The originating document has been archived. We cannot confirm the completeness, accuracy, or currency of the content.
Osimertinib (Monograph)
Brand name: Tagrisso
Drug class: Antineoplastic Agents
Introduction
Antineoplastic agent; a third-generation inhibitor of receptor tyrosine kinases.
Uses for Osimertinib
Non-small Cell Lung Cancer (NSCLC)
Adjuvant treatment after tumor resection in patients with NSCLC harboring epidermal growth factor receptor (EGFR) exon 19 deletions (del19) or exon 21 (L858R) substitution mutations (as detected by an FDA-approved diagnostic test).
First-line treatment of metastatic NSCLC harboring EGFR exon 19 deletions (del19) or exon 21 (L858R) substitution mutations (as detected by an FDA-approved diagnostic test).
Treatment of metastatic NSCLC harboring EGFR T790M mutation (as detected by an FDA-approved diagnostic test) in patients who have experienced disease progression during or after EGFR tyrosine kinase inhibitor therapy.
Designated an orphan drug by FDA for treatment of EGFR mutation-positive NSCLC.
Osimertinib Dosage and Administration
General
Pretreatment Screening
-
Adjuvant therapy of NSCLC: Confirm presence of epidermal growth factor receptor (EGFR) exon 19 deletions (del19) or exon 21 (L858R) substitution mutations in tumor specimens using an FDA-approved companion diagnostic test (e.g., cobas EGFR Mutation Test).
-
First-line treatment of metastatic NSCLC: Confirm presence of EGFR del19 or L858R substitution mutations in tumor or plasma specimens using an FDA-approved diagnostic test (e.g., cobas EGFR Mutation Test). Patients with a negative plasma del19 or L858R mutation result should be reevaluated for feasibility of a tumor biopsy.
-
Previously treated metastatic NSCLC: Confirm presence of EGFR T790M mutation in tumor or plasma specimens by an FDA-approved diagnostic test (e.g., cobas EGFR Mutation Test). Because of the high rate of false-negative results, plasma testing is recommended only when a tumor biopsy cannot be obtained; patients with a negative plasma result should be reevaluated for feasibility of a tumor biopsy.
-
Baseline left ventricular ejection fraction (LVEF) in patients with cardiac risk factors.
-
Peform a CBC with differential before initiating therapy.
-
Verify pregnancy status in females of reproductive potential.
Patient Monitoring
-
Monitor for symptoms of interstitial lung disease and pneumonitis during therapy.
-
Monitor for corrected QT (QTc) interval prolongation in patients with congenital long QTc syndrome, congestive heart failure, or electrolyte abnormalities, and those receiving concomitant drugs known to prolong the QTc interval.
-
Periodic monitoring of electrolyte concentrations recommended in patients with congenital long QTc syndrome, congestive heart failure, or electrolyte abnormalities, and those receiving concomitant drugs known to prolong the QTc interval.
-
Patients with cardiac risk factors: Monitor for signs and symptoms of cardiomyopathy during therapy; assess LVEF in patients with cardiac risk factors at baseline and in those who develop signs or symptoms of cardiomyopathy during therapy.
-
Perform a CBC with differential periodically during therapy, and more frequently if clinically indicated.
Dispensing and Administration Precautions
-
Based on the Institute for Safe Medication Practices (ISMP), osimertinib is a high-alert medication that has a heightened risk of causing significant patient harm when used in error.
Administration
Oral Administration
Administer orally once daily without regard to meals; swallow tablets whole and do not crush.
For patients with difficulty swallowing solids, may disperse tablet in a container with 60 mL (2 ounces) of noncarbonated water (do not use other liquids); immediately swallow. To ensure full dose is administered, rinse container with an additional 120–240 mL of water and drink immediately. Do not crush, heat, or ultrasonicate tablet when preparing drug dispersion.
Alternatively, for administration through a nasogastric tube, disperse tablet in a container with 15 mL of noncarbonated water and draw dispersion into a syringe; rinse container with additional 15 mL of water to transfer any residue to the syringe. Administer the resulting 30-mL drug dispersion through the nasogastric tube, then flush tube with appropriate volumes of water (approximately 30 mL).
If a dose is missed, take next dose at regularly scheduled time; do not take missed dose.
Dosage
Available as osimertinib mesylate; dosage expressed in terms of osimertinib.
Adults
NSCLC
Adjuvant Treatment of NSCLC
Oral80 mg once daily. Continue therapy for up to 3 years or until disease recurrence or unacceptable toxicity occurs.
