Tocilizumab Dosage
Medically reviewed by Drugs.com. Last updated on Jul 23, 2024.
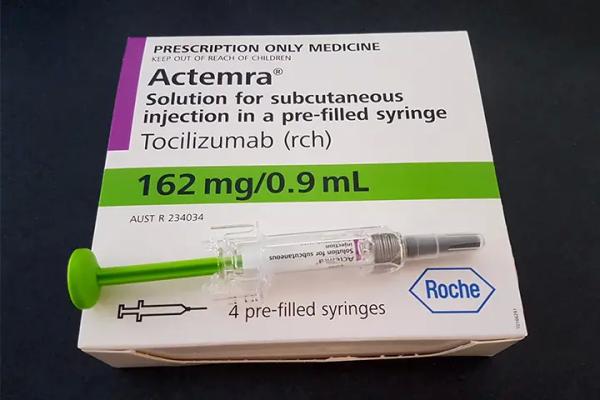
Applies to the following strengths: 20 mg/mL; 162 mg/0.9 mL; bavi 200 mg/10mL; bavi 400 mg/20mL; bavi 80 mg/4mL; aazg 162 mg/0.9 mL; aazg 20 mg/mL
Usual Adult Dose for:
- Rheumatoid Arthritis
- Giant Cell Arteritis
- Interstitial Lung Disease
- Cytokine-Associated Toxicity
- COVID-19
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Rheumatoid Arthritis
IV Infusion: 4 mg/kg IV every 4 weeks followed by an increase to 8 mg/kg IV every 4 weeks based on clinical response
Maximum dose: 800 mg per infusion
Subcutaneous Injection:
- Less than 100 kg: 162 mg subcutaneously every other week followed by an increase to once a week based on clinical response
- At least 100 kg: 162 mg subcutaneously once a week
Comments:
- This drug may be used as monotherapy or concomitantly with methotrexate or other nonbiologic disease-modifying antirheumatic drugs (DMARDs).
- When transitioning from IV infusion to subcutaneous injection, the first subcutaneous dose should be administered instead of the next scheduled IV dose.
- To manage certain dose-related laboratory changes (including elevated liver enzymes, neutropenia, thrombocytopenia):
- IV infusion: Dose should be reduced from 8 mg/kg to 4 mg/kg.
- Subcutaneous injection: Dose should be interrupted or frequency should be reduced from once a week to every other week dosing.
Use: For the treatment of patients with moderately to severely active rheumatoid arthritis (RA) who have had an inadequate response to 1 or more DMARDs
Usual Adult Dose for Giant Cell Arteritis
IV Infusion: 6 mg/kg IV every 4 weeks
Maximum dose: 600 mg per infusion
Subcutaneous Injection: 162 mg subcutaneously once a week
- Based on clinical considerations, 162 mg subcutaneously every other week may be prescribed.
Comments:
- This drug should be used in combination with a tapering course of glucocorticoids; it can be used alone after discontinuation of glucocorticoids.
- When transitioning from IV infusion to subcutaneous injection, the first subcutaneous dose should be administered instead of the next scheduled IV dose.
- To manage dose-related laboratory abnormalities (including elevated liver enzymes, neutropenia, thrombocytopenia):
- IV infusion: Dosing may need to be interrupted.
- Subcutaneous injection: Interruption of dose or reduction in frequency from once a week to every other week dosing may be needed.
Use: For the treatment of giant cell arteritis (GCA)
Usual Adult Dose for Interstitial Lung Disease
Subcutaneous Injection: 162 mg subcutaneously once a week
Comments:
- To manage dose-related laboratory abnormalities (including elevated liver enzymes, neutropenia, thrombocytopenia), dosing may need to be interrupted.
- Subcutaneous administration with the prefilled autoinjector has not been studied in systemic sclerosis-associated interstitial lung disease (SSc-ILD).
- IV administration is not approved for SSc-ILD.
