The originating document has been archived. We cannot confirm the completeness, accuracy, or currency of the content.
Metoclopramide Hydrochloride (Monograph)
Brand names: Gimoti, Reglan
Drug class: Prokinetic Agents
Warning
- Tardive Dyskinesia
-
May result in tardive dyskinesia.5 267 268 269 277 278 Risk increases with increasing duration of therapy and total cumulative dose.5 267 268 269 277 278
-
Discontinue metoclopramide in patients who develop signs or symptoms of tardive dyskinesia.5 267 Symptoms may lessen or resolve in some patients after discontinuance.5 267 268 269 277 278
-
Avoid treatment durations >12 weeks because of increased risk of developing tardive dyskinesia with longer-term use.5 267 268 269 277 278
Introduction
Antiemetic; stimulant of upper GI motility (prokinetic agent); dopamine D2-receptor antagonist.5 267
Uses for Metoclopramide Hydrochloride
Diabetic Gastroparesis
Symptomatic treatment of acute and recurrent diabetic gastric stasis (gastroparesis).5 44 80 267 277 286 287 268 269 292 Therapy should not exceed 12 weeks’ duration because of the risk for developing tardive dyskinesia with longer-term use.5 267 268 269 277 278
Metoclopramide is the only approved drug therapy for diabetic gastroparesis, but evidence supporting its use is weak; given the potential for serious adverse events (e.g., acute dystonic reactions, drug-induced parkinsonism, akathisia, tardive dyskinesia), the American Diabetes Association recommends reserving use for severe cases of diabetic gastroparesis that are unresponsive to other therapies.293 The American College of Gastroenterology (ACG) suggests metoclopramide over no treatment for management of refractory gastroparesis symptoms.294
Cancer Chemotherapy-induced Nausea and Vomiting
Used parenterally for the prevention of nausea and vomiting associated with emetogenic cancer chemotherapy.98 99 100 101 102 144 145 218 267
Has been used orally† [off-label] for the prevention of chemotherapy-induced nausea and vomiting.177 218 264 265 266
No longer routinely used for prophylaxis of chemotherapy-induced nausea and vomiting; other drugs with fewer adverse effects now preferred (some experts state that metoclopramide may still be a reasonable prophylactic option in patients receiving low emetic risk chemotherapy).296 297 298
American Society of Clinical Oncology (ASCO) states metoclopramide may be an option for treatment of breakthrough nausea and vomiting† [off-label] in patients who received prophylactic antiemetic therapy with drugs from a different therapeutic class .263
Intubation of the Small Intestine
Used parenterally to facilitate small intestine intubation in adults and pediatric patients when the tube (e.g., endoscope, biopsy tube) does not pass through the pylorus with conventional maneuvers.105 106 107 109 176 267 299 300
Radiographic Examination of the Upper GI Tract
Used parenterally to stimulate gastric emptying and intestinal transit of barium when delayed emptying interferes with radiographic examination of the stomach and/or small intestine.43 110 184 267
Gastroesophageal Reflux
Short-term (4–12 weeks) relief of symptomatic, documented gastroesophageal reflux in adults who are unresponsive to conventional therapy.5 39 112 116 117 186 188 268 269 278
Use typically reserved for patients with GERD and concomitant gastroparesis.258 273 274 ACG recommends against treatment of GERD with any prokinetic agent (e.g., metoclopramide) unless there is objective evidence of gastroparesis.258 The American Gastroenterological Association (AGA) recommends against the use of metoclopramide for treatment of GERD, and states that prokinetic agents have not been shown to be useful in GERD (but may be useful for concomitant gastroparesis). 273
Other Uses
Prevention of postoperative nausea and vomiting when nasogastric suction is considered undesirable (evidence limited, but may be useful if other dopamine antagonists not available).267 301 302
Has been used for aspiration prophylaxis in patients undergoing anesthesia† [off-label] (routine use not recommended, but may be considered for patients at high risk of aspiration and patients undergoing cesarean delivery or postpartum tubal ligation).307 308
Has been used for the symptomatic treatment of acute and chronic postsurgical gastroparesis† [off-label] following vagotomy and gastric resection or vagotomy and pyloroplasty.31 37 44 49 84 113 114 115 148 149 Has been used for gastroparesis related to other conditions (nondiabetic gastroparesis† [off-label]).294
Has been used for the management of migraine†.284 303 Some experts state that IV metoclopramide may be considered for relief of migraine pain.284
Has been used for breakthrough nausea and vomiting associated with low or minimal emetic risk radiation therapy† .263
Option for the treatment of nausea and vomiting in pregnancy† in patients not responding to first-line antiemetic therapies.309
Has been used for nausea and vomiting due to other causes† (evidence limited).304 Has been used for the management of intractable hiccups†305 and to promote lactation† .139 154 155 167 306
Metoclopramide Hydrochloride Dosage and Administration
General
Patient Monitoring
-
Monitor patients with hepatic impairment for fluid retention and volume overload while receiving metoclopramide.5 269 277 278
-
In patients receiving concomitant drugs with possible diminished GI absorption by metoclopramide, monitor for reduced efficacy.5 269 277 278
-
Monitor blood glucose concentrations and adjust insulin as necessary in patients with insulin-controlled diabetes mellitus.5 269 277 278
Other General Considerations
-
Avoid use of metoclopramide if patients are receiving other drug therapies that are likely to cause tardive dyskinesia (e.g., antipsychotic agents).5 269 277 278
-
Patients with cytochrome-b5 reductase deficiency who receive metoclopramide have an increased risk of methemoglobinemia and/or sulfhemoglobinemia.5 267 268 269 277 278 Patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency who develop metoclopramide-induced methemoglobinemia should not receive methylene blue therapy due to the risk of potentially fatal hemolytic anemia.5 267 268 269 277 278
-
Some formulations of metoclopramide oral solution may contain the dye tartrazine (FD&C yellow No. 5), which may cause allergic reactions including bronchial asthma in susceptible individuals.268
-
Advise patients who must restrict their intake of phenylalanine that the 5- and 10-mg orally disintegrating tablets contain aspartame (metabolized to phenylalanine).278
Administration
Administer orally, intranasally, by direct IV injection or IV infusion, or IM.5 267 277
Metoclopramide therapy, including all dosage forms and routes of administration, should not exceed 12 weeks’ duration because of risk of tardive dyskinesia with longer-term use.5 267 268 269 277 278
Oral Administration
Oral formulations of metoclopramide are recommended for use in adults only.5 268 269 278
Administer orally on an empty stomach (at least 30 minutes before eating) as conventional tablets, oral solution, or orally disintegrating tablets.5 268 269 278 At least one manufacturer states that dose should not be repeated if inadvertently administered with food.278
Orally Disintegrating Tablets
Remove tablet from the blister packaging with dry hands and immediately place it on the tongue.278 Tablet should disintegrate in approximately one minute (range: 10 seconds to 14 minutes); swallow the granules without water.278 Discard any tablet that breaks or crumbles during handling.278
The 5- and 10-mg orally disintegrating tablets contain aspartame (metabolized to phenylalanine).278
Intranasal Administration
Metoclopramide nasal spray is recommended for use in adults only.277
Commercially available in a bottle with a metered-dose spray pump attachment for administration by nasal inhalation.277 For information on administration technique, consult manufacturer's instructions for use.277
Prime the pump prior to first use or if not used for ≥2 weeks.277
IV Administration
Dilution
For direct IV injection, use without further dilution.267
If dose is >10 mg, dilute in 50 mL of a compatible IV solution.267
For IV infusion, manufacturer recommends dilution in 50 mL of 5% dextrose, 0.9% sodium chloride, 5% dextrose and 0.45% sodium chloride, Ringer’s, or lactated Ringer’s injection.267