First-line Treatment of Metastatic NSCLC
Oral80 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Previously Treated Metastatic NSCLC
Oral80 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Dosage Modification
Interstitial Lung Disease/Pneumonitis
OralIf interstitial lung disease or pneumonitis occurs, permanently discontinue drug.
Cardiac Effects
OralIf QTc interval >500 msec on at least 2 separate ECGs, withhold therapy. If QTc interval improves to <481 msec or returns to baseline (if baseline QTc interval ≥481 msec), may resume therapy at reduced dosage of 40 mg daily.
If QTc-interval prolongation occurs concurrently with signs and/or symptoms of life-threatening arrhythmia, permanently discontinue drug.
If symptomatic congestive heart failure occurs, permanently discontinue drug.
Cutaneous Toxicity
OralIf Stevens-Johnson syndrome or erythema multiforme major is suspected, withhold osimertinib. Permanently discontinue osimertinib if diagnosis confirmed.
If cutaneous vasculitis is suspected, withhold osimertinib and evaluate patient for systemic involvement; consider consultation with a dermatologist. Consider permanent discontinuance based on severity when no other etiology is identified.
Other Toxicity
OralIf other grade 3 or higher adverse effects occur, withhold therapy for up to 3 weeks.
If adverse effect improves to grade 0–2, resume therapy at original dosage or reduced dosage (40 mg daily); if no improvement within 3 weeks, permanently discontinue drug.
Concomitant Use with CYP3A Inducers
OralIf used concomitantly with a potent CYP3A inducer, increase osimertinib dosage to 160 mg daily.
Special Populations
Hepatic Impairment
Mild to moderate hepatic impairment (Child-Pugh class A or B; total bilirubin concentration not exceeding ULN with AST concentration exceeding ULN; or total bilirubin concentration 1–3 times ULN with any AST concentration): No dosage adjustment needed.
Severe hepatic impairment: Insufficient data to provide dosage recommendations.
Renal Impairment
Mild to severe renal impairment (Clcr 15–89 mL/minute): No dosage adjustment needed.
End-stage renal disease: Insufficient data to provide dosage recommendations.
Geriatric Patients
No specific dosage recommendations.
Cautions for Osimertinib
Contraindications
-
Manufacturer states none known.
Warnings/Precautions
Interstitial Lung Disease/Pneumonitis
Severe or fatal interstitial lung disease or pneumonitis may occur.
Temporarily interrupt therapy and promptly evaluate patient if any respiratory manifestations suggestive of interstitial lung disease occur; permanently discontinue if a diagnosis is confirmed.
Prolongation of QT Interval
QTc-interval prolongation reported. Appears to occur in a concentration-dependent manner.
Periodically monitor ECG and serum electrolytes in patients with congenital long QT syndrome, congestive heart failure, or electrolyte abnormalities and in those receiving concomitant drugs known to prolong the QT interval with known risk of torsades de pointes.
If QT-interval prolongation occurs, dosage reduction, temporary interruption, or permanent discontinuance of therapy may be necessary.
Permanently discontinue if QTc-interval prolongation is accompanied by signs and/or symptoms of life-threatening arrhythmia.
Cardiomyopathy
Cardiomyopathy (e.g., acute or chronic cardiac failure, CHF, pulmonary edema, decreased ejection fraction) reported.
Assess cardiac function (including LVEF) in patients with cardiac risk factors prior to initiating therapy and periodically thereafter. Assess LVEF in any patient who develops cardiac complications during therapy.
Permanently discontinue in patients who develop symptomatic CHF.
Keratitis
Keratitis reported. If manifestations suggestive of keratitis (e.g., eye inflammation, lacrimation, photosensitivity, blurred vision, eye pain, red eye) occur, promptly refer patient to an ophthalmologist for evaluation.
Erythema Multiforme and Stevens-Johnson Syndrome
Erythema multiforme and Stevens-Johnson syndrome reported in postmarketing case reports.
Withhold osimertinib if erythema multiforme or Stevens-Johnson syndrome suspected; permanently discontinue if diagnosis confirmed.
Cutaneous Vasculitis
Cutaneous vasculitis (e.g., leukocytoclastic vasculitis, urticarial vasculitis, and IgA vasculitis) reported in postmarketing case reports.
Withhold osimertinib if cutaneous vasculitis suspected and evaluate for systemic involvement; consider consultation with a dermatologist. Consider permanently discontinuing osimertinib based on severity when no other etiology is identified.