Use: For slowing the rate of decline in pulmonary function in patients with SSc-ILD
Usual Adult Dose for Cytokine-Associated Toxicity
IV Infusion:
- Less than 30 kg: 12 mg/kg IV once
- At least 30 kg: 8 mg/kg IV once
Comments:
- This drug should be administered by IV infusion only; subcutaneous administration is not approved for CRS.
- This drug may be used alone or in combination with corticosteroids.
- If no clinical improvement in the signs/symptoms of cytokine release syndrome (CRS) occurs after the first dose, up to 3 additional doses may be administered. The interval between consecutive doses should be at least 8 hours.
Use: For the treatment of chimeric antigen receptor (CAR) T cell-induced severe or life-threatening CRS
Usual Adult Dose for COVID-19
IV Infusion: 8 mg/kg IV once
Maximum dose: 800 mg per infusion
Comments:
- This drug should be administered by IV infusion only; subcutaneous administration is not approved for coronavirus disease 2019 (COVID-19).
- If clinical signs/symptoms worsen or do not improve after the first dose, 1 additional infusion of this drug may be administered at least 8 hours after the initial infusion.
Use: For the treatment of COVID-19 in hospitalized patients who are receiving systemic corticosteroids and require supplemental oxygen, noninvasive or invasive mechanical ventilation, or extracorporeal membrane oxygenation (ECMO)
Usual Pediatric Dose for Juvenile Idiopathic Arthritis
2 YEARS OR OLDER:
Polyarticular Juvenile Idiopathic Arthritis (PJIA):
IV Infusion:
- Less than 30 kg: 10 mg/kg IV every 4 weeks
- At least 30 kg: 8 mg/kg IV every 4 weeks
Subcutaneous Injection:
- Less than 30 kg: 162 mg subcutaneously every 3 weeks
- At least 30 kg: 162 mg subcutaneously every 2 weeks
Systemic Juvenile Idiopathic Arthritis (SJIA):
IV Infusion:
- Less than 30 kg: 12 mg/kg IV every 2 weeks
- At least 30 kg: 8 mg/kg IV every 2 weeks
Subcutaneous Injection:
- Less than 30 kg: 162 mg subcutaneously every 2 weeks
- At least 30 kg: 162 mg subcutaneously once a week
Comments:
- This drug may be used as monotherapy or concomitantly with methotrexate.
- Because weight may fluctuate, dose should not be changed based solely on a single visit body weight measurement.
- When transitioning from IV infusion to subcutaneous injection, the first subcutaneous dose should be administered instead of the next scheduled IV dose.
- To manage dose-related laboratory abnormalities (including elevated liver enzymes, neutropenia, thrombocytopenia), dosing may need to be interrupted.
- Dose reduction has not been studied in this patient population.
- Dose should be interrupted for liver enzyme abnormalities, low neutrophil counts, and low platelet counts at levels similar to those for patients with RA and GCA. If appropriate, dosing of concomitant methotrexate and/or other medications should be modified or stopped.
- The decision to discontinue therapy for a laboratory abnormality should be based on the medical assessment of the individual patient.
Uses: For the treatment of active PJIA; for the treatment of active SJIA
Usual Pediatric Dose for Cytokine-Associated Toxicity
2 YEARS OR OLDER:
IV Infusion:
- Less than 30 kg: 12 mg/kg IV once
- At least 30 kg: 8 mg/kg IV once
Comments:
- This drug should be administered by IV infusion only; subcutaneous administration is not approved for CRS.
- This drug may be used alone or in combination with corticosteroids.
- If no clinical improvement in the signs/symptoms of CRS occurs after the first dose, up to 3 additional doses may be administered. The interval between consecutive doses should be at least 8 hours.
Use: For the treatment of CAR T cell-induced severe or life-threatening CRS
Usual Pediatric Dose for COVID-19
For investigational use only
2 YEARS OR OLDER:
IV Infusion:
- Less than 30 kg: 12 mg/kg IV once
- At least 30 kg: 8 mg/kg IV once
Comments:
- The US FDA issued an Emergency Use Authorization (EUA) to allow the emergency use of this drug for the treatment of COVID-19 in hospitalized pediatric patients (2 years or older) who are receiving systemic corticosteroids and require supplemental oxygen, noninvasive or invasive mechanical ventilation, or ECMO; this drug is not approved by the US FDA for use in pediatric patients with COVID-19.