Manufacturer states that 0.9% sodium chloride injection is preferred because metoclopramide hydrochloride is most stable in this solution.267
Rate of Administration
Direct IV injection: Administer each 10 mg slowly over 1–2 minutes.267 Rapid IV injection may cause transient but intense feelings of anxiety and restlessness, followed by drowsiness.267
IV infusion: Administer slowly over ≥15 minutes.267
IM Administration
Inject without further dilution.267
Dosage
Available as metoclopramide hydrochloride; dosage expressed in terms of metoclopramide.5 267
Metoclopramide therapy, including all dosage forms and routes of administration, should not exceed 12 weeks’ duration because of risk of tardive dyskinesia with longer-term use.5 267 268 269 277 278
Nasal spray delivers 15 mg of metoclopramide per 70-µL metered spray.277 Each bottle contains 9.8 mL of solution, which is sufficient for administration 4 times daily over a period of 4 weeks.277
Pediatric Patients
Intubation of the Small Intestine
IV
Children <6 years of age: Usually, one 0.1-mg/kg dose given by direct IV injection.267
Pediatric patients 6–14 years of age: Usually, one 2.5- to 5-mg dose given by direct IV injection.267
Pediatric patients >14 years of age: Usually, one 10-mg dose given by direct IV injection.267
Adults
Diabetic Gastroparesis
Oral
10 mg 4 times daily, given 30 minutes before meals and at bedtime.5 268 269 278 Maximum recommended dosage is 40 mg daily.5 269 278 Continue for 2–8 weeks, depending on response.5 268 269 278
Intranasal
15 mg (one spray in one nostril) administered 30 minutes before meals and at bedtime.277 Continue for 2–8 weeks, depending on response.277
IV, then Oral
If symptoms are severe or oral use is not feasible, 10 mg 4 times daily, given by direct IV injection 30 minutes before meals and at bedtime.5 267 278 Continued use for up to 10 days may be required until symptoms subside enough to allow oral administration;5 267 278 however, thoroughly assess the risks and benefits prior to continuing therapy.267
IM, then Oral
If symptoms are severe or oral use is not feasible, 10 mg 4 times daily, given by IM injection 30 minutes before meals and at bedtime.5 267 278 Continued use for up to 10 days may be required until symptoms subside enough to allow oral administration;5 267 278 however, thoroughly assess the risks and benefits prior to continuing therapy.267
Cancer Chemotherapy-induced Nausea and Vomiting
Oral
When used for breakthrough nausea and vomiting† in addition to prophylactic antiemetic therapy, metoclopramide dosages of 10–20 mg given every 6 hours as needed have been used.263 296
IV
Manufacturer states that metoclopramide usually is given by IV infusion 30 minutes before administration of chemotherapy, and then repeated every 2 hours for 2 additional doses followed by every 3 hours for 3 additional doses.267 Manufacturer states that initial 2 doses should be 2 mg/kg if highly emetogenic chemotherapy used;267 for less emetogenic drugs or regimens, 1 mg/kg dose may be sufficient.267
When used for breakthrough nausea and vomiting† in addition to prophylactic antiemetic therapy, IV metoclopramide dosages of 10–20 mg given every 6 hours as needed have been used.263 296
Prevention of Postoperative Nausea and Vomiting
IM
Manufacturer states that usual dose is 10 mg administered near the end of the surgical procedure; 20 mg also may be used.267
Intubation of the Small Intestine
IV
Usually, one 10-mg dose given by direct IV injection.267
Radiographic Examination of the Upper GI Tract
IV
Usually, one 10-mg dose given by direct IV injection.267
Gastroesophageal Reflux Disease
Oral
If continuous dosing is required, 10–15 mg 4 times daily, given 30 minutes before meals and at bedtime for 4–12 weeks; base treatment duration on endoscopic evaluation of response.5 269 278 Maximum recommended dosage is 60 mg daily.5 269
For intermittent symptoms or symptoms at specific times of the day, one 20-mg dose before the provocative situation may be preferred to daily administration of multiple doses.5 269 278
Special Populations
Hepatic Impairment
Diabetic Gastroparesis
Oral
Moderate or severe hepatic impairment (Child-Pugh class B or C): 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).5 269 278
Mild hepatic impairment (Child-Pugh class A): Patient may receive usual recommended dosage.5 269 278
Intranasal
Moderate or severe hepatic impairment: Not recommended because dosage cannot be adjusted.277
Mild hepatic impairment: Patient may receive usual recommended dosage.277
Gastroesophageal Reflux Disease
Oral
Moderate or severe hepatic impairment: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).5 269 278
Mild hepatic impairment: Patient may receive usual recommended dosage.5 269 278
Renal Impairment
In patients with Clcr <40 mL/minute, manufacturers of metoclopramide injection recommend an initial parenteral dosage of approximately 50% of the usual dosage.267 Subsequently, increase or decrease dosage according to response and tolerance.267
Diabetic Gastroparesis
Oral
Moderate or severe renal impairment (Clcr <60 mL/minute): 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).5 269 278
End-stage renal disease, including hemodialysis or continuous ambulatory peritoneal dialysis (CAPD): 5 mg twice daily (maximum 10 mg daily).5 269 278
Intranasal
Moderate or severe renal impairment (Clcr <60 mL/minute): Not recommended because dosage cannot be adjusted.277
Mild renal impairment (Clcr ≥60 mL/minute): Patient may receive usual recommended dosage.277
Gastroesophageal Reflux Disease
Oral
Moderate or severe renal impairment (Clcr ≤60 mL/minute): 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).5 269 278
End-stage renal disease, including hemodialysis or CAPD: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg twice daily (maximum 20 mg daily).5 269 278
Geriatric Patients
Reduce initial dosage.5 278 Administer lowest effective dosage.267
Diabetic Gastroparesis
Oral: Initially, 5 mg 4 times daily, given 30 minutes before meals and at bedtime.5 269 278 May titrate to 10 mg 4 times daily based on response and tolerability (maximum 40 mg daily).5 269 278
Intranasal: Metoclopramide nasal spray not recommended as initial therapy in patients ≥65 years of age.277 May switch from an alternative metoclopramide preparation given at a stable dosage of 10 mg 4 times daily to the nasal formulation given at a dosage of 15 mg (one spray in one nostril) given 30 minutes before meals and at bedtime (maximum 4 times daily); continue for 2–8 weeks, depending on response.277
Gastroesophageal Reflux Disease
Oral: Initially, 5 mg 4 times daily, given 30 minutes before meals and at bedtime.5 May titrate to 10–15 mg 4 times daily based on response and tolerability (maximum 60 mg daily).5
Poor CYP2D6 Metabolizers
Metoclopramide elimination may be slower in poor CYP2D6 metabolizers than in intermediate, extensive, or ultra-rapid CYP2D6 metabolizers; poor metabolizers may be at increased risk of dystonic and other adverse reactions.5 269 278 Reduced dosage recommended.5 269 278
IV or IM: Manufacturers make no specific dosage recommendations.267
Diabetic Gastroparesis
Oral: 5 mg 4 times daily, given 30 minutes before meals and at bedtime (maximum 20 mg daily).5 269 278
Intranasal: Metoclopramide nasal spray not recommended because dosage cannot be adjusted.277
Gastroesophageal Reflux Disease
Oral: 5 mg 4 times daily, given 30 minutes before meals and at bedtime, or 10 mg 3 times daily (maximum 30 mg daily).5 269 278
Cautions for Metoclopramide Hydrochloride
Contraindications
-
Concomitant use of other drugs likely to cause extrapyramidal reactions.267
-
History of tardive dyskinesia or dystonic reaction to metoclopramide.5 268 269 277 278
-
Mechanical obstruction or perforation or other situations in which stimulation of GI motility might be dangerous.5 267 269 277 278
-
Pheochromocytoma or other catecholamine-releasing paragangliomas (due to potential for hypertensive/pheochromocytoma crisis).5 267 268 269 277 278
-
Known hypersensitivity to metoclopramide.5 267 268 269 277 278
Warnings/Precautions
Warnings
Tardive Dyskinesia
