Tocilizumab (Monograph)
Brand names: Actemra, Tyenne, Tofidence
Drug class: Interleukin-mediated Agents, Miscellaneous
Warning
- Risk of Serious Infections
-
Serious, sometimes fatal infections including tuberculosis (pulmonary or extrapulmonary disease), bacterial and viral infections, invasive fungal infections (may be disseminated), and other opportunistic infections reported.
-
Carefully consider risks and benefits prior to initiating tocilizumab therapy in patients with chronic or recurring infections.
-
Evaluate patients, except for those with COVID-19, for latent tuberculosis infection prior to and periodically during tocilizumab therapy; if indicated, initiate appropriate antimycobacterial regimen prior to initiating tocilizumab therapy.
-
Closely monitor patients for infection, including active tuberculosis in those with a negative tuberculin skin test, during and after treatment. If serious infection develops, discontinue tocilizumab until infection is controlled.
Introduction
Tocilizumab, tocilizumab-aazg, and tocilizumab-bavi are biologic response modifiers and disease-modifying antirheumatic drugs (DMARDs); recombinant humanized IgG1 monoclonal antibodies specific for the interleukin-6 (IL-6) receptor.
Tocilizumab-aazg (Tyenne) and tocilizumab-bavi (Tofidence) are biosimilar to tocilizumab (Actemra). A biosimilar is a biological that is highly similar to an FDA-licensed reference biological with the exception of minor differences in clinically inactive components and for which there are no clinically meaningful differences in safety, purity, or potency. Biosimilars are approved through an abbreviated licensure pathway that establishes biosimilarity between proposed biological and reference biological but does not independently establish safety and effectiveness of the proposed biological. In order to be considered an interchangeable biosimilar, a biological product must meet additional requirements beyond demonstrating biosimilarity to its reference product. None of the currently available tocilizumab biosimilars has interchangeable data at this time.
In this monograph, unless otherwise stated, the term "tocilizumab products" refers to tocilizumab (the reference drug) and its biosimilars (tocilizumab-aazg and tocilizumab-bavi).
Uses for Tocilizumab
Rheumatoid Arthritis in Adults
Tocilizumab products: management of moderately to severely active rheumatoid arthritis (RA) in adults who have had an inadequate response to one or more DMARDs.
Can be used alone or in combination with methotrexate or other nonbiologic DMARDs (e.g., hydroxychloroquine, leflunomide, minocycline, sulfasalazine).
Do not use concomitantly with other biologic DMARDs, such as tumor necrosis factor (TNF; TNF-α) blocking agents (e.g., adalimumab, certolizumab, etanercept, golimumab, infliximab), interleukin-1 (IL-1) receptor antagonists (e.g., anakinra), anti-CD20 monoclonal antibodies (e.g., rituximab), and selective costimulation modulators (e.g., abatacept); concomitant use has not been studied and there is a possibility of increased immunosuppression and increased risk of infection.
Several studies have demonstrated potential efficacy of IV and subcutaneous tocilizumab for treatment-naïve patients† [off-label] with recent onset rheumatoid arthritis, although not FDA-labeled for use in such patients.
Guidelines recommend addition of a biologic DMARD such as tocilizumab for patients not at target with maximally tolerated doses of methotrexate.
Juvenile Idiopathic Arthritis (JIA)
Tocilizumab products: management of active systemic or polyarticular JIA in patients ≥2 years of age.
Can be used alone or in combination with methotrexate.
Do not use concomitantly with other biologic DMARDs; concomitant use has not been studied, and there is a possibility of increased immunosuppression and increased risk of infection.
Guidelines generally recommend biologic DMARDs, including tocilizumab, as an initial treatment option in patients with involvement of high-risk joints and as an add-on treatment for patients with inadequate response to other treatments.
Giant Cell Arteritis (GCA)
Tocilizumab products: management of GCA in adults.
Can be used in combination with a tapering course of corticosteroids or alone following discontinuance of corticosteroids.
Do not use concomitantly with other biologic DMARDs; concomitant use has not been studied, and there is a possibility of increased immunosuppression and increased risk of infection.
The American College of Rheumatology and Vasculitis Foundation issued a joint guideline in 2021 for the management of GCA. The guideline conditionally recommends the use of tocilizumab with oral glucocorticoids over oral glucocorticoids alone in patients with newly diagnosed GCA and patients who experience disease relapse with symptoms of cranial ischemia while receiving glucocorticoids.
Cytokine Release Syndrome (CRS) Associated with Chimeric Antigen Receptor (CAR) T-cell Therapy
Tocilizumab only: management of CAR T cell-induced severe or life-threatening CRS in adults and pediatric patients ≥2 years of age.
Can be used alone or in combination with corticosteroids.
Do not use concomitantly with other biologic DMARDs; concomitant use has not been studied, and there is a possibility of increased immunosuppression and increased risk of infection.
The American Society of Clinical Oncology (ASCO) issued a guideline in 2021 for the management of immune-related adverse events in patients treated with CAR T-cell therapy. The guideline recommends use of tocilizumab with or without a corticosteroid in patients with prolonged or severe CAR T-cell-associated CRS.
Systemic Sclerosis-Associated Interstitial Lung Disease (SSc-ILD)
Tocilizumab only: management of adults with SSc-ILD to reduce the rate of decline in pulmonary function.
Coronavirus Disease 2019 (COVID-19)
Tocilizumab and tocilizumab-bavi: management of COVID-19 in hospitalized adults who are receiving systemic corticosteroids and require supplemental oxygen, noninvasive or invasive mechanical ventilation, or extracorporeal membrane oxygenation (ECMO).
Rationale for use related to specificity of tocilizumab for the IL-6 receptor, which may help relieve symptoms of CRS (e.g., fever, organ failure, death) in severely ill patients with COVID-19.
Several studies have demonstrated efficacy and safety in hospitalized adult patients with severe COVID-19-related pneumonia to reduce mortality and hospital length of stay.