- No adequate, approved, and available alternative is available for treatment of these patients. ClinicalTrials.gov should be consulted for information on clinical trials of this drug and other therapies for the treatment of COVID-19.
- If clinical signs/symptoms worsen or do not improve after the first dose, 1 additional infusion of this drug may be administered at least 8 hours after the initial infusion.
- Subcutaneous administration is not authorized for the treatment of COVID-19 patients.
- For additional information: https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization#coviddrugs.
Use: For the treatment of COVID-19 in hospitalized patients requiring supplemental oxygen, noninvasive or invasive mechanical ventilation, or ECMO
Renal Dose Adjustments
Mild to moderate renal dysfunction: No adjustment recommended
Severe renal dysfunction: Data not available
Comments:
- This drug has not been studied in patients with severe renal dysfunction.
Liver Dose Adjustments
Active liver disease or liver dysfunction: Not recommended.
If Liver Enzyme Abnormalities Develop During Therapy:
Greater than 1 to 3 times the upper limit of normal (1 to 3 x ULN):
- For RA and SSc-ILD: Dose of concomitant DMARDs should be modified, if appropriate. For persistent increases in this range:
- For patients receiving IV therapy, the dose should be reduced to 4 mg/kg or therapy should be held until ALT or AST levels have normalized.
- For patients receiving subcutaneous therapy, the injection frequency should be reduced to every other week or dosing should be held until ALT or AST levels have normalized; therapy should resume at every other week and frequency should be increased to once a week as clinically appropriate.
- For GCA: Dose of immunomodulatory agents should be modified, if appropriate. For persistent increases in this range:
- For patients receiving IV therapy, therapy should be held until ALT or AST levels have normalized.
- For patients receiving subcutaneous therapy, the injection frequency should be reduced to every other week or dosing should be held until ALT or AST levels have normalized; therapy should resume at every other week and frequency should be increased to once a week as clinically appropriate.
Greater than 3 to 5 x ULN (confirmed by repeat testing):
- For RA, SSc-ILD, and GCA:
- Dosing should be held until less than 3 x ULN and the recommendations for laboratory values greater than 1 to 3 x ULN should be followed.
- For persistent increases greater than 3 x ULN, this drug should be discontinued.
Greater than 5 x ULN:
- For RA, SSc-ILD, and GCA: This drug should be discontinued.
Comments:
- Safety and efficacy of this drug have not been studied in patients with liver dysfunction, including patients with positive HBV and HCV serology.
- Dose should be interrupted for liver enzyme abnormalities in patients with PJIA and SJIA at levels similar to those for patients with RA and GCA. If appropriate, dosing of concomitant methotrexate and/or other medications should be modified or stopped.
- In PJIA and SJIA, the decision to discontinue therapy for a liver enzyme abnormality should be based on the medical assessment of the individual patient.
Dose Adjustments
Serious Infections: Therapy should be held if a patient develops a serious infection until the infection is controlled.
Low Absolute Neutrophil Count (ANC):
ANC greater than 1000 cells/mm3:
- For RA, SSc-ILD, and GCA: Dose should be maintained.
ANC 500 to 1000 cells/mm3:
- For RA and SSc-ILD: Dosing should be held. When ANC greater than 1000 cells/mm3:
- For patients receiving IV therapy, dosing should resume at 4 mg/kg and increase to 8 mg/kg as clinically appropriate.
- For patients receiving subcutaneous therapy, dosing should resume at every other week and frequency should increase to once a week as clinically appropriate.
- For GCA: Dosing should be held. When ANC greater than 1000 cells/mm3:
- For patients receiving IV therapy, dosing should resume at 6 mg/kg.
- For patients receiving subcutaneous therapy, dosing should resume at every other week and frequency should increase to once a week as clinically appropriate.
ANC less than 500 cells/mm3:
- For RA, SSc-ILD, and GCA: This drug should be discontinued.