May cause tardive dyskinesia, a potentially irreversible disorder manifested by involuntary movements of the tongue or face, and sometimes by involuntary movements of the trunk and/or extremities; movements may be choreoathetotic in appearance (see Boxed Warning).5 267 268 269 277 278 Risk of developing tardive dyskinesia is increased in geriatric patients, especially older women, and patients with diabetes mellitus.5 267 268 269 277 278 Risk of developing tardive dyskinesia and likelihood that it will become irreversible increase with duration of therapy and total cumulative dose.5 267 268 269 277 278 Tardive dyskinesia occurs in about 20% of patients receiving the drug for >12 weeks.267 268 278 Avoid treatment durations >12 weeks, including all dosage forms and routes of administration, and reduce dosage in geriatric patients.5 267 269 278 Metoclopramide nasal spray not recommended for initial therapy in geriatric patients.277 Avoid use in patients receiving other drugs that are likely to cause tardive dyskinesia (e.g., antipsychotic agents).5 269 277 278 Discontinue metoclopramide in patients who develop signs or symptoms of tardive dyskinesia.5 267 268 269 277 278 Tardive dyskinesia may remit, either partially or completely, in some patients within several weeks to months after discontinuance.5 267 268 269 277 278 Metoclopramide may suppress or partially suppress signs of tardive dyskinesia, thereby masking the underlying disease process; effect of this suppression on the long-term course of tardive dyskinesia is unknown.5 267 268 269 277 278 Do not use metoclopramide for symptomatic control of tardive dyskinesia.267 268
Other Warnings and Precautions
Other Extrapyramidal Symptoms
In addition to tardive dyskinesia, potential for other extrapyramidal reactions (e.g., acute dystonic reactions, parkinsonian symptoms, akathisia), especially in pediatric patients and adults <30 years of age or when high doses (e.g., IV doses for prophylaxis of cancer chemotherapy-induced nausea and vomiting) are administered.5 267 268 269 277 278 Advise patients to seek immediate medical attention if such symptoms occur and to discontinue metoclopramide. 5 269 277 278
Avoid use in patients receiving other drugs that are likely to cause extrapyramidal reactions (e.g., antipsychotic agents).5 269 277 278
Commonly manifested as acute dystonic reactions or akathisia; stridor and dyspnea (possibly due to laryngospasm) reported rarely.5 267
Generally occur within 24–48 hours after starting therapy.5 267 268 269 277 278
Give diphenhydramine hydrochloride 50 mg IM or benztropine 1–2 mg IM to reverse symptoms.267 268
If akathisia resolves, may consider reinitiating metoclopramide at a lower dosage.5 269 278 Discontinue intranasal metoclopramide if symptoms of akathisia occur.277
Parkinsonian symptoms (e.g., tremor, cogwheel rigidity, bradykinesia, mask-like facies) have occurred.5 267 268 269 277 278 More common during first 6 months of therapy but occur occasionally after longer periods.5 267 268 269 277 278 Symptoms generally subside within 2–3 months following drug discontinuance.5 267 268 269 277 278
Some manufacturers state metoclopramide can be used cautiously in patients with Parkinson’s disease,267 268 while others recommend avoiding use in patients with parkinsonian syndrome and in patients receiving antiparkinsonian drugs due to the potential exacerbation of symptoms.5 269 277 278
Neuroleptic Malignant Syndrome (NMS)
NMS, a potentially fatal symptom complex characterized by hyperpyrexia, muscular rigidity, altered mental status, and autonomic dysfunction, reported with dopamine antagonists.5 267 268 269 277 278 Other symptoms may include elevations in CPK, rhabdomyolysis, and acute renal failure.5 269 277 278 Evaluate patients with these symptoms immediately.5 269 277 278
Has occurred following metoclopramide overdosage in patients receiving concomitant therapy with other drugs associated with NMS.5 269 277 278
Avoid use in patients receiving other drugs associated with NMS (e.g., typical or atypical antipsychotic agents).5 269 277 278
Important to determine whether untreated or inadequately treated extrapyramidal reactions and serious medical illness (e.g., pneumonia, systemic infection) may coexist.5 267 268 269 277 278 In differential diagnosis, consider the possibility of central anticholinergic toxicity, heat stroke, malignant hyperthermia, drug fever, serotonin syndrome, and primary CNS pathology.5 267 268 269 277 278
Immediately discontinue metoclopramide and other drugs not considered essential, provide intensive symptomatic treatment, monitor patient, and treat any concomitant serious medical condition for which specific therapies are available.5 267 268 269 277 278
Depression
Mild to severe depression (including suicidal ideation and suicide) has occurred in patients with or without history of depression who receive metoclopramide.5 267 268 269 277 278
Some manufacturers recommend avoidance of metoclopramide in patients with a history of depression,5 269 277 278 while others state it can be given if expected benefits outweigh expected risks.267 268
Hypertension
May increase BP; increase in circulating catecholamines reported in hypertensive patients.5 269 277 278 Avoid use in patients with hypertension and in those receiving MAO inhibitors.5 269 277 278
Hypertensive crisis reported in patients with undiagnosed pheochromocytoma; discontinue metoclopramide in any patient who has a rapid increase in BP.5 269 277 278
Fluid Retention
Possible transient increases in plasma aldosterone concentrations and sodium retention; closely monitor patients (e.g., those with hepatic impairment, CHF, or cirrhosis) at risk of developing fluid retention and volume overload. 5 267 268 269 277 278
Monitor patients with hepatic impairment for fluid retention and volume overload.5 269 277 278 Discontinue metoclopramide if fluid retention or volume overload occurs at any time during therapy.5 267 268 269 277 278
Hyperprolactinemia
May cause elevations in prolactin levels that persist with long-term administration.268 Hyperprolactinemia may result in impaired gonadal steroidogenesis and inhibition of reproductive function in both females and males.5 269 277 278 Galactorrhea, gynecomastia, amenorrhea, and impotence reported.5 267 269 277 278
Hyperprolactinemia may potentially stimulate prolactin-dependent breast cancer.5 269 277 278 However, some clinical and epidemiologic studies have not shown an association between dopamine D2-receptor antagonists and tumorigenesis in humans.5 269 277 278
Effects on the Ability to Drive and Operate Machinery
Drowsiness may occur, particularly at higher dosages.5 267 268 269 277 278
Performance of activities requiring mental alertness and physical coordination (e.g., operating machinery, driving a motor vehicle) may be impaired.5 267 268 269 277 278 Concomitant use of CNS depressants and drugs that cause extrapyramidal reactions may increase mental and/or physical impairment; avoid such concomitant use.5 267 268 269 277 278
Phenylketonuria
Each 5- or 10-mg orally disintegrating tablet of metoclopramide contains aspartame, which is metabolized in the GI tract to provide 4.7 mg of phenylalanine per tablet.278
Pressure on Suture Lines Following GI Anastomosis or Closure
When deciding whether to use parenteral metoclopramide or NG suction to prevent postoperative nausea and vomiting, consider the possibility that metoclopramide theoretically could produce increased pressure on suture lines following GI anastomosis or closure.267
Specific Populations
Pregnancy
Published studies, including retrospective cohort studies, national registry studies, and meta-analyses, have not revealed an increased risk of adverse pregnancy-related outcomes with metoclopramide use during pregnancy.5 269 277 278
No adverse developmental effects observed in animal studies.5 269 277 278
Crosses the placenta and may cause extrapyramidal reactions and methemoglobinemia in neonates whose mothers received the drug during delivery; monitor for extrapyramidal effects.5 269 277 278
Lactation
Distributed into milk.5 Estimated dose received by breast-fed infants is <10% of the maternal weight-adjusted oral dose.5 269 277 278 In one study, estimated dose from breast milk was 6–24 mcg/kg daily at 3–9 days postpartum and 1–13 mcg/kg daily at 8–12 weeks postpartum.5 269 277 278 Exposure expected to be similar following maternal doses of 10 mg administered orally or 15 mg administered intranasally.277