Aplastic Anemia
Aplastic anemia reported; some cases resulted in fatal outcomes. Advise patients of signs and symptoms of aplastic anemia (e.g., new or persistent fevers, bruising, bleeding, pallor). If suspected, withhold osimertinib and obtain a hematology consultation. If diagnosis is confirmed, permanently discontinue osimertinib. Perform CBC with differential before initiating therapy, periodically throughout treatment, and more frequently if indicated.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm. Embryofetal toxicity (e.g., postimplantation loss and early embryonic death, decreased fetal weight) demonstrated in animals.
Verify pregnancy status prior to initiating therapy. Avoid pregnancy during therapy. Females of reproductive potential should use effective methods of contraception during therapy and for 6 weeks after drug discontinuance.
Males with female partners of reproductive potential should use effective methods of contraception during therapy and for 4 months after drug discontinuance.
Impairment of Fertility
Based on animal studies, may impair female and male fertility.
Specific Populations
Pregnancy
No available data in pregnant women; animal studies and the drug's mechanism of action suggest possible fetal harm. If used during pregnancy or if patient becomes pregnant during therapy, apprise of potential fetal hazard.
Lactation
Not known whether distributed into human milk or if drug has any effect on milk production or nursing infant. Discontinue nursing during therapy and for 2 weeks after drug is discontinued.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
No overall differences in efficacy based on age; however, a higher incidence of grade 3 or 4 adverse reactions and more frequent dosage modifications for adverse reactions observed in patients ≥65 years of age relative to younger adults.
Hepatic Impairment
Pharmacokinetics of osimertinib not altered by mild to moderate hepatic impairment (Child-Pugh class A or B; total bilirubin concentration not exceeding ULN with AST concentration exceeding ULN; or total bilirubin concentration 1–3 times ULN with any AST concentration).
Not studied in patients with severe (total bilirubin concentration 3–10 times ULN with any AST concentration) hepatic impairment.
Renal Impairment
Pharmacokinetics of osimertinib not altered by mild to severe renal impairment (Clcr 15–89 mL/minute).
Not studied in patients with end-stage renal disease (Clcr <15 mL/minute).
Common Adverse Effects
Adverse effects reported in >20% of patients: Diarrhea, rash, musculoskeletal pain, dry skin, nail toxicity, stomatitis, fatigue, cough. Laboratory abnormalities reported in ≥20% of patients: Leukopenia, lymphopenia, anemia, thrombocytopenia, neutropenia.
Drug Interactions
Metabolized principally by CYP3A. Substrate of P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP).
Induces CYP1A2. Does not inhibit CYP1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, or 2E1.
Inhibits BCRP, but does not inhibit organic anion transporter (OAT) 1 and OAT3, organic anion transporter polypeptide (OATP) 1B1 and OATP1B3, multidrug and toxin extrusion transporter (MATE) 1 and MATE2K, or organic cation transporter (OCT) 2.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP3A inducers: Possible pharmacokinetic interaction (decreased plasma osimertinib concentrations). Avoid concomitant use. If concomitant use cannot be avoided, increase osimertinib dosage to 160 mg daily; resume dosage of 80 mg daily 3 weeks after the potent CYP3A inducer is discontinued.
Drugs Transported by Breast Cancer Resistance Protein
Possible pharmacokinetic interaction (increased plasma concentrations of substrate). Monitor for adverse effects of BCRP substrate.
Drugs Affected by the P-gp Transport System
Possible pharmacokinetic interaction (increased plasma concentrations of substrate). Monitor for adverse effects of P-gp substrate.
Drugs that Prolong QT Interval
Potential pharmacologic interaction (additive effect on QT-interval prolongation). Avoid concomitant use. If concomitant use cannot be avoided, periodically monitor ECG and electrolytes. (See Prolongation of QT Interval under Cautions.)
Drugs Affecting Gastric Acidity
Clinically important pharmacokinetic interactions unlikely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Fexofenadine |
Increased peak concentrations and AUC of fexofenadine by 76 and 56%, respectively, following a single dose, and by 25 or 27%, respectively, at steady state |
Monitor for adverse effects of fexofenadine |
|
Itraconazole |
AUC of osimertinib increased by 24% and peak plasma concentrations decreased by 20%; not considered clinically important |
|
|
Omeprazole |
No substantial effect on osimertinib exposure |
|
|
Rifampin |
Decreased peak plasma concentrations and AUC of osimertinib by 73 and 78%, respectively |
If concomitant use cannot be avoided, increase osimertinib dosage to 160 mg daily; resume dosage of 80 mg daily 3 weeks after rifampin is discontinued |
|
Rosuvastatin |
Increased peak concentrations and AUC of rosuvastatin by 72 and 35%, respectively |
Monitor for adverse effects of rosuvastatin |
|
Simvastatin |
No substantial effect on pharmacokinetics of simvastatin |
Osimertinib Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations attained approximately 6 hours (range 3–24 hours) after oral administration.