Low Platelet Count:
Platelet count 50,000 to 100,000 cells/mm3:
- For RA and SSc-ILD: Dosing should be held. When platelet count is greater than 100,000 cells/mm3:
- For patients receiving IV therapy, dosing should resume at 4 mg/kg and increase to 8 mg/kg as clinically appropriate.
- For patients receiving subcutaneous therapy, dosing should resume at every other week and frequency should increase to once a week as clinically appropriate.
- For GCA: Dosing should be held. When platelet count is greater than 100,000 cells/mm3:
- For patients receiving IV therapy, dosing should resume at 6 mg/kg.
- For patients receiving subcutaneous therapy, dosing should resume at every other week and frequency should increase to once a week as clinically appropriate.
Platelet count less than 50,000 cells/mm3:
- For RA, SSc-ILD, and GCA: This drug should be discontinued.
PJIA and SJIA:
- Dose should be interrupted for low neutrophil counts and low platelet counts in patients with PJIA and SJIA at levels similar to those for patients with RA and GCA. If appropriate, dosing of concomitant methotrexate and/or other medications should be modified or stopped.
- In PJIA and SJIA, the decision to discontinue therapy for a laboratory abnormality should be based on the medical assessment of the individual patient.
Precautions
US BOXED WARNING:
- RISK OF SERIOUS INFECTIONS: Patients treated with this drug are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants (e.g., methotrexate, corticosteroids). If a serious infection develops, therapy should be interrupted until the infection is controlled. Reported infections include: active tuberculosis (TB), which may present with pulmonary/extrapulmonary disease; invasive fungal infections (including candidiasis, aspergillosis, pneumocystosis); and bacterial, viral, and other infections (due to opportunistic pathogens). Patients (except for those with COVID-19) should be tested for latent TB before starting this drug and during therapy; if positive, treatment for latent infection should be started prior to therapy. Patients with invasive fungal infections may present with disseminated, rather than localized, disease. The risks and benefits of this drug should be carefully considered before starting therapy in patients with chronic/recurrent infection. Patients should be closely monitored for signs/symptoms of infection during and after therapy, including the possible development of TB in patients who tested negative for latent TB before starting therapy.
CONTRAINDICATIONS:
- Known hypersensitivity to the active component or any of the ingredients
Safety and efficacy in PJIA, SJIA, or CRS have not been established in patients younger than 2 years. Safety and efficacy have not been established in patients younger than 18 years with conditions other than PJIA, SJIA, or CRS.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Do not use this drug with biological DMARDs.
- Obtain and assess baseline CBC and liver function tests before therapy.
- RA, GCA, SSc-ILD, PJIA, and SJIA: This drug should not be started in patients with ANC below 2000 cells/mm3, platelet count below 100,000 cells/mm3, or ALT or AST above 1.5 x ULN.
- CRS: Patients with severe or life-threatening CRS often have cytopenias or elevated ALT or AST due to lymphodepleting chemotherapy or the CRS; the decision to use this drug should consider the potential benefit of treating the CRS vs the risks of short-term therapy with this drug.
- COVID-19: This drug should not be started in patients with ANC below 1000 cells/mm3, platelet count below 50,000 cells/mm3, or ALT or AST above 10 x ULN.
- This drug should only be infused by a health care professional with appropriate medical support to manage anaphylaxis.
- Allow the fully diluted solution to reach room temperature before infusion.
- Administer as a single IV drip infusion over 60 minutes with an infusion set; do not administer as an IV push or bolus.
- Do not infuse concomitantly in the same IV line with other drugs.
- Not intended for IV drip infusion
- Assess suitability of patient for home use; this drug should be used under the guidance of a health care practitioner.
- After proper training in technique, a patient may self-inject this drug or the patient's caregiver may administer this drug if determined appropriate by health care provider.
- Prior to injection, remove the prefilled syringe or autoinjector from the refrigerator and allow it to reach room temperature (prefilled syringe: 30 minutes; autoinjector: 45 minutes); do not warm any other way.