FDA has issued an emergency use authorization (EUA) for treatment of COVID-19 in hospitalized pediatric patients 2–17 years of age who are receiving systemic corticosteroids and require supplemental oxygen, non-invasive or invasive mechanical ventilation, or extracorporeal membrane oxygenation† [off-label] (ECMO). For additional information, consult the tocilizumab EUA letter of authorization ([Web]), EUA fact sheet for healthcare providers ([Web]), and EUA fact sheet for patients, parents and caregivers ([Web]) .
Tocilizumab Dosage and Administration
General
Pretreatment Screening
-
Consider potential risks and benefits of tocilizumab prior to initiating therapy in patients with chronic infection or history of recurrent infection. Do not administer in patients with an active infection until the infection resolves or is appropriately treated.
-
Evaluate all patients (except those with COVID-19) for active or inactive tuberculosis prior to initiation of tocilizumab therapy. Do not administer to patients with active tuberculosis.
-
Administer all age-appropriate vaccines prior to starting tocilizumab therapy.
-
Measure absolute neutrophil count (ANC), platelet count, and ALT and AST levels prior to initiating therapy. In patients with rheumatoid arthritis, GCA, SSc-ILD, polyarticular juvenile idiopathic arthritis (PJIA), or systemic juvenile idiopathic arthritis (SJIA), do not initiate therapy if ANC <2000/mm3, platelet count <100,000/mm3, or ALT or AST >1.5 times the ULN. In patients with COVID-19, do not initiate therapy if ANC <1000/mm3, platelet count <50,000/mm3, or ALT or AST >10 times ULN.
-
Perform a pregnancy test prior to initiating therapy in females of reproductive potential; if positive, enroll patients in manufacturer’s pregnancy registry.
Patient Monitoring
-
Monitor patients for signs and symptoms of bacterial, viral, or fungal infections.
-
Evaluate all patients (except for those with COVID-19) for active tuberculosis infection during treatment, even if initial latent tuberculosis test is negative.
-
Monitor patients who present with new-onset abdominal symptoms for signs of GI perforation.
-
Monitor lipid parameters approximately 4 to 8 weeks after start of therapy, and manage according to clinical guidelines.
-
Monitor patients for signs and symptoms of infusion-related and hypersensitivity reactions during and after infusions.
-
Monitor patients for signs and symptoms indicative of demyelinating disorders.
-
In patients with rheumatoid arthritis, GCA, or SSc-ILD: obtain a liver test panel (alkaline phosphatase, total bilirubin, ALT and AST levels) every 4 to 8 weeks after start of therapy for the first 6 months of treatment and every 3 months thereafter.
-
In patients with rheumatoid arthritis, GCA, SSc-ILD, or COVID-19: monitor ANC and platelet count 4 to 8 weeks after start of therapy and every 3 months thereafter.
-
In patients with PJIA: monitor liver test panel (alkaline phosphatase, total bilirubin, ALT and AST levels), ANC, and platelet count at the time of second administration and every 4 to 8 weeks thereafter.
-
In patients with SJIA: monitor liver test panel (alkaline phosphatase, total bilirubin, ALT and AST levels), ANC, and platelet count at the time of second administration and every 2 to 4 weeks thereafter.
Dispensing and Administration Precautions
-
IV infusions of tocilizumab should only be administered by a healthcare professional with appropriate medical support to manage anaphylaxis. If anaphylaxis or other hypersensitivity reaction occurs, stop administration of tocilizumab immediately and permanently discontinue therapy.
Other General Considerations
-
Patients with severe or life-threatening CAR T cell-induced cytokine release syndrome (CRS) frequently have cytopenias or elevated ALT or AST concentrations due to lymphodepleting chemotherapy or the CRS itself. Consider the potential benefit of treating the CRS versus the risks of short-term therapy with tocilizumab.
-
For the management of rheumatoid arthritis, tocilizumab products may be used as monotherapy or concomitantly with methotrexate or other nonbiologic disease-modifying antirheumatic drugs (DMARDs). Tocilizumab products may be used alone or in combination with methotrexate in patients with systemic or polyarticular juvenile idiopathic arthritis (JIA).
-
For the management of GCA, administer tocilizumab products initially in combination with a tapering course of corticosteroids. Once corticosteroids are discontinued, continue tocilizumab alone.
-
Do not use tocilizumab products concomitantly with other biologic DMARDs, such as tumor necrosis factor (TNF) blocking agents, interleukin-1 (IL-1) receptor antagonists, anti-CD20 monoclonal antibodies, and selective costimulation modulators.
Administration
Administer tocilizumab and tocilizumab-aazg by IV infusion or sub-Q injection in the management of rheumatoid arthritis, GCA, and polyarticular or systemic JIA. Tocilizumab-bavi is only approved for IV administration for these indications.
Administer tocilizumab by sub-Q injection in the management of SSc-ILD and by IV infusion only for CAR T cell-induced CRS. Not FDA-labeled for IV administration in the management of SSc-ILD or for sub-Q administration in the management of CRS.
Administer tocilizumab and tocilizumab-bavi by IV infusion for the management of COVID-19. Not FDA-labeled for sub-Q administration in the management of COVID-19.
IV Administration
Administer by IV infusion after dilution.
Tocilizumab products for IV use are commercially available in single-dose vials for IV infusion. The injection concentrate must be diluted prior to IV administration.
Allow diluted tocilizumab infusion solutions to reach room temperature prior to administration.
Do not infuse tocilizumab simultaneously through the same IV line with other drugs.
Dilution
Tocilizumab and tocilizumab-aazg:Dilute tocilizumab and tocilizumab-aazg injection concentrate (20 mg/mL) in an infusion bag or bottle containing 0.9 or 0.45% sodium chloride injection to provide a total volume of 50 mL (for patients who weigh <30 kg) or 100 mL (for patients who weigh ≥30 kg). Remove a volume of diluent equal to the total required volume of the injection concentrate from the bag or bottle of 0.9 or 0.45% sodium chloride injection prior to adding the injection concentrate. Slowly add the total required volume of tocilizumab injection concentrate (0.2, 0.3, 0.4, 0.5, or 0.6 mL/kg for a dose of 4, 6, 8, 10, or 12 mg/kg, respectively) to the diluent; gently invert bag or bottle to mix the solution and avoid foaming.