Adverse GI effects (e.g., intestinal discomfort, increased intestinal gas formation) reported in breast-fed infants exposed to metoclopramide.5 269 277 278
Although metoclopramide increases prolactin concentrations, data are inadequate to support drug-related effects on milk production.5 269 277 278
Consider developmental and health benefits of breast-feeding along with the mother's clinical need for metoclopramide and any potential adverse effects on the breast-fed child from the drug or underlying maternal condition.5 269 277 278
Monitor nursing neonates for extrapyramidal effects (dystonias) and methemoglobinemia.5 269 277 278
Females and Males of Reproductive Potential
Animal reproductive studies using metoclopramide dosages of up to approximately 3 times the maximum recommended human dose (MRHD) have not revealed impaired fertility or altered reproductive performance.5 269 277 278 Menstrual disturbances and impotence have been reported with metoclopramide.5 269 277 278
Pediatric Use
Safety profile in adults cannot be extrapolated to pediatric patients.267 268 Dystonias and other extrapyramidal reactions are more common in pediatric patients than in adults.5 267 268 269
Safety and efficacy of oral and intranasal metoclopramide not established in pediatric patients; these formulations are not recommended for use in pediatric patients because of risk of tardive dyskinesia and other extrapyramidal reactions, as well as risk of methemoglobinemia in neonates.5 268 269 277 278
Safety and efficacy of metoclopramide injection in pediatric patients is established only for use to facilitate intubation of the small intestine.267 Use metoclopramide injection with caution; incidence of extrapyramidal reactions is increased in pediatric patients.267
Use metoclopramide injection with caution in neonates.267 Neonatal susceptibility to methemoglobinemia is increased due to prolonged clearance (may cause excessive serum concentrations) in combination with decreased neonatal levels of cytochrome-b5 reductase.5 267
Geriatric Use
Geriatric patients are more likely to have decreased renal function and may be more sensitive to therapeutic or adverse effects of metoclopramide.5 268 Geriatric patients, especially older women, are at increased risk for tardive dyskinesia.5 267 268 269 277
Risk of adverse parkinsonian effects increases with increasing dosage;5 267 administer lowest effective dosage in geriatric patients.267 268 If parkinsonian symptoms develop, generally should discontinue metoclopramide before initiating specific antiparkinsonian therapy.267 268
Confusion and oversedation may occur.267 268
Substantially eliminated by the kidneys; risk of adverse reactions, including tardive dyskinesia, may be greater in patients with impaired renal function.5 267 268 269 277 278
Consider reduced dosage.5 278 Select dosage with caution, usually initiating therapy at the low end of the dosage range, because of age-related decreases in renal function and concomitant disease and drug therapy.267 268
Hepatic Impairment
Clearance reduced by approximately 50% in patients with severe hepatic impairment (Child-Pugh class C), resulting in increased exposure.5 269 277 278 Possible increased risk of adverse effects.5 269 277 278 Pharmacokinetic data lacking in patients with moderate hepatic impairment (Child-Pugh class B).5 269 277 278 Reduced dosage recommended in patients with moderate to severe hepatic impairment.5 269 277 278 Avoid intranasal metoclopramide in patients with moderate to severe hepatic impairment.277
Possible increased risk of fluid retention in patients with hepatic impairment.5 269 277 278 Monitor for fluid retention and volume overload in patients with hepatic impairment.5 269 277 278
Renal Impairment
Systemic exposure increased approximately 2-fold in patients with moderate or severe renal impairment (Clcr <60 mL/minute) following oral administration.5 269 277 278 In patients with ESRD requiring dialysis, systemic exposure increased approximately 3.5-fold.5 269 277 278 Reduce dosages in patients with moderate to severe renal impairment, including those undergoing hemodialysis or continuous ambulatory peritoneal dialysis.5 278
Avoid intranasal metoclopramide in patients with moderate to severe renal impairment, including those undergoing hemodialysis or peritoneal dialysis.277 Initial parenteral dosage reductions recommended in patients with Clcr<40 mL/minute; subsequently, increase or decrease dosage according to response and tolerance..267
Common Adverse Effects
Oral metoclopramide (>10% of patients): Restlessness, drowsiness, fatigue, lassitude.5 269 278
Parenteral metoclopramide: restlessness, sleepiness, tiredness, dizziness, exhaustion, headache, confusion, difficulty sleeping.267
Intranasal metoclopramide (≥5% of patients): Dysgeusia, headache, and fatigue.277
Drug Interactions
Metabolized by CYP2D6; also conjugated with glucuronic acid and sulfuric acid.5 269 277 278
Orally Administered Drugs
Possible decreased absorption of certain drugs that disintegrate, dissolve, and/or are absorbed mainly in the stomach.267 268
Possible enhanced rate and extent of absorption of drugs mainly absorbed in the small intestine.267 268
Drugs that Impair GI Motility
Possible reduced oral absorption of metoclopramide; monitor for reduced metoclopramide efficacy.5 269 277 278
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP2D6 inhibitors: Possible increased systemic exposure to metoclopramide and exacerbation of extrapyramidal symptoms.5 269 278 Reduce metoclopramide dosage (see Table 1).5 269 278 Examples of potent CYP2D6 inhibitors include, but are not limited to, bupropion, fluoxetine, paroxetine, and quinidine.5 269 278
|
Metoclopramide Route of Administration |
Adult Dosage Recommendation |
|---|---|
|
Oral |
Diabetic gastroparesis: 5 mg given 4 times daily (maximum 20 mg daily)5 269 278 Gastroesophageal reflux: 5 mg given 4 times daily or 10 mg given 3 times daily (maximum 30 mg daily)5 269 278 |
|
Parenteral |
Manufacturers make no specific recommendations267 |
|
Intranasal |
Not recommended; dosage cannot be adjusted to reduce exposure277 |
Drugs Metabolized by Hepatic Microsomal Enzymes
CYP2D6 substrates: In vitro studies suggest metoclopramide can inhibit CYP2D6, but interactions considered unlikely in vivo at clinically relevant concentrations.5 269 278
Drugs with Similar Adverse Effect Profiles
Drugs that are likely to cause extrapyramidal reactions or are known to cause tardive dyskinesia or neuroleptic malignant syndrome (NMS): Possible additive effects; avoid concomitant use.5 267 269 277 278
Dopaminergic Agents
Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine.5 269 277 278 Avoid concomitant use; if concomitant use is required, monitor therapeutic effects.5 269 277 278
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
Possible enhanced rate and extent of acetaminophen absorption267 268 |
|
|
Anticholinergic agents (e.g., atropine) |
Antagonism of GI motility effects of metoclopramide 5 267 Impairment of GI motility by anticholinergic agent may reduce oral absorption of metoclopramide5 269 277 278 |
|
|
Antidiarrheal agents, antiperistaltic |
Impairment of GI motility by antiperistaltic agent may reduce oral absorption of metoclopramide5 269 277 278 |
|
|
Antipsychotic agents (e.g., butyrophenones, phenothiazines) |
Possible additive adverse effects, including increased frequency and severity of tardive dyskinesia, parkinsonian or other extrapyramidal symptoms, and NMS5 269 278 |
|
|
Atovaquone |
||
|
CNS depressants (alcohol, opiates or other analgesics, sedatives or hypnotics, anxiolytic agents, anesthetics) |
Increased CNS depressant effects;5 267 possible enhanced rate and extent of alcohol absorption 5 269 277 278 |
|
|
Cyclosporine |
Possible enhanced rate and extent of cyclosporine absorption267 268 |
Monitor cyclosporine concentrations and adjust cyclosporine dosage as needed5 269 277 278 |
|
Digoxin |
Monitor digoxin concentrations and adjust digoxin dosage as needed5 269 277 278 |
|
|
Dopamine agonists (e.g., apomorphine, bromocriptine, cabergoline, pramipexole, ropinirole, rotigotine) |
Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine5 269 277 278 |
Avoid concomitant use; if concomitant use required, monitor therapeutic effects5 269 277 278 |