- Do not use prefilled syringes or autoinjectors showing particulate matter, cloudiness, or discoloration; do not use if any part of the prefilled syringe or autoinjector appears to be damaged.
- Rotate injection sites with each injection; never inject into moles, scars, or areas where skin is tender, bruised, red, hard, or not intact.
Storage requirements:
- Store refrigerated at 2C to 8C (36F to 46F); do not freeze.
- Store in the original container until time of use to protect from light; keep syringes and autoinjectors dry.
- Once removed from the refrigerator, can store the prefilled syringes and autoinjector up to 2 weeks at/below 30C (86F); always keep the prefilled syringes and autoinjector in the carton.
- Fully diluted solution for infusion: Protect from light; allow to reach room temperature before infusion.
- Diluted using 0.9% Sodium Chloride Injection, USP: May store at 2C to 8C (36F to 46F) or room temperature for up to 24 hours
- Diluted using 0.45% Sodium Chloride Injection, USP: May store at 2C to 8C (36F to 46F) for up to 24 hours or room temperature for up to 4 hours
Reconstitution/preparation techniques:
- The injection for IV infusion should be diluted by a health care professional.
- The manufacturer product information should be consulted.
IV compatibility:
- Compatible (undiluted injection): 0.9% or 0.45% Sodium Chloride Injection, USP
- Compatible (fully diluted solution): Polypropylene, polyethylene, and polyvinyl chloride infusion bags; polypropylene, polyethylene, and glass infusion bottles
General:
- This drug has not been studied in combination with biological DMARDs (e.g., tumor necrosis factor antagonists, interleukin-1 receptor antagonists, anti-CD20 monoclonal antibodies, selective costimulation modulators) due to the possibility of increased immunosuppression and increased risk of infection.
Monitoring:
- Hematologic: Neutrophils and platelet counts in patients with COVID-19 (according to current standard clinical practice); neutrophils and platelets in patients with RA, GCA, and SSc-ILD (4 to 8 weeks after start of therapy and every 3 months thereafter); neutrophils and platelets for PJIA (at second dose and thereafter every 4 to 8 weeks); neutrophils and platelets for SJIA (every 2 to 4 weeks)
- Hepatic: ALT and AST in patients with COVID-19 (according to current standard clinical practice); liver test panel including ALT and AST for PJIA (at second dose and thereafter every 4 to 8 weeks); liver test panel including ALT and AST for SJIA (every 2 to 4 weeks)
- Infections/Infestations: For signs/symptoms of infection (during and after therapy); for signs/symptoms of tuberculosis including in patients who tested negative for latent tuberculosis before starting therapy
- Metabolic: Lipid parameters in patients with RA, GCA, SSc-ILD, PJIA, and SJIA (about 4 to 8 weeks after start of therapy)
- Nervous System: For signs/symptoms of demyelinating disorders
Patient advice:
- Read the US FDA-approved patient labeling (Medication Guide and Instructions for Use).
- For COVID-19 treatment in pediatric patients (2 years or older): Read the Fact Sheet for Patients, Parents, and Caregivers.
- It is important to contact your doctor immediately when symptoms of infection or severe, persistent abdominal pain appear to assure rapid evaluation and appropriate treatment.
- Inform health care professional before administering the next dose if any symptoms of allergic reaction occur; seek immediate medical attention if symptoms of serious allergic reactions develop.
- If using the subcutaneous formulation: Inject the full amount in the syringe (0.9 mL) or full amount in the autoinjector (0.9 mL), which provides 162 mg of this drug, as directed in the Instructions for Use. Consult health care provider if the full dose is not received.
- Patients of childbearing potential: Notify prescriber of a known/suspected pregnancy.
Frequently asked questions
- What are the new drugs for rheumatoid arthritis (RA)?
- What is Actemra used to treat?
- What biosimilars have been approved in the United States?
- Is tocilizumab (Actemra) effective for treating COVID-19?
More about tocilizumab
- Check interactions
- Compare alternatives
- Reviews (58)
- Side effects
- During pregnancy
- Drug class: interleukin inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Actemra, Tyenne, Avtozma, Tofidence
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.