Tocilizumab-bavi:For tocilizumab-bavi, preparation and administration instructions are similar to tocilizumab and tocilizumab-aazg except only 0.9% sodium chloride injection may be utilized for dilution.
Fully diluted tocilizumab infusion solutions are compatible with infusion bags and/or infusion sets made with varying materials; refer to the labeling for each tocilizumab product for further information.
Discard any unused portion remaining in the vial since the injection concentrate contains no preservative.
Rate of Administration
Infuse dose over 60 minutes; do not administer by rapid IV injection (e.g., IV push or bolus).
Sub-Q Administration
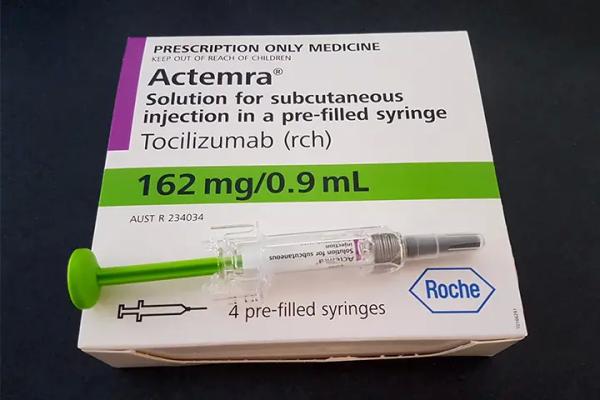
Tocilizumab and tocilizumab-aazg for sub-Q use are commercially available in prefilled single-dose syringes and prefilled single-dose autoinjectors. Each syringe or autoinjector delivers 162 mg of tocilizumab in 0.9 mL.
Intended for use under the guidance of a clinician, but may be self-administered if the clinician determines that the patient and/or their caregiver is competent to safely administer the drug after appropriate training. Patients with polyarticular or systemic JIA may self-administer tocilizumab if both clinician and the parent/legal guardian determine it is appropriate.
Allow to sit at room temperature outside of carton for 30 minutes (for the prefilled syringe) or 45 minutes (for the autoinjector) prior to injection; do not warm tocilizumab in any other way (e.g., microwave, hot water).
Administer sub-Q injections into anterior thigh or abdomen (except for the 2-inch area around the umbilicus); may be administered into upper arm by a caregiver. Rotate injection sites. Do not make injections into areas where the skin is tender, bruised, red, hard, or nonintact or into scars or moles.
Do not use the commercially available sub-Q injection for IV administration.
Dosage
Pediatric Patients
Juvenile Idiopathic Arthritis (JIA)
IV
Tocilizumab products: Polyarticular JIA in patients ≥2 years of age: 10 mg/kg once every 4 weeks in those weighing <30 kg; 8 mg/kg once every 4 weeks in those weighing ≥30 kg.
Tocilizumab products: Systemic JIA in patients ≥2 years of age: 12 mg/kg once every 2 weeks in those weighing <30 kg; 8 mg/kg once every 2 weeks in those weighing ≥30 kg.
Do not adjust dosage based solely on patient's weight as measured at a single visit, as weight may fluctuate.
Sub-Q
Tocilizumab or tocilizumab-aazg: Polyarticular JIA in patients ≥2 years of age: 162 mg once every 3 weeks in those weighing <30 kg; 162 mg once every 2 weeks in those weighing ≥30 kg.
Tocilizumab or tocilizumab-aazg: Systemic JIA in patients ≥2 years of age: 162 mg every 2 weeks in those weighing <30 kg; 162 mg once weekly in those weighing ≥30 kg.
Do not adjust dosage based solely on patient's weight as measured at a single visit, as weight may fluctuate.
When switching from IV to sub-Q administration, administer first sub-Q dose in place of the next scheduled IV dose.
Treatment Interruption or Discontinuance for Toxicity
IV or Sub-QIf certain dose-related laboratory changes (i.e., elevated ALT or AST concentrations, neutropenia, thrombocytopenia) occur, interrupt tocilizumab therapy at values similar to those considered in adults with rheumatoid arthritis . If clinically appropriate, consider dosage reduction or discontinuance of concomitant methotrexate and/or other therapy and withhold tocilizumab pending clinical evaluation. Individualize the decision to discontinue tocilizumab.
Tocilizumab dosage reductions not evaluated in patients with polyarticular or systemic JIA.
CRS Associated with CAR T-cell Therapy
IV
May use tocilizumab alone or in combination with corticosteroids.
Tocilizumab only: Pediatric patients ≥2 years of age who weigh <30 kg: 12 mg/kg by IV infusion over 60 minutes.
Tocilizumab only: Pediatric patients ≥2 years of age who weigh ≥30 kg: 8 mg/kg (maximum 800 mg) by IV infusion over 60 minutes.
If clinical improvement does not occur following the first dose, may administer ≤3 additional doses. The interval between consecutive doses should be ≥8 hours.
COVID-19 Infection
IV
The FDA EUA that permits use of tocilizumab for treatment of COVID-19 in certain hospitalized pediatric patients 2–17 years of age † [off-label] treatment of COVID-19 in hospitalized pediatric patients† [off-label] states that those weighing <30 kg can receive a dosage of 12 mg/kg (maximum of 800 mg per infusion) given as a single 60-minute IV infusion; may administer one additional IV infusion ≥8 hours after the first infusion if clinical signs or symptoms worsen or do not improve after the initial dose. Those 2–17 years of age weighing ≥30 kg can receive a dosage of 8 mg/kg (maximum of 800 mg per infusion) given as a single 60-minute IV infusion; may administer one additional IV infusion ≥8 hours after the first infusion if clinical signs or symptoms worsen or do not improve after the initial dose.