|
Fluoxetine |
Increased peak concentration and AUC of metoclopramide by 40 and 90%, respectively; possible exacerbation of extrapyramidal symptoms5 269 277 278 |
Reduce metoclopramide dosage5 (see Table 1) |
|
Fosfomycin |
||
|
Insulin |
Possible alteration of glycemic control secondary to metoclopramide-related changes in the delivery of food to and the rate of absorption in the intestine5 267 269 277 278 |
Monitor blood glucose; adjustment of insulin dose or timing may be necessary5 267 269 277 278 |
|
Levodopa |
Possible enhanced rate and extent of levodopa absorption267 268 Possible reduced efficacy of metoclopramide and possible exacerbation of parkinsonian symptoms due to opposing effects on dopamine5 269 277 278 |
Avoid concomitant use; if concomitant use required, monitor therapeutic effects5 269 277 278 |
|
MAO inhibitors |
Possible hypertensive reaction due to metoclopramide-induced release of catecholamines5 267 268 269 277 278 |
|
|
Neuromuscular blocking agents |
Enhanced neuromuscular blockade due to metoclopramide inhibition of plasma cholinesterase5 269 277 278 |
|
|
Opiate analgesics |
Antagonism of GI motility effects of metoclopramide5 267 268 Impairment of GI motility by opiate may reduce oral absorption of metoclopramide5 269 277 278 |
|
|
Posaconazole |
Posaconazole oral suspension: Possible decreased posaconazole absorption5 269 277 278 Posaconazole delayed-release tablets: Absorption not affected5 269 277 278 |
Posaconazole oral suspension: Monitor for reduced posaconazole efficacy5 269 277 278 |
|
Sirolimus |
Monitor sirolimus concentrations and adjust sirolimus dosage as needed5 269 277 278 |
|
|
Tacrolimus |
Monitor tacrolimus concentrations and adjust tacrolimus dosage as needed5 269 277 278 |
|
|
Tetracycline |
Possible enhanced rate and extent of tetracycline absorption267 268 |
Metoclopramide Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Following oral administration, rapidly and almost completely absorbed.267 268 269 Relative to a 20 mg IV dose, absolute bioavailability of oral metoclopramide is about 80%.5 267 268 269 278 Peak plasma concentration usually attained at 1–2 hours.5 267 268 269
Orally disintegrating tablets are bioequivalent to metoclopramide conventional tablets when administered under fasting conditions in adults.278 Time to peak plasma concentration is delayed from 1.8 to 3 hours and peak concentration is decreased by 17% when orally disintegrating tablets are administered with a high-fat meal compared to the fasted state, although overall absorption is not significantly affected.278 Clinical relevance of a lower peak plasma concentration is not known.278
Following intranasal administration, absolute bioavailability is 47% compared with IV administration.277 Absorption is reduced following intranasal versus oral administration; peak concentration, AUC, and time to reach peak concentration are similar following a 15-mg intranasal dose or a 10-mg oral dose.277
Over an intranasal dose range of 10–80 mg, systemic exposure is proportional to dose.277
Onset
Following oral administration, 30–60 minutes for effects on GI tract.267
Following IM administration, 10–15 minutes for effects on GI tract.267
Following IV administration, 1–3 minutes for effects on GI tract.267
Food
Administration of the orally disintegrating tablets immediately after a high-fat meal did not affect extent of absorption, but decreased peak blood concentration by 17% and increased time to peak concentration to 3 hours (compared with 1.8 hours under fasting conditions).278 Clinical importance of decreased peak concentration is unknown.278
Special Populations
Moderate or severe renal impairment: AUC following oral administration is approximately 2-fold that observed in individuals with normal renal function; in end-stage renal disease requiring dialysis, AUC is approximately 3.5-fold that observed in individuals with normal renal function.5 267 277 278
Females: AUC and peak concentration following intranasal administration are increased by 34 and 42%, respectively, compared with males.277 Clinical relevance unknown.277
Body weight: Following intranasal administration, lower systemic exposure expected in individuals with higher lean body weight (within range of 34–94 kg).277 Clinical relevance unknown.277
Pediatric patients: Pharmacodynamics are highly variable; relationship between drug plasma concentrations and pharmacodynamic effects not established. 267
Infants: Metoclopramide may accumulate in plasma after multiple doses; mean peak plasma concentration was 2-fold higher after tenth dose compared with that after first dose in infants (3.5 weeks–5.4 months of age) with gastroesophageal reflux receiving metoclopramide oral solution.267
Distribution
Extent
Distributed into milk in humans.5 269 277 278
Plasma Protein Binding
30% bound.5 267 268 269 277 278
Elimination
Metabolism
Undergoes enzymatic metabolism via oxidation as well as conjugation with glucuronic acid and sulfuric acid in the liver.5 269 277 278 Monodeethylmetoclopramide, a major oxidative metabolite, is formed mainly by CYP2D6, which is subject to genetic variability.5 269 277 278
Elimination Route
Excreted in urine (85%) within 72 hours following an oral dose;5 267 268 269 277 278 approximately 50% of dose excreted as free or conjugated metoclopramide.267 268 About 18 and 22% of a 10 mg and 20 mg oral dose, respectively, excreted in urine as unchanged drug within 36 hours.5 269 277 278
Minimally removed by hemodialysis or peritoneal dialysis.5 267 268 277
Half-life
In adults with normal renal function, 5–6 hours.5 267 268 Half-life of 8.1 hours reported following intranasal administration.277
In pediatric patients, elimination half-life is about 4.1–4.5 hours.267 268
Special Populations
Renal impairment: Half-life may be prolonged and clearance decreased.267 268
Severe hepatic impairment (Child-Pugh class C): Average clearance following oral administration is reduced by approximately 50% compared with individuals with normal hepatic function.5 269 277 278
Data insufficient to determine whether pharmacokinetics of the drug in pediatric patients are similar to those in adults.267 268
Neonates: Reduced clearance, possibly associated with immature renal and hepatic functions present at birth.5 267 268
Stability
Storage
Nasal
Solution
20–25°C (may be exposed to 15–30°C).277 Discard 4 weeks after opening.277
Oral
Tablets
Tight, light-resistant containers at 20–25°C.5
Tablets, Orally Disintegrating
20–25°C.278 Do not remove from blister pack until immediately before administration.278
Solution
Tight, light-resistant containers at 20–25°C.268 269 Protect from freezing.268
Parenteral
Injection
20–25°C.267 Protect from light.267
Following dilution with 5% dextrose, 0.9% sodium chloride, 5% dextrose and 0.45% sodium chloride, Ringer’s, or lactated Ringer’s injection, store for up to 48 hours (without freezing) when protected from light or for up to 24 hours under normal light conditions (i.e., unprotected from light).267
May be stored frozen for up to 4 weeks following dilution with 0.9% sodium chloride injection.267
Degradation occurs if metoclopramide is diluted in 5% dextrose injection and frozen.267
Actions
-
A dopamine D2-receptor antagonist, an antiemetic, and a stimulant of upper GI motility (prokinetic agent).5 267
-
Mechanism of action in GI disorders not fully elucidated; principal effects involve the GI tract and CNS.5 267 268 269 277 278 Appears to sensitize tissue to the actions of acetylcholine, resulting in stimulation of the upper GI tract, without causing stimulation of gastric, biliary, or pancreatic secretions. 5 267 268 269 277 278
-
Increases gastric contraction tone and amplitude, relaxes the pyloric sphincter and duodenal bulb, and increases peristalsis of the duodenum and jejunum to accelerate gastric emptying and intestinal transit.5 267 268 269 277 278
-
Antiemetic effects likely due to blockade of central and peripheral dopamine receptors, which decreases stimulation of the chemoreceptor trigger zone.267 268
Advice to Patients
-
Provide the patient or caregiver with a copy of the manufacturer’s medication guide.5 267 Instruct patient or caregiver to read and understand the contents of the medication guide before initiating therapy and each time the prescription is refilled.5 267
