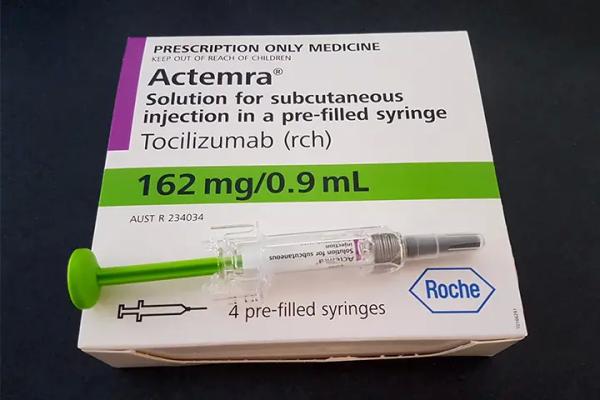
Tocilizumab (Intravenous, Subcutaneous)
Generic name: tocilizumab [ toe-si-LIZ-oo-mab ]
Brand names: Actemra, Tofidence
Drug class: Interleukin inhibitors
Medically reviewed by Drugs.com. Last updated on Jul 6, 2025.
Risk Of Serious Infections
Patients treated with tocilizumab products including tocilizumab-bavi are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids.
If a serious infection develops, interrupt tocilizumab-bavi until the infection is controlled.
Reported infections include: 1. Active tuberculosis, which may present with pulmonary or extrapulmonary disease. Patients should be tested for latent tuberculosis before tocilizumab-bavi use and during therapy. Treatment for latent infection should be initiated prior to tocilizumab-bavi use. 2. Invasive fungal infections, including candidiasis, aspergillosis, and pneumocystosis. Patients with invasive fungal infections may present with disseminated, rather than localized, disease. 3. Bacterial, viral and other infections due to opportunistic pathogens.
The risks and benefits of treatment with tocilizumab-bavi should be carefully considered prior to initiating therapy in patients with chronic or recurrent infection.
Patients should be closely monitored for the development of signs and symptoms of infection during and after treatment with tocilizumab-bavi, including the possible development of tuberculosis in patients who tested negative for latent tuberculosis infection prior to initiating therapy .
Uses for tocilizumab
Tocilizumab injection is used alone or together with other medicines to reduce the signs and symptoms of moderate to severe active rheumatoid arthritis. This medicine helps keep joint damage from getting worse after other medicines (eg, adalimumab, etanercept, infliximab) have been used and did not work well. It is a monoclonal antibody.
Tocilizumab injection is also used alone or together with glucocorticoids (steroid medicine) to treat giant cell arteritis (inflammation of the arteries). It can be used alone after stopping treatment with glucocorticoids.
Tocilizumab injection is also used to slow the rate of decline in lung function in patients with systemic sclerosis-associated interstitial lung disease (SSc-ILD).
Tocilizumab injection is also used alone or together with methotrexate to treat polyarticular juvenile idiopathic arthritis (PJIA) and systemic juvenile idiopathic arthritis (SJIA) in children 2 years of age and older. It is also used to treat severe or life-threatening cytokine release syndrome (CRS) in adults and children 2 years of age and older.
Tocilizumab injection is also used to treat coronavirus disease 2019 (COVID-19) in hospitalized patients who are receiving systemic corticosteroids and requiring supplemental oxygen and mechanical ventilation.
This medicine is available only with your doctor's prescription.
Before using tocilizumab
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Appropriate studies performed to date have not demonstrated pediatric-specific problems that would limit the usefulness of tocilizumab injection in children 2 years of age and older with PJIA, SJIA, and CRS. However, safety and efficacy have not been established for other conditions and in children younger than 2 years of age with PJIA, SJIA, and CRS.
