-dose-proportional manner.
Pediatric patients ≥12 years of age or weighing ≥30 kg: Safety, efficacy, and pharmacokinetics consistent with those observed in HCV-infected adults in clinical trials.
Concomitant use of elbasvir and grazoprevir does not have a clinically important effect on pharmacokinetics of either drug compared with administration alone.
Food
Elbasvir and grazoprevir: Effect of food not considered clinically important.
Administration of elbasvir/grazoprevir with a high-fat meal (approximately 900 kcal, 500 kcal from fat) in healthy individuals decreases elbasvir AUC and peak plasma concentrations by approximately 11 and 15%, respectively, and increases grazoprevir AUC and peak plasma concentrations by approximately 1.5- and 2.8-fold, respectively, relative to administration in the fasting state.
Special Populations
Elbasvir: In individuals with mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, or C) without HCV infection, no clinically important differences in AUCs compared with individuals with normal hepatic function.
Grazoprevir: In individuals with mild, moderate, or severe hepatic impairment (Child-Pugh class A, B, or C) without HCV infection, AUCs increased by 1.7-, 5-, or 12-fold, respectively, compared with individuals with normal hepatic function.
Elbasvir: In individuals with severe renal impairment (not dependent on dialysis) or individuals requiring hemodialysis, AUCs increased by 46 or 25%, respectively, compared with individuals without severe renal impairment.
Grazoprevir: In individuals with severe renal impairment (not dependent on dialysis) or individuals requiring hemodialysis, AUCs increased by 40 or 10%, respectively, compared with individuals without severe renal impairment.
Adults ≥65 years of age: Elbasvir and grazoprevir AUCs estimated to be increased by 16 and 45%, respectively, compared with AUCs in younger adults.
Asian individuals: Elbasvir and grazoprevir AUCs estimated to be increased by 15 and 50%, respectively, compared with white individuals.
Black or African American individuals: Elbasvir and grazoprevir AUCs comparable to those in white individuals.
Females: Elbasvir and grazoprevir AUCs estimated to be increased by 50 and 30%, respectively, compared with males.
Distribution
Extent
Elbasvir: Distributes into most tissues, including the liver, based on preclinical studies.
Grazoprevir: Distributes principally into the liver, based on preclinical studies; distribution into liver probably facilitated by active transport through OATP1B1 and 1B3.
Plasma Protein Binding
Elbasvir: 99.9%.
Grazoprevir: 98.8%.
Elimination
Metabolism
Elbasvir and grazoprevir both partially eliminated by oxidative metabolism, principally by CYP3A.
Elimination Route
Elbasvir and grazoprevir: >90% of dose excreted in feces; <1% excreted in urine.
Half-life
Elbasvir: Approximately 24 hours in HCV-infected adults.
Grazoprevir: Approximately 31 hours in HCV-infected adults.
Special Populations
Elbasvir and grazoprevir: Not removed by hemodialysis; removal by peritoneal dialysis unlikely since highly bound to plasma protein.
Stability
Storage
Oral
Film-coated Tablets
20–25°C (excursions permitted between 15–30°C).
Protect from moisture by storing in original blister package until used.
Actions and Spectrum
-
Elbasvir/grazoprevir is a fixed combination of 2 HCV antivirals. Elbasvir is an HCV NS5A replication complex inhibitor (NS5A inhibitor) and grazoprevir is an HCV NS3/4A protease inhibitor.
-
Elbasvir and grazoprevir are both direct-acting antivirals (DAAs) with activity against HCV. No in vitro evidence of antagonistic anti-HCV effects between the drugs in HCV replicon studies.
-
Elbasvir targets HCV NS5A protein, which is required for viral replication and virion assembly. In vitro studies using cell-based replicon assays indicate elbasvir has activity against HCV genotypes 1a, 1b, and 4.
-
Grazoprevir inhibits HCV NS3/4A protease, which is required for viral replication. Inhibition of NS3/4A protease prevents proteolytic cleavage of the HCV-encoded polyprotein to form mature forms of NS3, NS4A, NS4B, NS5A, and NS5B. In vitro studies using cell-based replicon assays indicate grazoprevir has activity against HCV genotypes 1a, 1b, and 4.