Dose-proportional increases in AUC and peak plasma concentration observed over a dose range of 20–240 mg.
Steady-state concentrations are achieved in approximately 15 days.
Food
Administration with a high-fat meal slightly increased AUC and peak plasma concentration by 19 and 14%, respectively; not considered clinically important.
Distribution
Extent
Not known whether distributed into milk. Limited animal data suggest that drug distributes into brain.
Plasma Protein Binding
95%.
Elimination
Metabolism
Principally metabolized by CYP3A.
Metabolized to 2 active metabolites (AZ7550 and AZ5104), each accounting for approximately 10% of total drug exposure.
AZ7550 has a similar potency to parent drug; AZ5104 exhibits higher potency against mutant EGFR and wild-type EGFR.
Elimination Route
Eliminated in feces (68%) and urine (14%); 2% eliminated as unchanged drug.
Half-life
Approximately 48 hours.
Special Populations
Age, weight, gender, smoking status, baseline albumin concentration, line of therapy, and race (Asian versus non-Asian) do not substantially affect pharmacokinetics of osimertinib.
Stability
Storage
Oral
Tablets
25°C (excursions permitted between 15–30°C).
Actions
-
Binds irreversibly and selectively to mutant forms of EGFR including the EGFR-sensitizing mutations (e.g., exon 19 deletion [del19], exon 21 substitution [L858R]) and the secondary T790M mutation.
-
Also inhibits HER2/ErbB2, HER3/ErbB3, HER4/ErbB4, ACK1, and BLK in vitro.
-
Demonstrates antitumor activity against NSCLC cell lines expressing EGFR L858R/T790M, L858R, T790M/del19, and del19 and, to a lesser extent, wild-type EGFR.
-
Exhibits approximately ninefold greater affinity for mutant forms of EGFR than wild-type EGFR.
Advice to Patients
-
Risk of severe or fatal interstitial lung disease/pneumonitis. Importance of immediately informing clinician if new or worsening respiratory symptoms (e.g., difficulty breathing, shortness of breath, cough, fever) occur.
-
Risk of QTc-interval prolongation. Importance of immediately informing clinician if any possible symptoms of QT-interval prolongation (e.g., dizziness, lightheadedness, syncope) occur.
-
Risk of cardiomyopathy. Importance of immediately informing clinician if manifestations of heart failure (e.g., palpitations, shortness of breath, edema) occur.
-
Risk of keratitis. Importance of informing clinician if manifestations of keratitis (e.g., eye inflammation, lacrimation, photosensitivity, eye pain, red eye, changes in vision) occur.
-
Risk of erythema multiforme and Stevens-Johnson syndrome. Importance of promptly informing clinician if target lesions or severe blistering/peeling of the skin occur.
-
Risk of cutaneous vasculitis. Importance of informing clinician if they develop multiple, non-blanching red papules on their extremities or buttocks, or large hives on their trunk that do not resolved within 24 hours and develop a bruised appearance.
-
Risk of aplastic anemia. Importance of informing clinician if signs and symptoms develop such as new or persistent fevers, bruising, bleeding, or pallor.
-
Risk of fetal harm. Advise females of reproductive potential to use effective methods of contraception during therapy and for 6 weeks after drug discontinuance. Advise males with female partners of reproductive potential to use effective methods of contraception during therapy and for 4 months after drug is discontinued. Importance of women informing their clinician if they are pregnant or think they may be pregnant. If pregnancy occurs, advise patient of potential fetal risk.
-
Importance of advising women to avoid breast-feeding while receiving osimertinib therapy and for 2 weeks after the drug is discontinued.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Importance of informing patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care. For further information on the handling of antineoplastic agents, see the ASHP Guidelines on Handling Hazardous Drugs at [Web].
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Osimertinib mesylate can only be obtained through a limited network of specialty distributors. Consult manufacturer's website for additional information.
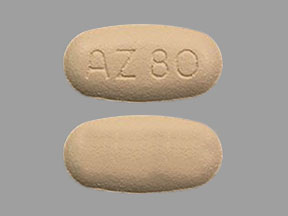
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
40 mg (of osimertinib) |
Tagrisso |
AstraZeneca |
|
80 mg (of osimertinib) |
Tagrisso |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions September 27, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about osimertinib
- Check interactions
- Compare alternatives
- Reviews (42)
- Side effects
- Dosage information
- During pregnancy
- Drug class: EGFR inhibitors
- Breastfeeding
- En español