Geriatric
Appropriate studies performed to date have not demonstrated geriatric-specific problems that would limit the usefulness of tocilizumab injection in the elderly. However, elderly patients are more likely to have serious infections, which may require caution in patients receiving tocilizumab injection.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abatacept
- Abemaciclib
- Acalabrutinib
- Adenovirus Vaccine, Live
- Alfentanil
- Alosetron
- Anifrolumab-fnia
- Aprepitant
- Astemizole
- Atazanavir
- Atomoxetine
- Atorvastatin
- Avanafil
- Avapritinib
- Axitinib
- Bacillus of Calmette and Guerin Vaccine, Live
- Baricitinib
- Bosutinib
- Brigatinib
- Budesonide
- Buspirone
- Caffeine
- Celecoxib
- Ceritinib
- Cholera Vaccine, Live
- Cisapride
- Clobazam
- Cobimetinib
- Codeine
- Colchicine
- Conivaptan
- Crizotinib
- Cyclosporine
- Daridorexant
- Darifenacin
- Darunavir
- Dasatinib
- Dengue Tetravalent Vaccine, Live
- Desipramine
- Dexlansoprazole
- Dextromethorphan
- Diazepam
- Dihydroergotamine
- Docetaxel
- Dofetilide
- Doxepin
- Dronedarone
- Duloxetine
- Ebola Zaire Vaccine, Live
- Eletriptan
- Eliglustat
- Elvitegravir
- Encainide
- Entrectinib
- Eplerenone
- Ergotamine
- Everolimus
- Felodipine
- Fentanyl
- Fezolinetant
- Finerenone
- Flecainide
- Flibanserin
- Fluticasone
- Fosaprepitant
- Fosphenytoin
- Gliclazide
- Glipizide
- Glyburide
- Hexobarbital
- Ibrexafungerp
- Ibrutinib
- Ibuprofen
- Indinavir
- Infliximab
- Influenza Virus Vaccine, Live
- Isavuconazonium Sulfate
- Ivabradine
- Ivacaftor
- Ivosidenib
- Lansoprazole
- Levomethadyl
- Lomitapide
- Lopinavir
- Lornoxicam
- Lovastatin
- Lurasidone
- Maraviroc
- Measles Virus Vaccine, Live
- Melatonin
- Meloxicam
- Mephobarbital
- Metoprolol
- Mexiletine
- Midazolam
- Midostaurin
- Mobocertinib
- Mumps Virus Vaccine, Live
- Naloxegol
- Nebivolol
- Neratinib
- Nilotinib
- Nisoldipine
- Olaparib
- Omeprazole
- Oxycodone
- Pantoprazole
- Paritaprevir
- Paroxetine
- Pazopanib
- Perphenazine
- Phenytoin
- Pimavanserin
- Pimozide
- Piroxicam
- Poliovirus Vaccine, Live
- Pomalidomide
- Proguanil
- Propafenone
- Quetiapine
- Quinidine
- Quinine
- Rabeprazole
- Ramelteon
- Ribociclib
- Risperidone
- Rotavirus Vaccine, Live
- Rubella Virus Vaccine, Live
- Ruxolitinib
- Selegiline
- Sildenafil
- Simvastatin
- Sirolimus
- Smallpox Monkeypox Vaccine, Live Non-Replicating
- Smallpox Vaccine
- Sonidegib
- Tacrine
- Tacrolimus
- Tamoxifen
- Tasimelteon
- Temsirolimus
- Theophylline
- Thioridazine
- Ticagrelor
- Tilidine
- Tipranavir
- Tizanidine
- Tolbutamide
- Tolterodine
- Tolvaptan
- Triazolam
- Trimipramine
- Typhoid Vaccine, Live
- Ubrogepant
- Ulipristal
- Vardenafil
- Varicella Virus Vaccine, Live
- Venetoclax
- Venlafaxine
- Voclosporin
- Yellow Fever Vaccine
- Yohimbine
- Zanubrutinib
- Zoster Vaccine, Live
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Chronic inflammatory demyelinating polyneuropathy (nerve problem) or
- Hyperlipidemia (high fats in the blood) or
- Liver disease, history of or
- Multiple sclerosis or
- Neutropenia (low level of white blood cells) or
- Stomach or bowel problems (eg, diverticulitis, perforations, ulcers) or
- Thrombocytopenia (low number of platelets) or
- Weak immune system (eg, HIV, cancer, or steroid use)—Use with caution. May make these conditions worse.