-
Inform patients that oral and intranasal formulations of metoclopramide are recommended for use in adults only.5 268 269 277 278
-
Instruct patients receiving intranasal metoclopramide therapy on appropriate use of the metered-dose inhaler and provide them with a copy of the manufacturer's instructions for use.277
-
Inform patients of the risk of tardive dyskinesia.5 267 Stress importance of contacting clinician immediately if new, abnormal, involuntary, or uncontrollable muscle movements occur (e.g., lip smacking, chewing, puckering mouth, frowning, scowling, tongue protrusion, blinking, eye movements, arm and leg shaking).5 267 Stress importance of not taking metoclopramide for >12 weeks.5
-
Inform patients of the risk of neuroleptic malignant syndrome (NMS).5 Stress importance of contacting clinician immediately if signs or symptoms of NMS (e.g., high fever, stiff muscles, difficulty thinking, fast or uneven heartbeat, increased sweating) occur.5
-
Inform patients of the risk of dystonic reactions, parkinsonian symptoms, or akathisia.5 Stress importance of contacting clinician immediately if such reactions occur.5
-
Inform patients of the risk of depression and/or suicidality.5 Stress importance of contacting clinician immediately if depression or suicidality occurs.5
-
Inform patients of the potential for drowsiness or dizziness.5
-
Inform patients of the potential for metoclopramide to impair mental alertness or physical coordination; avoid driving or operating machinery until effects on the individual are known.5 267 Advise patients that alcohol, opiate analgesics, sedatives or hypnotics, anxiolytic agents, other CNS depressants, and other drugs that cause extrapyramidal symptoms may enhance such impairment.5 267
-
For patients receiving metoclopramide nasal solution, stress importance of not repeating a dose if uncertain whether the spray entered the nostril and of not administering an extra dose or a double dose to make up for a missed dose; instead, administer the next dose at the regularly scheduled time.277
-
Inform patients with phenylketonuria that metoclopramide orally disintegrating tablets contain aspartame.278
-
Stress importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.5 Advise patients that concomitant use of metoclopramide with many other drugs may precipitate or worsen tardive dyskinesia, extrapyramidal symptoms, NMS, and CNS depression.5 Explain that the prescriber of any other medication must be made aware that the patient is taking metoclopramide. 5 269 277 278
-
Stress importance of patients informing clinicians if they are or plan to become pregnant or plan to breast-feed.5 267
-
Inform patients of other important precautionary information.5
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Nasal |
Solution |
15 mg (of metoclopramide) per metered spray |
Gimoti |
Evoke |
|
Oral |
Solution |
5 mg (of metoclopramide) per 5 mL* |
Metoclopramide Hydrochloride Oral Solution |
|
|
Tablets |
5 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Tablets |
||
|
Reglan |
ANI |
|||
|
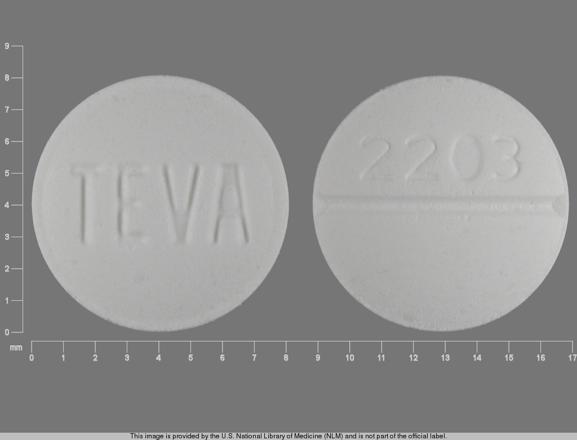
10 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Tablets |
|||
|
Reglan (scored) |
ANI |
|||
|
Tablets, orally disintegrating |
5 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Orally Disintegrating Tablets |
||
|
10 mg (of metoclopramide)* |
Metoclopramide Hydrochloride Orally Disintegrating Tablets |
|||
|
Parenteral |
Injection |
5 mg (of metoclopramide) per mL* |
Metoclopramide Hydrochloride Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
5. ANI Pharmaceuticals. Metoclopramide hydrochloride tablets prescribing information. Baudette, MN; 2021 Jul. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=797aad80-0597-42f8-99d5-39de180c3b5a
31. Stadaas J, Aune S. The effect of metoclopramide (Primperan) on gastric motility before and after vagotomy in man. Scand J Gastroenterol. 1971; 6:17-21. https://pubmed.ncbi.nlm.nih.gov/5100064
37. Hancock BD, Bowen-Jones E, Dixon R et al. The effect of metoclopramide on gastric emptying of solid meals. Gut. 1974; 15:462-7. https://pubmed.ncbi.nlm.nih.gov/4605245
39. Behar J, Biancani P. Effect of oral metoclopramide on gastroesophageal reflux in the post-cibal state. Gastroenterology. 1976; 70:331-5. https://pubmed.ncbi.nlm.nih.gov/765184
43. James WB, Hume R. Action of metoclopramide on gastric emptying and small bowel transit time. Gut. 1968; 9:203-5. https://pubmed.ncbi.nlm.nih.gov/5655030
44. Perkel MS, Moore C, Hersch T et al. Metoclopramide therapy in patients with delayed gastric emptying: a randomized double-blind study. Dig Dis Sci. 1979; 24:662-6. https://pubmed.ncbi.nlm.nih.gov/385260
49. Malagelada JR, Ress WDW, Mazzotta LJ et al. Gastric motor abnormalities in diabetic and postvagotomy gastroparesis: effect of metoclopramide and bethanecol. Gastroenterology. 1980; 78:286-93. https://pubmed.ncbi.nlm.nih.gov/7350052
80. Snape WJ, Battle WM, Schwartz SS et al. Metoclopramide to treat gastroparesis due to diabetes mellitus. Ann Intern Med. 1982; 96:444-6. https://pubmed.ncbi.nlm.nih.gov/7065559
81. Carey RM, Thorner MO, Ortt EM. Effects of metoclopramide and bromocriptine on the renin-angiotensin-aldosterone system in man: dopaminergic control of aldosterone. J Clin Invest. 1979; 63:727-35. https://pubmed.ncbi.nlm.nih.gov/438333
82. Aono T, Shioji T, Kinugasa T et al. Clinical and endocrinological analyses of patients with galactorrhea and menstrual disorders due to sulpiride or metoclopramide. J Clin Endocrinol Metab. 1978; 47:675-80. https://pubmed.ncbi.nlm.nih.gov/122411
83. Campbell IW, Heading RC, Tothill P et al. Gastric emptying in diabetic autonomic neuropathy. Gut. 1977; 18:462-7. https://pubmed.ncbi.nlm.nih.gov/873328
84. Saltzman M, Meyer C, Callachan C et al. Effect of metoclopramide on chronic gastric stasis in diabetic and post-gastric surgery patients. Gastroenterology. 1981; 80:1268.
98. Gralla RJ, Itri LM, Pisko SE et al. Antiemetic efficacy of high-dose metoclopramide: randomized trials with placebo and prochlorperazine in patients with chemotherapy-induced nausea and vomiting. N Engl J Med. 1981; 305:905-9. https://pubmed.ncbi.nlm.nih.gov/7024807
99. Strum SB, McDermed JE, Opfell RW et al. Intravenous metoclopramide: an effective antiemetic in cancer chemotherapy. JAMA. 1982; 247:2683-6. https://pubmed.ncbi.nlm.nih.gov/7043002
100. Carr B, Palone B, Pertrand M et al. A double-blind comparison of metoclopramide (MCP) and proclorperazine (PCP) for cis-platinum (DDP) induced emesis. Proc Am Soc Clin Oncol. 1982; 1:66.
101. Daniels M, Belt RJ. High dose metoclopramide as an antiemetic for patients receiving chemotherapy with cis-platinum. Oncol Nurs Forum. 1982; 9:20-2. https://pubmed.ncbi.nlm.nih.gov/6921788
102. Gralla RJ, Tyson LB, Clark RA et al. Antiemetic trials with high dose metoclopramide superiority over THC, and preservation of efficacy in subsequent chemotherapy courses. Proc Am Soc Clin Oncol. 1982; 1:58.
105. Moshal MG. A rapid jejunal biopsy technique aided by metoclopramide: a double-blind trial with 50 patients. Postgrad Med J. 1973; 49(Suppl 4):87-9.
106. Arvanitakis C, Gonzalez G, Rhodes JB. The role of metoclopramide in peroral jejunal biopsy: a controlled randomized trial. Am J Dig Dis. 1976; 21:880-4. https://pubmed.ncbi.nlm.nih.gov/1015496
107. Cristie DL, Ament ME. A double blind crossover study of metoclopramide versus placebo for facilitating passage of multipurpose biopsy tube. Gastroenterology. 1976; 71:726-8. https://pubmed.ncbi.nlm.nih.gov/786773
109. Bolin TD. The facilitation of duodenal intubation with metoclopramide. Med J Aust. 1969; 1:1078-9.
110. Margieson GR, Sorby WA, Williams HBL. The action of metoclopramide on gastric emptying: a radiological assessment. Med J Aust. 1966; 2:1272-4. https://pubmed.ncbi.nlm.nih.gov/5957603
112. McCallum RW, Ippoliti AF, Cooney C et al. A controlled trial of metoclopramide in symptomatic gastroesophageal reflux. N Engl J Med. 1977; 296:354-7. https://pubmed.ncbi.nlm.nih.gov/319356
113. Stadaas JO, Aune S. Clinical trial of metoclopramide in postvagotomy gastric stasis. Arch Surg. 1972; 104:684-5. https://pubmed.ncbi.nlm.nih.gov/4554726
114. Metzger W, Cano R, Sturdevant RAL. Effect of metoclopramide in chronic gastric retention after gastric surgery. Gastroenterology. 1975; 68:954.