-
Certain amino acid substitutions in NS5A of HCV genotypes 1a, 1b, and 4 selected in cell culture and associated with reduced susceptibility to elbasvir in vitro in replicon studies. Single M28A/G/T, Q30D/E/H/K/R, L31M/V, H28D, and Y93C/H/N substitutions in HCV genotype 1a replicons confer reduced susceptibility to elbasvir; single L28M, L31F, and Y93H substitutions in HCV genotype 1b replicons are associated with reduced susceptibility to elbasvir. In HCV genotype 4 replicons, single L30S, M31V, and Y93H substitutions are associated with reduced susceptibility to elbasvir. In general, combinations of elbasvir resistance-associated substitutions further reduce elbasvir antiviral activity in HCV genotypes 1a, 1b, and 4 replicons. In phase 2 and 3 clinical trials, treatment-emergent amino acid substitutions in NS5A were detected in patients with HCV genotype 1a infection (M28A/G/T, Q30H/K/R/Y, L31F/M/V, H58D, Y93H/N/S), HCV genotype 1b infection (L28M, L31F/V, Y93H), or HCV genotype 4 infection (L28S/T, M31I/V, P58D, Y93H) experiencing virologic failure.
-
Certain amino acid substitutions in NS3 of HCV genotypes 1a, 1b, and 4 selected in cell culture and associated with reduced susceptibility to grazoprevir in vitro in replicon studies. Single Y56H, R155K, A156G/T/V, and D168A/E/G/N/S/V/Y substitutions in HCV genotype 1a replicons confer reduced susceptibility to grazoprevir; single F43S, Y56F, V107I, A156S/T/V, and D168A/G/V substitutions in HCV genotype 1b replicons confer reduced susceptibility to grazoprevir. In HCV genotype 4 replicons, single D168A/V substitutions are associated with reduced susceptibility to grazoprevir. In general, combinations of grazoprevir resistance-associated substitutions further reduce grazoprevir antiviral activity in HCV genotypes 1a, 1b, and 4 replicons. In phase 2 and 3 clinical trials, treatment-emergent amino acid substitutions in NS3 were detected in patients with HCV genotype 1a infection (V36L/M, Y56H, V107I, R155I/K, A156G/T/V, V158A, D168A/G/N/V/Y), HCV genotype 1b infection (Y56F, V107I, A156T), or HCV genotype 4 infection (A156M/T/V, D168A/G, V170I) experiencing virologic failure.
-
Possible cross-resistance among HCV NS5A inhibitors and among HCV NS3/4A protease inhibitors. Efficacy of elbasvir/grazoprevir not established in patients who failed previous treatment with a regimen that included an HCV NS5A inhibitor. Only limited data available regarding efficacy of elbasvir/grazoprevir in patients who failed previous treatment with a regimen of peginterferon alfa, ribavirin, and an HCV NS3/4A protease inhibitor (e.g., boceprevir, simeprevir, telaprevir; no longer commercially available) and have HCV NS3 resistance-associated substitutions at baseline prior to administration of elbasvir/grazoprevir. Elbasvir and grazoprevir active against HCV with amino acid substitutions associated with resistance to HCV NS5B polymerase inhibitors.
Advice to Patients
-
Inform patients of the importance of reading patient information provided by the manufacturer.
-
Advise patients that the fixed-combination preparation of elbasvir and grazoprevir (elbasvir/grazoprevir) should be taken once daily (with or without food) on a regular dosing schedule.
-
Inform patients of the importance of taking the recommended dosage of elbasvir/grazoprevir for the recommended duration of treatment; importance of not missing or skipping doses.
-
Inform patients that reactivation of hepatitis B virus (HBV) infection has occurred in coinfected patients being treated for hepatitis C virus (HCV) infection. Inform patients of the importance of informing clinician of any history of HBV infection or other liver problems (e.g., cirrhosis). Inform patients of the importance of immediately contacting a clinician if any signs or symptoms of serious liver injury (e.g., fatigue, weakness, loss of appetite, nausea and vomiting, yellowing of the eyes or skin, light-colored bowel movements) occur.
-
Advise patients to immediately contact a clinician if they have symptoms of worsening liver problems (e.g., nausea, vomiting, yellowing of skin or white part of the eyes, bleeding or bruising more easily than normal, confusion, loss of appetite, diarrhea, dark or brown urine, dark or bloody stools, abdominal swelling, pain in upper right side of stomach area, sleepiness, vomiting of blood).
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Advise women to inform clinicians if they are or plan to become pregnant or plan to breast-feed. If used in conjunction with ribavirin, advise men and women of importance of using 2 forms of effective contraception during and for 6 months after ribavirin therapy.
-
Advise patients of other important precautionary information.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
Elbasvir 50 mg and Grazoprevir 100 mg |
Zepatier |
Merck |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about elbasvir / grazoprevir
- Check interactions
- Compare alternatives
- Reviews (53)
- Side effects
- Dosage information
- During pregnancy
- Drug class: antiviral combinations
- En español