- Herpes zoster, history of or
- Tuberculosis, history of—Use with caution. May cause infections to come back (reactivate).
- Infections (eg, hepatitis B, bacteria, virus, fungus), active or recurring or
- Liver disease, active—Should not be used in patients with these conditions.
Proper use of tocilizumab
A nurse or other trained health professional will give you this medicine in a medical facility. It is given through a needle placed into one of your veins to treat rheumatoid arthritis, giant cell arteritis, PJIA, SJIA, or CRS. It must be given slowly, so the needle will have to remain in place for at least 1 hour.
Tocilizumab injection may also be given as a shot under your skin to treat rheumatoid arthritis, SSc-ILD, PJIA, SJIA, or giant cell arteritis. It may sometimes be given at home to patients who do not need to be in the hospital or clinic. If you are using this medicine at home, your doctor or nurse will teach you how to inject the medicine. Be sure that you understand exactly how to use this.
This medicine comes with a Medication Guide and patient instructions. Read and follow these instructions carefully. Ask your doctor or pharmacist if you have any questions.
This medicine is available in 2 forms. You may use a prefilled syringe or an autoinjector.
If you use this medicine at home, you will be shown the body areas where this shot can be given. Use a different body area each time you give yourself a shot. Keep track of where you give each shot to make sure you rotate body areas. This will help prevent skin problems. Do not inject into scars, moles, or skin areas that are red, bruised, tender, hard, or not intact.
Allow the prefilled syringe to warm to room temperature 30 minutes or the autoinjector for 45 minutes before using it. Do not warm it in any other way.
Check the liquid in the prefilled syringe or autoinjector. It should be clear and colorless or slightly yellow. Do not use it if it is cloudy, discolored, or has particles in it.
Use all of the medicine in each prefilled syringe or autoinjector. Use each prefilled syringe and autoinjector only one time. Do not save an open syringe or autoinjector.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
- For injection dosage form (prefilled syringe):
- For giant cell arteritis:
- Adults—162 milligrams (mg) injected under the skin once a week or once every other week. Your doctor may adjust your dose as needed and tolerated.
- Children—Use and dose must be determined by your doctor.
- For moderate to severe rheumatoid arthritis:
- Adults weighing 100 kilograms (kg) or more—162 milligrams (mg) injected under the skin once a week. Your doctor may adjust your dose as needed and tolerated.
- Adults weighing less than 100 kg—At first, 162 mg injected under the skin once every other week. Your doctor may increase the dose to 162 mg once a week as needed and tolerated.
- Children—Use and dose must be determined by your doctor.
- For systemic sclerosis-associated interstitial lung disease:
- Adults—162 milligrams (mg) injected under the skin once a week. Your doctor may adjust your dose as needed and tolerated.
- Children—Use and dose must be determined by your doctor.
- For polyarticular juvenile idiopathic arthritis:
- Adults and children 2 years of age and older weighing 30 kilograms (kg) or more—162 milligrams (mg) injected under the skin once every 2 weeks.
- Children 2 years of age and older weighing less than 30 kg—162 milligrams (mg) injected under the skin once every 3 weeks.
- Children younger than 2 years of age—Use and dose must be determined by your doctor.
- For systemic juvenile idiopathic arthritis:
- Adults and children 2 years of age and older weighing 30 kilograms (kg) or more—162 milligrams (mg) injected under the skin once a week.
- Children 2 years of age and older weighing less than 30 kg—162 milligrams (mg) injected under the skin once every 2 weeks.
- Children younger than 2 years of age—Use and dose must be determined by your doctor.
- For giant cell arteritis:
Missed Dose
If you miss a dose of this medicine, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Store in the refrigerator. Do not freeze.
Protect this medicine from direct light. Keep it in its original package until you are ready to use it.
Throw away used syringes in a hard, closed container where the needles cannot poke through. Keep this container away from children and pets.