Adults
Rheumatoid Arthritis
IV
Tocilizumab products: Initially, 4 mg/kg once every 4 weeks; may increase to 8 mg/kg once every 4 weeks based on clinical response. Doses >800 mg per infusion are not recommended.
Sub-Q
Tocilizumab or tocilizumab-aazg: Adults weighing <100 kg: 162 mg every other week; may increase to 162 mg every week based on clinical response.
Tocilizumab or tocilizumab-aazg: Adults weighing ≥100 kg: 162 mg every week.
When switching from IV to sub-Q administration, administer first sub-Q dose in place of the next scheduled IV dose.
GCA
IV
Tocilizumab products: Recommended dosage: 6 mg/kg (maximum 600 mg) every 4 weeks in combination with a tapering course of glucocorticoids. May use tocilizumab alone following discontinuance of glucocorticoids.
Sub-Q
Tocilizumab or tocilizumab-aazg: Recommended dosage: 162 mg every week in combination with a tapering course of corticosteroids. A dosage of 162 mg given once every other week also may be prescribed based on clinical considerations. May use tocilizumab alone following discontinuance of corticosteroids.
When switching from IV to sub-Q administration, administer first sub-Q dose in place of the next scheduled IV dose.
Systemic Sclerosis-Associated Interstitial Lung Disease
Sub-Q
Tocilizumab only: Recommended dosage: 162 mg every week.
CRS Associated with CAR T-cell Therapy
IV
May use tocilizumab alone or in combination with corticosteroids.
Tocilizumab only: 8 mg/kg (maximum 800 mg) by IV infusion over 60 minutes.
If clinical improvement does not occur following the first dose, may administer ≤3 additional doses. The interval between consecutive doses should be ≥8 hours.
COVID-19
IV
Tocilizumab or tocilizumab-bavi: Recommended dosage: 8 mg/kg (maximum 800 mg) given as a single IV infusion over 60 minutes.
If clinical signs or symptoms worsen or do not improve after the first dose, may administer one additional infusion ≥8 hours after the initial infusion.
Dosage Modification for Serious Infections or Laboratory Abnormalities
If a serious infection, an opportunistic infection, or sepsis develops, discontinue tocilizumab products until the infection is controlled.
|
ALT or AST Value |
Recommendation for RA and SSc-ILD |
Recommendation for GCA |
|---|---|---|
|
>1 to 3 times ULN |
Modify dosage of concomitant DMARDs if appropriate |
Modify dosage of concomitant immunomodulatory agents if appropriate |
|
For persistent increases within this range in patients receiving IV tocilizumab, reduce dose of tocilizumab to 4 mg/kg or withhold therapy until ALT/AST values normalize |
For persistent increases within this range in patients receiving IV tocilizumab, withhold therapy until ALT/AST values normalize |
|
|
For persistent increases within this range in patients receiving sub-Q tocilizumab, reduce frequency of tocilizumab administration to every other week or withhold therapy until ALT/AST values normalize; resume tocilizumab at every other week and increase frequency to every week as clinically indicated |
For persistent increases within this range in patients receiving sub-Q tocilizumab, reduce frequency of tocilizumab administration to every other week or withhold therapy until ALT/AST values normalize; resume tocilizumab at every other week and increase frequency to every week as clinically indicated |
|
|
>3 to 5 times ULN (confirmed by repeat testing) |
Interrupt tocilizumab therapy until ALT/AST <3 times ULN and follow recommendations for ALT/AST >1 to 3 times ULN |
Interrupt tocilizumab therapy until ALT/AST <3 times ULN and follow recommendations for ALT/AST >1 to 3 times ULN |
|
For persistent increases of >3 times ULN, discontinue tocilizumab |
For persistent increases of >3 times ULN, discontinue tocilizumab |
|
|
>5 times ULN |
Discontinue tocilizumab |
Discontinue tocilizumab |
|
ANC (cells/mm3) |
Recommendation for RA and SSc-ILD |
Recommendation for GCA |
|---|---|---|
|
>1000 |
Maintain current dosage |
Maintain current dosage |
|
500–1000 |
Interrupt tocilizumab therapy |
Interrupt tocilizumab therapy |
|
When ANC >1000/mm3 in patients receiving IV tocilizumab, resume tocilizumab at a dose of 4 mg/kg and increase to 8 mg/kg as clinically indicated |
When ANC >1000/mm3 in patients receiving IV tocilizumab, resume tocilizumab at a dose of 6 mg/kg |
|
|
When ANC >1000/mm3 in patients receiving sub-Q tocilizumab, resume tocilizumab at every other week and increase frequency to every week as clinically indicated |
When ANC >1000/mm3 in patients receiving sub-Q tocilizumab, resume tocilizumab at every other week and increase frequency to every week as clinically indicated |
|
|
<500 |
Discontinue tocilizumab |
Discontinue tocilizumab |
|
Platelet Count (cells/mm3) |
Recommendation for RA and SSc-ILD |
Recommendation for GCA |
|---|---|---|
|
50,000–100,000 |
Interrupt tocilizumab therapy |
Interrupt tocilizumab therapy |
|
When platelet count >100,000/mm3 in patients receiving IV tocilizumab, resume tocilizumab at a dose of 4 mg/kg and increase to 8 mg/kg as clinically indicated |
When platelet count >100,000/mm3 in patients receiving IV tocilizumab, resume tocilizumab at a dose of 6 mg/kg |
|
|
When platelet count >100,000/mm3 in patients receiving sub-Q tocilizumab, resume tocilizumab at every other week and increase frequency to every week as clinically appropriate |
When platelet count >100,000/mm3 in patients receiving sub-Q tocilizumab, resume tocilizumab at every other week and increase frequency to every week as clinically appropriate |
|
|
<50,000 |
Discontinue tocilizumab |
Discontinue tocilizumab |
Special Populations
Hepatic Impairment
Use is not recommended in patients with active hepatic disease or hepatic impairment.
Renal Impairment
Dosage adjustment not necessary in patients with mild or moderate renal impairment; not evaluated in severe renal impairment.