115. McCallum RW, Saltzman M, Meyer C. Effect of metoclopramide in chronic gastric retention after gastric surgery. Clin Res. 1980; 28:765A.
116. Winnan J, Avella J, Callachan C et al. Double-blind trial of metoclopramide versus placebo-antacid in symptomatic gastroesophageal reflux. Gastroenterology. 1980; 78:1292.
117. Bright-Asare P, El-Bassoussi M. Cimetidine, metoclopramide or placebo in the treatment of symptomatic gastroesophageal reflux. J Clin Gastroenterol. 1980; 2:149-56. https://pubmed.ncbi.nlm.nih.gov/7002998
124. ASHP injectable drug information. Metoclopramide. Bethesda, MD: American Society of Health-System Pharmacists; Updated 2024 Aug 24. Accessed 2024 Oct 4. https://injectables.ashp.org
139. Lewis PJ, Devenish C, Kahn C. Controlled trial of metoclopramide in the initiation of breast feeding. Br J Clin Pharmacol. 1980; 9:217-9. https://pubmed.ncbi.nlm.nih.gov/6986894
144. Tyson LB, Clark RA, Gralla RJ. High-dose metoclopramide: control of dacarbazine-induced emesis in a preliminary trial. Cancer Treat Rep. 1982; 66:2108. https://pubmed.ncbi.nlm.nih.gov/7139656
145. Cox R, Newman CE, Leyland MJ. Metoclopramide in the reduction of nausea and vomiting associated with combined chemotherapy. Cancer Chemother Pharmacol. 1982; 8:133-5. https://pubmed.ncbi.nlm.nih.gov/7046974
148. Metzger WH, Cano R, Sturdevant RAL. Effect of metoclopramide in chronic gastric retention after gastric surgery. Gastroenterology. 1976; 71:30-2. https://pubmed.ncbi.nlm.nih.gov/1278647
149. Davidson ED, Hersh T, Iiaun C et al. Use of metoclopramide in patients with delayed gastric emptying following gastric surgery. Am Surg. 1977; 43:40-4. https://pubmed.ncbi.nlm.nih.gov/831608
154. Guzman V, Toscano G, Canales ES et al. Improvement of defective lactation by using oral metoclopramide. Acta Obstet Gynecol Scand. 1979; 58:53-5. https://pubmed.ncbi.nlm.nih.gov/369279
155. Kauppila A, Kivinen S, Ylikorkala O. A dose response relation between improved lactation and metoclopramide. Lancet. 1981; 1:1175-7. https://pubmed.ncbi.nlm.nih.gov/6112526
167. Kauppila A, Kivinen S, Ylikorkala O. Metoclopramide increases prolactin release and milk secretion in puerperium without stimulating the secretion of thyrotropin and thyroid hormones. J Clin Endocrinol Metab. 1981; 52:436-9. https://pubmed.ncbi.nlm.nih.gov/6780593
176. Hradsky M, Stockbrugger R. The effect of metoclopramide (Primperan) during gastroscopic observation of the antrum and the pylorus. Gastrointest Endosc. 1974; 21:55-7. https://pubmed.ncbi.nlm.nih.gov/4452458
177. Garnick MB. Oral metoclopramide and cisplatin chemotherapy. Ann Intern Med. 1983; 99:127. https://pubmed.ncbi.nlm.nih.gov/6683089
184. James WB, Melrose AG. Metoclopramide in gastro-intestinal radiology. Clin Radiol. 1969; 20:57-60. https://pubmed.ncbi.nlm.nih.gov/5774092
186. Fuchs B, Bartolomeo RS. Prevention of meal-induced heartburn and regurgitation with metoclopramide in patients with gastroesophageal reflux. Clin Ther. 1982; 5:179-85. https://pubmed.ncbi.nlm.nih.gov/6760968
188. McCallum RW, Fink SM, Winnan GR et al. Metoclopramide in gastroesophageal reflux disease: rationale for its use and results of a double-blind trial. Am J Gastroenterol. 1984; 79:165-72. https://pubmed.ncbi.nlm.nih.gov/6367434
216. The United States pharmacopeia, 24th rev, and the national formulary, 19th ed. Rockville, MD: The United States Pharmacopeial Convention, Inc; 2000:1097-9.
218. Levitt M, Warr D, Yelle L et al. Ondansetron compared with dexamethasone and metoclopramide as antiemetics in the chemotherapy of breast cancer with cyclophosphamide, methotresate, and fluorouracil. N Engl J Med. 1993; 328:1081-4. https://pubmed.ncbi.nlm.nih.gov/8455665
236. De Mulder PHM, Seynaeve C, Vermorken JB et al. Ondansetron compared with high-dose metoclopramide in prophylaxis of acute and delayed cisplatin-induced nausea and vomiting: a multicenter, randomized, double-blind, crossover study. Ann Intern Med. 1990; 113:834-40. https://pubmed.ncbi.nlm.nih.gov/2146911
238. Italian Group for Antiemetic Research. Ondansetron + dexamethasone vs metoclopramide + dexamethasone + diphenhydramine in prevention of cisplatin-induced emesis. Lancet. 1992; 340:96-99. https://pubmed.ncbi.nlm.nih.gov/1352024
243. Marty M. A comparison of granisetron as a single agent with conventional combination antiemetic therapies in the treatment of cytostatic-induced emesis. The Granisetron Study Group. Eur J Cancer. 1992; 28A(Suppl 1):S12-6.
244. Ohmatsu H, Eguchi K, Shinkai T et al. A randomized cross-over study of high-dose metoclopramide plus dexamethasone versus granisetron plus dexamethasone in patients receiving chemotherapy with high-dose cisplatin. Jpn J Cancer Res. 1994; 85:1151-8. https://pubmed.ncbi.nlm.nih.gov/7829401
245. Heron JF, Goedhals L, Jordaan JP et al. Oral granisetron alone and in combination with dexamethasone: a double-blind randomized comparison against high-dose metoclopramide plus dexamethasone in prevention of cisplatin-induced emesis. The Granisetron Study Group. Ann Oncol. 1994; 5:579-4. https://pubmed.ncbi.nlm.nih.gov/7993831
246. The Granisetron Study Group. The antiemetic efficacy and safety of granisetron compared with metoclopramide plus dexamethasone in patients receiving fractionated chemotherapy over 5 days. J Cancer Res Clin Oncol. 1993; 119:555-9. https://pubmed.ncbi.nlm.nih.gov/8392077
256. Aapro MS. 5-HT3 receptor antagonists: an overview of their present status and future potential in cancer therapy-induced emesis. Drugs. 1991; 551-68.
258. Katz PO, Dunbar KB, Schnoll-Sussman FH, Greer KB, Yadlapati R, Spechler SJ. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol. 2022 Jan 1;117(1):27-56.