Precautions while using tocilizumab
It is very important that your doctor check your or your child's progress at regular visits to make sure that this medicine is working properly. Blood and urine tests may be needed to check for unwanted effects.
You or your child will need to have a skin test for tuberculosis before you start using this medicine. Tell your doctor if you or anyone in your home has ever had a positive reaction to a tuberculosis skin test.
This medicine will lower the number of some types of blood cells in your body. Because of this, you may bleed or get infections more easily. To help with these problems, avoid being near people who are sick or have infections. Wash your hands often. Stay away from rough sports or other situations where you could be bruised, cut, or injured. Brush and floss your teeth gently. Be careful when using sharp objects, including razors and fingernail clippers. Tell your doctor if you have any kind of infection before you start using this medicine. Also tell your doctor if you have ever had an infection that would not go away or an infection that keeps coming back.
Call your doctor right away if you or your child start to have a cough that would not go away, weight loss, night sweats, fever, chills, or flu-like symptoms, such as a runny or stuffy nose, headache, blurred vision, or feeling generally ill. These may be signs that you have an infection.
This medicine may cause serious stomach and bowel problems, especially if you have a history of ulcers or diverticulosis. Check with your doctor right away if you or your child start having severe stomach cramps or pain, black, tarry stools, diarrhea, fever, or vomiting that is severe and sometimes bloody while being treated with this medicine.
Check with your doctor right away if you have pain or tenderness in the upper stomach, pale stools, dark urine, loss of appetite, nausea, vomiting, or yellow eyes or skin. These could be symptoms of a serious liver problem.
Using this medicine may increase your risk of having certain cancers. Talk to your doctor if you have unusual bleeding, bruising, or weakness, swollen lymph nodes in the neck, underarms, or groin, or unexplained weight loss. Also, check with your doctor right away if your skin has red, scaly patches, or raised bumps that are filled with pus.
Tocilizumab may cause headaches and skin reactions, such as a rash or itching, while you are receiving the injection or within 24 hours after you receive it. Check with your doctor or nurse right away if you or your child have any of these symptoms.
This medicine may cause serious types of allergic reactions, including anaphylaxis, which can be life-threatening and require immediate medical attention. Tell your doctor right away if you or your child have a rash, itching, hoarseness, trouble breathing, trouble swallowing, or any swelling of your hands, face, or mouth after using this medicine.
While you or your child are being treated with tocilizumab, and after you stop treatment with it, it is important to see your doctor about the immunizations (vaccinations) you should receive. Do not get any immunizations (vaccines) without your doctor's approval. Tocilizumab may lower your body's resistance, and there is a chance you might get the infection the vaccine is meant to prevent. In addition, you should not be around other persons living in your household who receive live virus vaccines because there is a chance that they could pass the virus on to you. Some examples of live vaccines include measles, mumps, influenza (nasal flu vaccine), poliovirus (oral form), rotavirus, and rubella. Do not get close to them and do not stay in the same room with them for very long. If you have questions about this, talk to your doctor.