Geriatric Patients
Manufacturer makes no specific dosage recommendations.
Cautions for Tocilizumab
Contraindications
-
Known hypersensitivity to the drug.
Warnings/Precautions
Warnings
Infectious Complications
Increased risk for developing serious infections that may lead to hospitalization or death, particularly in patients taking concomitant immunosuppressants such as methotrexate or corticosteroids (see Boxed Warning).
Do not initiate tocilizumab in patients with active infections, including localized infections. Consider potential risks and benefits of the drug prior to initiating therapy in patients with a history of chronic, recurring, serious, or opportunistic infections; patients with underlying conditions that may predispose them to infections; and patients who have been exposed to tuberculosis or who have resided or traveled in regions where tuberculosis or mycoses are endemic. Information regarding the use of tocilizumab in patients with COVID-19 and concomitant active serious infections is limited; consider the risks and benefits of treatment in COVID-19 patients with other concurrent infections.
Closely monitor patients during and after treatment with tocilizumab for the development of signs or symptoms of infection. If new infection occurs during therapy, perform thorough diagnostic evaluation (appropriate for immunocompromised patient), initiate appropriate anti-infective therapy, and closely monitor patient. If serious infection, opportunistic infection, or sepsis develops, discontinue tocilizumab until the infection is controlled.
Evaluate patients, except for those with COVID-19, for latent tuberculosis and for risk factors for tuberculosis prior to and periodically during therapy. When indicated, initiate an appropriate antimycobacterial regimen for the treatment of latent tuberculosis infection prior to tocilizumab therapy. Consider initiation of antimycobacterial therapy prior to initiation of tocilizumab in individuals with a history of latent or active tuberculosis in whom an adequate course of antimycobacterial treatment cannot be confirmed and in individuals with a negative test for latent tuberculosis who have risk factors for tuberculosis. Consultation with a tuberculosis specialist is recommended when deciding whether to initiate antimycobacterial therapy.
Monitor all patients, including those with a negative test for latent tuberculosis, for active tuberculosis.
Viral reactivation can occur in patients receiving immunosuppressive therapies. Herpes zoster exacerbation reported in patients receiving tocilizumab. No cases of hepatitis B reaction reported in clinical studies.
Other Warnings/Precautions
GI Perforation
GI perforation reported in clinical trials, usually as a complication of diverticulitis.
Caution is advised if tocilizumab is used in patients at risk for GI perforation.
Promptly evaluate patients with new-onset abdominal symptoms for evidence of GI perforation.
Hepatotoxicity
Serious hepatic injury observed in patients receiving IV or sub-Q tocilizumab; some cases resulted in a liver transplant or death. Onset of hepatotoxicity occurred months to years following initiation of therapy. Although most cases presented with marked elevations of aminotransferases (>5 times the ULN), some cases presented with signs or symptoms of liver dysfunction and only mildly elevated aminotransferases. During controlled clinical trials, tocilizumab was associated with a higher incidence of aminotransferase elevations than placebo. Increased frequency and magnitude of aminotransferase elevations observed when potentially hepatotoxic drugs (e.g., methotrexate) were used concurrently.
In adults with rheumatoid arthritis, GCA, or SSc-ILD, perform liver function tests (i.e., serum ALT and AST, alkaline phosphatase, and total bilirubin concentrations) prior to initiation of therapy, then every 4–8 weeks during therapy for the first 6 months and every 3 months thereafter. Do not initiate therapy in rheumatoid arthritis, GCA, or SSc-ILD patients with aminotransferases >1.5 times the ULN. In patients with ALT or AST >5 times the ULN, discontinue tocilizumab.
A similar pattern of serum aminotransferase elevations was observed in tocilizumab-treated patients with polyarticular or systemic JIA. Monitor liver function tests at the time of the second infusion and every 4–8 weeks thereafter in patients with polyarticular JIA and at the time of the second infusion and every 2–4 weeks thereafter in patients with systemic JIA.
In patients hospitalized with COVID-19, perform liver function tests (i.e., serum ALT and AST) before initiating tocilizumab therapy and during treatment. The manufacturer recommends tocilizumab therapy should not be initiated in COVID-19 patients with elevated ALT or AST above 10 times the ULN. Multi-organ failure with involvement of the liver is recognized as a complication of severe COVID-19. The decision to administer tocilizumab should balance the potential benefit of treating COVID-19 against the potential risks of acute treatment with tocilizumab.
In patients with symptoms indicative of possible liver injury (e.g., fatigue, anorexia, right upper abdominal discomfort, dark urine, jaundice), perform liver function tests promptly. If liver function tests are abnormal (e.g., ALT >3 times the ULN, total bilirubin >2 times the ULN), interrupt therapy and evaluate patient to determine the probable cause. Do not reinitiate therapy unless another explanation for the liver function test abnormalities is found and values have returned to normal.
Hematologic Effects
Possible neutropenia or thrombocytopenia.
Reduction in neutrophil count to <1000/mm3 reported in patients receiving tocilizumab. Infections infrequently reported in association with treatment-related neutropenia in long-term extension studies and postmarketing clinical experience.
In clinical trials, decreases in platelet counts were not associated with severe bleeding.
Do not start in RA, GCA, and SSc-ILD patients with ANC less than 2000/mm3. Discontinue in patients who develop an absolute neutrophil count less than 500/mm3. Monitor neutrophil and platelet counts 4–8 weeks after initiation of therapy and every 3 months thereafter in adults with rheumatoid arthritis, GCA, or SSc-ILD.
Monitor neutrophil and platelet counts at the time of the second tocilizumab administration and every 4–8 weeks thereafter in patients with polyarticular JIA, and at the time of the second administration and every 2–4 weeks thereafter in patients with systemic JIA.
It is not recommended to initiate tocilizumab treatment in COVID-19 patients with an absolute neutrophil count less than 1000 per mm3 or a platelet count less than 50,000 per mm3. Neutrophil and platelet counts should be monitored.
Dosage adjustment, treatment interruption, or discontinuance may be necessary in patients with neutropenia or thrombocytopenia.