263. Hesketh PJ, Kris MG, Basch E, et al. Antiemetics: ASCO Guideline Update. J Clin Oncol. 2020;38(24):2782-2797.
264. Kris MG, Hesketh PJ, Somerfield MR et al. Ondansetron versus metoclopramide, both combined with dexamethasone, in the prevention of cisplatin-induced delayed emesis: the Italian Group for Antiemetic Research. J Clin Oncol. 1997; 15:124-30. https://pubmed.ncbi.nlm.nih.gov/8996133
265. Aapro MS, Thuerlimann B, Sessa C for the Swiss Group for Clinical Cancer Research et al. A randomized double-blind trial to compare the clinical efficacy of granisetron with metoclopramide, both combined with dexamethasone in the prophylaxis of chemotherapy-induced delayed emesis. Ann Oncol. 2003; 14:291-7. https://pubmed.ncbi.nlm.nih.gov/12562658
266. Kris MG, Gralla RJ, Tyson LB et al. Controlling delayed vomiting: double-blind, randomized trial comparing placebo, dexamethasone alone, and metoclopramide plus dexamethasone in patients receiving cisplatin. J Clin Oncol. 1989; 7:108-14. https://pubmed.ncbi.nlm.nih.gov/2642536
267. Avet Pharmaceuticals. Metoclopramide hydrochloride injection prescribing information. East Brunswick, NJ; 2024 May.
268. ANI Pharmaceuticals. Metoclopramide hydrochloride oral solution prescribing information. Baudette, MN; 2019 Nov.
269. Pharmaceutical Associates. Metoclopramide hydrochloride oral solution prescribing information. Greenville, SC; 2023 Mar.
273. Kahrilas PJ, Shaheen NJ, Vaezi MF et al. American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease. Gastroenterology. 2008; 135:1383-1391, 1391.e1-5. https://pubmed.ncbi.nlm.nih.gov/18789939
274. Yadlapati R, Gyawali CP, Pandolfino JE; CGIT GERD Consensus Conference Participants. AGA Clinical Practice Update on the Personalized Approach to the Evaluation and Management of GERD: Expert Review. Clin Gastroenterol Hepatol. 2022 May;20(5):984-994.e1.
277. Evoke Pharma. Gimoti (metoclopramide hydrochloride) nasal spray prescribing information. Solana Beach, CA; 2021 Jan.
278. Lupin Pharmaceuticals. Metoclopramide hydrochloride orally disintegrating tablets prescribing information. Baltimore, MD; 2020 Dec.
284. Orr SL, Friedman BW, Christie S et al. Management of Adults With Acute Migraine in the Emergency Department: The American Headache Society Evidence Assessment of Parenteral Pharmacotherapies. Headache. 2016; 56:911-40. https://pubmed.ncbi.nlm.nih.gov/27300483
286. Parkman HP, Carlson MR, Gonyer D. Metoclopramide nasal spray is effective in symptoms of gastroparesis in diabetics compared to conventional oral tablet. Neurogastroenterol Motil. 2014; 26:521-8. https://pubmed.ncbi.nlm.nih.gov/24372829
287. Parkman HP, Carlson MR, Gonyer D. Metoclopramide Nasal Spray Reduces Symptoms of Gastroparesis in Women, but not Men, With Diabetes: Results of a Phase 2B Randomized Study. Clin Gastroenterol Hepatol. 2015; 13:1256-1263.e1. https://pubmed.ncbi.nlm.nih.gov/25576687
290. Pasricha PJ, Camilleri M, Hasler WL et al. White Paper AGA: Gastroparesis: Clinical and Regulatory Insights for Clinical Trials. Clin Gastroenterol Hepatol. 2017; 15:1184-1190. https://pubmed.ncbi.nlm.nih.gov/28410896
292. McCallum RW, Parkman HP, Fass R, Bhandari BR, Carlson MR, Buck RD. Metoclopramide Nasal Spray in Women with Symptomatic Diabetic Gastroparesis: A Randomized, Double-Blind, Placebo-Controlled Phase 3 Study. Clin Gastroenterol Hepatol. 2023 Nov 2:S1542-3565(23)00866-2.
293. American Diabetes Association Professional Practice Committee. 12. Retinopathy, Neuropathy, and Foot Care: Standards of Care in Diabetes-2024. Diabetes Care. 2024 Jan 1;47(Suppl 1):S231-S243.
294. Camilleri M, Kuo B, Nguyen L, Vaughn VM, Petrey J, Greer K, Yadlapati R, Abell TL. ACG Clinical Guideline: Gastroparesis. Am J Gastroenterol. 2022 Aug 1;117(8):1197-1220.
295. US Food and Drug Administration. How to Request Domperidone for Expanded Access Use. From FDA website. Accessed 2024 October 2. https://www.fda.gov/drugs/investigational-new-drug-ind-application/how-request-domperidone-expanded-access-use
296. Lohr L. Chemotherapy-induced nausea and vomiting. Cancer J. 2008 Mar-Apr;14(2):85-93.
297. Natale JJ. Overview of the prevention and management of CINV. Am J Manag Care. 2018 Oct;24(18 Suppl):S391-S397.
298. Kennedy SKF, Goodall S, Lee SF, DeAngelis C, Jocko A, Charbonneau F, Wang K, Pasetka M, Ko YJ, Wong HCY, Chan AW, Rajeswaran T, Gojsevic M, Chow E, Gralla RJ, Ng TL, Jerzak KJ. 2020 ASCO, 2023 NCCN, 2023 MASCC/ESMO, and 2019 CCO: a comparison of antiemetic guidelines for the treatment of chemotherapy-induced nausea and vomiting in cancer patients. Support Care Cancer. 2024 Apr 10;32(5):280.
299. Ouyang X, Qu R, Hu B, Wang Y, Yao F, Lv B, Sun C, Deng Y, Chen C. Is metoclopramide beneficial for the postpyloric placement of nasoenteric tubes? A systematic review and meta-analysis of randomized controlled trials. Nutr Clin Pract. 2022 Apr;37(2):316-327.
300. Silva CC, Bennett C, Saconato H, Atallah ÁN. Metoclopramide for post-pyloric placement of naso-enteral feeding tubes. Cochrane Database Syst Rev. 2015 Jan 7;1(1):CD003353.
301. Weibel S, Schaefer MS, Raj D, Rücker G, Pace NL, Schlesinger T, Meybohm P, Kienbaum P, Eberhart LHJ, Kranke P. Drugs for preventing postoperative nausea and vomiting in adults after general anaesthesia: an abridged Cochrane network meta-analysis. Anaesthesia. 2021 Jul;76(7):962-973.
302. Gan TJ, Belani KG, Bergese S, Chung F, Diemunsch P, Habib AS, Jin Z, Kovac AL, Meyer TA, Urman RD, Apfel CC, Ayad S, Beagley L, Candiotti K, Englesakis M, Hedrick TL, Kranke P, Lee S, Lipman D, Minkowitz HS, Morton J, Philip BK. Fourth Consensus Guidelines for the Management of Postoperative Nausea and Vomiting. Anesth Analg. 2020 Aug;131(2):411-448.
303. Kirkland SW, Visser L, Meyer J, Junqueira DR, Campbell S, Villa-Roel C, Friedman BW, Essel NO, Rowe BH. The effectiveness of parenteral agents for pain reduction in patients with migraine presenting to emergency settings: A systematic review and network analysis. Headache. 2024 Apr;64(4):424-447.
304. Furyk JS, Meek RA, Egerton-Warburton D. Drugs for the treatment of nausea and vomiting in adults in the emergency department setting. Cochrane Database Syst Rev. 2015 Sep 28;2015(9):CD010106.
305. Polito NB, Fellows SE. Pharmacologic Interventions for Intractable and Persistent Hiccups: A Systematic Review. J Emerg Med. 2017 Oct;53(4):540-549.
306. Breastfeeding Challenges: ACOG Committee Opinion, Number 820. Obstet Gynecol. 2021 Feb 1;137(2):e42-e53.
307. Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective Procedures: An Updated Report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology. 2017 Mar;126(3):376-393.
308. Practice Guidelines for Obstetric Anesthesia: An Updated Report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology. 2016 Feb;124(2):270-300.
309. Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 189: Nausea And Vomiting Of Pregnancy. Obstet Gynecol. 2018 Jan;131(1):e15-e30.
Related/similar drugs
More about metoclopramide
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (524)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: GI stimulants
- Breastfeeding
Patient resources
- Metoclopramide drug information
- Metoclopramide nasal
- Metoclopramide (Injection, Intravenous) (Advanced Reading)
Professional resources
- Metoclopramide monograph
- Metoclopramide Injection (FDA)
- Metoclopramide Oral Solution (FDA)
- Metoclopramide Orally DisintegratingTablets (FDA)
- Metoclopramide Tablets (FDA)