This medicine may increase the amounts of cholesterol and fats in your blood. If this condition occurs, your doctor may give you some medicines that can lower their amounts. Talk to your doctor if you or your child have concerns.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Side Effects of tocilizumab
Along with its needed effects, a medicine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur:
More common
- Black, tarry stools
- bloody or cloudy urine
- blurred vision
- body aches or pain
- chest pain or tightness
- chills
- cough with or without mucus
- diarrhea
- difficult, burning, or painful urination
- difficulty breathing
- difficulty swallowing
- dizziness
- ear congestion
- fast heartbeat
- feeling of warmth
- fever
- frequent urge to urinate
- headache
- hives, itching, skin rash
- loss of appetite
- loss of consciousness
- loss of voice
- lower back or side pain
- nausea
- nervousness
- pain or tenderness around the eyes and cheekbones
- painful blisters on the trunk of the body
- pale skin
- pounding in the ears
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- redness of the face, neck, arms, and occasionally, upper chest
- slow or fast heartbeat
- sneezing
- sore throat
- stomach pain
- stuffy or runny nose
- sudden sweating
- ulcers, sores, or white spots in the mouth
- unusual bleeding or bruising
- unusual tiredness or weakness
Less common
- Accumulation of pus
- anxiety
- bladder pain
- burning feeling in the chest or stomach
- confusion
- dark urine
- decrease in height
- decreased urine
- difficulty moving
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- dry mouth
- fast, irregular, pounding, or racing heartbeat or pulse
- feeling hot
- general feeling of discomfort or illness
- heartburn
- increased thirst
- indigestion
- itching, pain, redness, swelling, tenderness, or warmth on the skin at the injection site
- joint pain
- light-colored stools
- loss of appetite
- mood changes
- muscle ache, pain, cramp, or stiffness
- numbness or tingling in the hands, feet, or lips
- pain in the back, ribs, arms, legs, groin, or genitals
- severe stomach pain
- sharp back pain just below the ribs
- shivering
- stomach upset
- sweating
- swollen joints
- swollen, painful, or tender lymph glands in the face, neck, armpit, or groin
- swollen, red, or tender area of infection
- tenderness in the stomach area
- trouble with sleeping
- unexplained runny nose or sneezing
- vomiting
- yellow eyes and skin
Rare
- Belching
- changes in skin color
- coughing or spitting up blood
- fainting
- gaseous stomach pain
- lightheadedness
- neck pain
- night sweats
- noisy breathing
- rapid, shallow breathing
- recurrent fever
- red, tender, or oozing skin at the wounded area
- sudden high fever or low-grade fever for months
- swelling of the foot or leg
- weight loss
Incidence not known
- Blistering, peeling, loosening of the skin
- bloating
- dilated neck veins
- pains in the stomach, side, or abdomen, possibly radiating to the back
- red skin lesions, often with a purple center
- red, irritated eyes
- severe stomach pain, cramping, or burning
- swelling of the face, fingers, feet, or lower legs
- vomiting of material that looks like coffee grounds, severe and continuous
- weight gain
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Burning, dry, or itching eyes
- constipation
- discharge, excessive tearing
- redness, pain, or swelling of the eye, eyelid, or inner lining of the eyelid
- skin rash, encrusted, scaly and oozing
- swelling or inflammation of the mouth
Less common
- Abnormal or decreased touch sensation
- bleeding or redness and swelling of the gums
- blemishes on the skin
- bloody eye
- chapped, red, or swollen lips
- earache
- feeling of constant movement of self or surroundings
- irritation in the mouth
- loose teeth
- persistent breath odor or bad taste in your mouth
- pimples
- redness or swelling in the ear
- scaling, redness, burning, pain, or other signs of inflammation on the lips
- sensation of spinning
- sore mouth or tongue
- white patches in the mouth or on the tongue
Rare
- Bleeding after passing stool
- blindness
- bloody nose
- burning, numbness, tingling, or painful sensations
- change in hearing
- continuing ringing or buzzing or other unexplained noise in the ears
- coughing or spitting up blood
- decreased vision or other changes in vision
- dry mouth
- ear drainage
- flushed, dry skin
- fruit-like breath odor
- hearing loss
- increased hunger, thirst, urination
- itching ears
- uncomfortable swelling around the anus
- unexplained weight loss
- unsteadiness or awkwardness
- weakness in the arms, hands, legs, or feet
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Commonly used brand name(s)
In the U.S.
- Actemra
- Tofidence
Available Dosage Forms:
- Solution
Therapeutic Class: Immunological Agent
Pharmacologic Class: Monoclonal Antibody
Biological Products Related to tocilizumab
Find detailed information on biosimilars for this medication.
Frequently asked questions
- What are the new drugs for rheumatoid arthritis (RA)?
- What is Actemra used to treat?
- What biosimilars have been approved in the United States?
- Is tocilizumab (Actemra) effective for treating COVID-19?
More about tocilizumab
- Check interactions
- Compare alternatives
- Reviews (58)
- Side effects
- Dosage information
- During pregnancy
- Drug class: interleukin inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Actemra, Tyenne, Avtozma, Tofidence
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.