Effects on Serum Lipids
Increased serum concentrations of total cholesterol, triglycerides, LDL-cholesterol, and/or HDL-cholesterol reported.
Monitor lipoprotein concentrations approximately 4–8 weeks after initiation of tocilizumab therapy in adults with rheumatoid arthritis, GCA, SSc-ILD or patients with polyarticular or systemic JIA.
Manage lipid disorders as clinically appropriate.
Malignancies
Immunosuppressive therapy may increase the risk of malignancies. Whether treatment with tocilizumab affects development of malignancies remains to be determined. Malignancies were reported in clinical trials.
Sensitivity Reactions
Serious hypersensitivity reactions, including fatal anaphylaxis in patients receiving IV infusions of tocilizumab, reported. Tocilizumab is contraindicated in patients with known hypersensitivity to the drug.
Hypersensitivity reactions requiring treatment discontinuance (e.g., anaphylaxis, generalized erythema, rash, urticaria) reported during clinical trials in various patient populations and with either IV or sub-Q therapy. Hypersensitivity reactions, including anaphylaxis and death, reported during postmarketing experience in patients receiving various IV dosages (with or without concomitant therapy), including in patients who received premedication. Hypersensitivity reactions, including anaphylaxis, have occurred both with and without prior hypersensitivity reactions and as early as the first IV infusion. Serious cutaneous reactions, including DRESS, reported in patients with autoinflammatory conditions treated with tocilizumab.
Have appropriate agents and equipment available for immediate use in case a serious hypersensitivity reaction occurs during IV tocilizumab infusion. Patients receiving sub-Q therapy should seek immediate medical attention if they experience symptoms of a hypersensitivity reaction.
If a hypersensitivity reaction occurs, immediately stop administration and permanently discontinue the drug; treat the reaction promptly and monitor the patient until resolution of signs and symptoms.
Demyelinating Disorders
Effect of tocilizumab on demyelinating disorders remains to be determined. Multiple sclerosis and chronic inflammatory demyelinating polyneuropathy reported rarely in patients with rheumatoid arthritis receiving tocilizumab.
Monitor patients receiving tocilizumab for signs and symptoms suggestive of a demyelinating disorder. Exercise caution when considering tocilizumab therapy in patients with preexisting or recent-onset demyelinating disorders.
Immunization
Do not administer live vaccines to patients receiving tocilizumab. Bring vaccinations up to date prior to initiation of tocilizumab therapy.
Immunogenicity
Antibodies to tocilizumab, including neutralizing antibodies, may develop; some patients with antibody development have experienced hypersensitivity reactions resulting in treatment discontinuance. Antibody detection rates appear similar with IV or sub-Q administration.
Specific Populations
Pregnancy
Clinical data in pregnant women not sufficient to determine whether there is a drug-associated risk for major birth defects and miscarriage.
Animal data suggest risk of fetal harm.
Inhibition of IL-6 signaling may interfere with cervical ripening and dilatation and myometrial contractile activity, which could potentially result in parturition delays.
As pregnancy progresses, monoclonal antibodies are increasingly transported across the placenta, with the largest amount transferred during the third trimester. Infants exposed to tocilizumab in utero may have impaired immune responses.
Safety of administering live vaccines to infants exposed to tocilizumab in utero is unknown; consider risks and benefits.
Lactation
Not known whether tocilizumab is distributed into milk; effects of the drug on the breast-fed infant and on milk production also not known.
IgG distributes into human milk. If tocilizumab distributes into human milk, effects of local GI tract exposure and potential limited systemic exposure in the infant are unknown. Risk to nursing infants not known.
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for tocilizumab and any potential adverse effects on the breast-fed child from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy of IV and sub-Q tocilizumab for management of active polyarticular or systemic JIA and of IV tocilizumab for management of severe or life-threatening CAR T cell-induced CRS established in pediatric patients ≥2 years of age. Safety and efficacy not established in children <2 years of age or for the management of conditions other than polyarticular or systemic JIA and CAR T cell-induced CRS in children.
Geriatric Use
In clinical trials of tocilizumab in rheumatoid arthritis, serious infections reported more frequently in patients ≥65 years of age than in younger adults. Geriatric patients in general may have a higher incidence of infections than younger adults. Use tocilizumab with caution in this age group.
Insufficient experience with tocilizumab in patients ≥65 years of age with CAR T cell-induced CRS to determine whether they respond differently than younger adults.
Clinical studies that evaluated tocilizumab for COVID-19 noted no overall differences in efficacy or safety between patients ≥65 years of age and those <65 years of age.
Hepatic Impairment
Safety and efficacy not established in patients with hepatic impairment, including those with serologic evidence of HBV or HCV infection. Use in patients with active hepatic disease or hepatic impairment is not recommended.
Renal Impairment
Mild renal impairment (Clcr 50–79 mL/minute) does not appear to affect pharmacokinetics. Dosage adjustment not necessary in patients with mild or moderate renal impairment. About one-third of the patients in the GCA trial had moderate renal impairment at baseline (creatinine clearance 30-59 mL/min), but no impact on exposure was noted in these patients. Not evaluated in patients with severe renal impairment.
Common Adverse Effects
Adverse effects reported in ≥5% of patients: upper respiratory tract infection, nasopharyngitis, headache, hypertension, increased ALT concentrations, injection site reactions.
Drug Interactions
May alter expression of CYP isoenzymes including 1A2, 2B6, 2C9, 2C19, 2D6, and 3A4; effects on CYP2C8 or transporters (e.g., P-glycoprotein) not elucidated.
Drugs Metabolized by Hepatic Microsomal Enzymes
Possible increased metabolism of drugs metabolized by CYP isoenzymes. Because IL-6 may down-regulate CYP isoenzymes, inhibition of IL-6 by tocilizumab in rheumatoid arthritis patients may restore CYP enzyme activity to higher levels. Effects on CYP enzyme activity may persist for several weeks after drug discontinuance.
Drugs metabolized by CYP isoenzymes that have a low therapeutic index and require individualized dosing: Carefully monitor therapeutic effect and serum concentrations following initiation or discontinuance of tocilizumab; adjust dosage as needed.
Other CYP3A4 substrates: Caution advised when a reduction in efficacy would be undesirable.
Vaccines
Avoid live vaccines.
Information not available regarding immune response to vaccines in patients receiving tocilizumab or regarding secondary transmission of infection from individuals receiving live vaccines to patients receiving tocilizumab.
Inhibition of IL-6 may interfere with normal immune response to new antigens; all patients (particularly pediatric and geriatric patients) should receive all appropriate vaccines recommended by current immunization guidelines prior to initiation of tocilizumab therapy, if possible. Consult current vaccination guidelines regarding interval between administration of live vaccines and initiation of immunosuppressive (e.g., tocilizumab) therapy.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Contraceptives, oral |
Possible increased metabolism of oral contraceptive |
Caution advised |
|
Corticosteroids |
Concomitant use does not appear to affect clearance of tocilizumab |
|
|
Cyclosporine |
Possible increased metabolism of cyclosporine |
Carefully monitor therapeutic effect and serum concentrations of cyclosporine following initiation or discontinuance of tocilizumab; adjust dosage as needed |
|
Dextromethorphan |
Reduction in exposure to dextromethorphan and dextrorphan following initiation of IV tocilizumab reported in rheumatoid arthritis patients receiving dextromethorphan (In rheumatoid arthritis patients not receiving tocilizumab, systemic exposure to dextromethorphan is similar to, but exposure to dextrorphan is decreased, compared with values in healthy individuals ) |
|
|
DMARDs, biologic (e.g., TNF blocking agents) |
Possible increased immunosuppression and increased risk of infection; concomitant use not studied |
Concomitant use not recommended |
|
HMG CoA reductase inhibitors (statins) |
Statins metabolized by CYP isoenzymes (e.g., atorvastatin, lovastatin): Possible increased metabolism of the statin Simvastatin: Reduction in exposure to simvastatin and simvastatin acid following initiation of tocilizumab reported in rheumatoid arthritis patients receiving simvastatin (values were similar to or slightly higher than values observed after simvastatin administration in healthy individuals); exposure to simvastatin and simvastatin acid increased following discontinuance of tocilizumab (Systemic exposure to simvastatin and simvastatin acid is increased in rheumatoid arthritis patients not receiving tocilizumab compared with healthy individuals) |
Caution advised When selecting simvastatin dosages for patients with rheumatoid arthritis, consider the potential for altered systemic exposure to the drug following initiation or discontinuance of tocilizumab |
|
Methotrexate |
Concomitant use does not appear to affect clearance of tocilizumab or exposure to methotrexate Possible increased risk of hepatotoxicity |
|
|
NSAIAs |
Concomitant use does not appear to affect clearance of tocilizumab |
|
|
Omeprazole |
Reduction in exposure to omeprazole following initiation of IV tocilizumab reported in rheumatoid arthritis patients receiving omeprazole (values were slightly higher than values observed after omeprazole administration in healthy individuals) (Systemic exposure to omeprazole is increased in rheumatoid arthritis patients not receiving tocilizumab compared with healthy individuals ) |
|
|
Theophylline |
Possible increased metabolism of theophylline |
Carefully monitor therapeutic effect and serum concentrations of theophylline following initiation or discontinuance of tocilizumab; adjust dosage as needed |
|
Warfarin |
Possible increased metabolism of warfarin |
Carefully monitor therapeutic effect of warfarin following initiation or discontinuance of tocilizumab; adjust dosage as needed |
Tocilizumab Pharmacokinetics
Absorption
Bioavailability
Following sub-Q injection in rheumatoid arthritis and GCA patients, bioavailability is 80%.
Following sub-Q injection in polyarticular and systemic JIA patients, bioavailability is 96 and 95%, respectively.
Plasma Concentrations
Increase in IV dosage from 4 mg/kg to 8 mg/kg every 4 weeks associated with proportional increases in peak plasma concentrations and greater-than-proportional increases in exposure and trough plasma concentrations.
Special Populations
At fixed sub-Q dosage, tocilizumab exposure is inversely related to body weight.
Following IV dose of 8 mg/kg, systemic drug exposure is substantially greater (86%) in individuals weighing >100 kg than in those weighing <60 kg, since linear clearance increases as body size increases.
Distribution
Extent
Not known whether tocilizumab is distributed into milk.
Crosses the placenta.
Elimination
Half-life
Adults with rheumatoid arthritis: Up to 11 days at IV dosage of 4 mg/kg every 4 weeks; up to 13 days at IV dosage of 8 mg/kg every 4 weeks or sub-Q dosage of 162 mg every week; up to 5 days after sub-Q dosage of 162 mg every other week.
Adults with GCA: 18.3–18.9 days at sub-Q dosage of 162 mg once weekly, 4.2–7.9 days at sub-Q dosage of 162 mg every other week and 13.2 days at IV dosage of 6 mg/kg every 4 weeks.
Pediatric patients with polyarticular JIA: ≤17 and ≤10 days following IV and sub-Q administration, respectively.
Pediatric patients with systemic JIA: ≤16 and ≤14 days following IV and sub-Q administration, respectively.
Eliminated by a combination of linear and nonlinear elimination. Clearance decreases as dose increases. At low tocilizumab concentrations, concentration-dependent nonlinear clearance plays a major role in determining total drug clearance; at higher concentrations, nonlinear pathway is saturated and clearance is determined mainly by linear clearance.
Special Populations
Steady-state pharmacokinetics in systemic JIA patients <2 years of age are similar to those in systemic JIA patients 2–17 years of age.
As body size increases, linear clearance increases. Following a weight-based IV dose of 8 mg/kg, systemic drug exposure is substantially greater in individuals weighing >100 kg than in those weighing <60 kg.
Pharmacokinetics not formally studied in renal or hepatic impairment. Population pharmacokinetic data indicate that mild renal impairment (Clcr ≥50 mL/minute but <80 mL/minute) does not alter pharmacokinetics. Pharmacokinetics not evaluated in patients with severe renal impairment.
Population pharmacokinetic analyses in adult rheumatoid arthritis and GCA patients indicate that age, gender, and race do not affect pharmacokinetics.
Stability
Storage
Parenteral
Injection (for Sub-Q Use)
Tocilizumab and tocilizumab-aazg: 2–8°C; do not freeze. Keep prefilled syringes and autoinjectors dry and store in original carton to protect from light. The prefilled syringe and autoinjector can be stored up to 2 weeks at or below 30°C for tocilizumab or at or below 25°C for tocilizumab-aazg after removal from the refrigerator.
Injection Concentrate (for IV Use)
2–8°C; do not freeze. Store vials in original carton to protect from light.
Following dilution with sodium chloride 0.9%, may store at 2–8°C for up to 24 hours or at room temperature for up to 24 hours (tocilizumab), up to 4 hours (tocilizumab-aazg), or up to 12 hours (tocilizumab-bavi). Protect from light.
Following dilution with sodium chloride 0.45%, may store tocilizumab and tocilizumab-aazg at 2–8°C for up to 24 hours or room temperature for up to 4 hours. Protect from light.
Actions
-
Binds to both soluble and membrane-bound IL-6 receptors and inhibits IL-6-mediated signaling through these receptors, thereby resulting in a reduction in inflammatory mediator production.
-
IL-6, a pleiotropic proinflammatory cytokine, is produced by various cell types (e.g., T-cells, B-lymphocytes, monocytes, fibroblasts, synoviocytes, endothelial cells) and has a broad spectrum of biologic activities, including involvement in T-cell activation, induction of immunoglobulin secretion, initiation of hepatic acute phase protein synthesis, stimulation of hematopoietic precursor cell proliferation and differentiation, and induction of osteoclast differentiation and activation.
-
IL-6 is overexpressed in synovial tissue in patients with rheumatoid arthritis and is thought to contribute to synovial proliferation and joint destruction in patients with the disease. Elevated levels of IL-6 in serum and synovial fluid correlate with clinical and laboratory measures of disease activity in patients with rheumatoid arthritis.
-
IL-6 is elevated in serum and synovial fluid in patients with polyarticular or systemic JIA; elevated IL-6 levels correlate with disease activity.
-
Specificity for the IL-6 receptor may help to relieve symptoms of cytokine release syndrome (CRS; e.g., fever, organ failure, death) in severely ill patients with COVID-19.
Advice to Patients
-
Advise patients and/or caregivers about potential benefits and risks of tocilizumab products. Advise patients and/or caregivers to read the medication guide.
-
Instruct the patient and/or caregiver regarding proper dosage and administration of tocilizumab products, including the use of aseptic technique, and proper disposal of prefilled syringes and autoinjectors if it is determined that the patient and/or caregiver is competent to safely administer subcutaneous injections of the drug.
-
Inform patients to consult clinician if the subcutaneous injection does not deliver the full dose.
-
Risk of increased susceptibility to infection. Instruct patients to inform their clinician immediately if any signs or symptoms suggestive of infection (e.g., fever or chills; sweating; cough; dyspnea; fatigue; diarrhea; burning or pain upon urination; warm, red, or painful skin) develop to assure rapid evaluation and appropriate treatment.
-
Risk of GI perforation. Instruct patients to inform their clinician immediately if severe, persistent abdominal pain occurs.
-
Risk of liver injury. Inform patients to notify their clinician if they develop right-sided abdominal swelling or pain, fatigue, lack of appetite for several days, yellowing of the skin or whites of the eyes, light-colored stools, weakness, nausea and vomiting, confusion, or dark colored urine.
-
Risk of hypersensitivity and serious allergic reactions, including anaphylaxis. Instruct patient to contact their clinician prior to administering the next dose if manifestations of an allergic reaction (e.g., urticaria, rash, flushing) occur; stress importance of seeking immediate medical attention if manifestations of a serious allergic reaction (e.g., difficulty breathing, chest pain, feelings of faintness or dizziness, abdominal pain or vomiting, swelling of the lips, tongue, or face) occur.
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription (e.g., biologic antirheumatic drugs, immunizations) and OTC drugs, vitamins, and herbal supplements, as well as any concomitant illnesses or any history of tuberculosis or other chronic or recurring infections.
-
Advise patients of periodic laboratory monitoring.
-
Advise patients to inform their clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Tocilizumab is obtained through designated specialty pharmacies. Contact manufacturer for specific availability information.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
162 mg/0.9 mL |
Actemra (available as single-use prefilled syringe) |
Genentech |
|
162 mg/0.9 mL |
Actemra ACTPen (available as single-use prefilled autoinjector) |
Genentech |
||
|
Injection concentrate, for IV infusion |
20 mg/mL (80 mg, 200 mg, 400 mg) |
Actemra |
Genentech |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection, for subcutaneous use |
162 mg/0.9 mL |
Tyenne (available as single-dose prefilled syringe or prefilled autoinjector) |
|
|
Injection concentrate, for IV infusion |
20 mg/mL (80 mg, 200 mg, 400 mg) |
Tyenne |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
Injection concentrate, for IV infusion |
20 mg/mL (80 mg, 200 mg, 400 mg) |
Tofidence |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions December 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Biological Products Related to tocilizumab
Find detailed information on biosimilars for this medication.
Frequently asked questions
- What are the new drugs for rheumatoid arthritis (RA)?
- What is Actemra used to treat?
- What biosimilars have been approved in the United States?
- Is tocilizumab (Actemra) effective for treating COVID-19?
More about tocilizumab
- Check interactions
- Compare alternatives
- Reviews (58)
- Side effects
- Dosage information
- During pregnancy
- Drug class: interleukin inhibitors
- Breastfeeding
- En español
Patient resources
Professional resources
Other brands
Actemra, Tyenne, Avtozma, Tofidence