Lorlatinib (Monograph)
Brand name: Lorbrena
Drug class: Antineoplastic Agents
- ALK Inhibitors
- ALK Tyrosine Kinase Inhibitors
- Anaplastic Lymphoma Kinase Inhibitors
- Kinase Inhibitors
- Receptor Tyrosine Kinase Inhibitors
- Tyrosine Kinase Inhibitors
Chemical name: (10R)-7-Amino-12-fluoro-2,10,16-trimethyl-15-oxo-10,15,16,17-tetrahydro-2H-4,8-methenopyrazolo[4,3-h][2,5,11]benzoxadiazacyclotetradecine-3-carbonitrile
Molecular formula: C21H19FN6O2
CAS number: 1454846-35-5
Introduction
Antineoplastic agent; an inhibitor of multiple tyrosine kinases, including anaplastic lymphoma kinase (ALK) and c-ros oncogene-1 (ROS-1).
Uses for Lorlatinib
Non-small Cell Lung Cancer (NSCLC)
Treatment of ALK-positive metastatic NSCLC in adults (designated an orphan drug by FDA for treatment of ALK-positive or ROS-1-positive NSCLC).
Guidelines generally support the use of lorlatinib in the second- or third-line setting in patients with NSCLC previously treated with an ALK inhibitor in the first-line setting.
About 3–7% of patients with NSCLC have ALK-positive disease; such patients typically are nonsmokers or light smokers and younger in age and often have adenocarcinoma.
Resistance mutations in ALK, amplification of gene expression, activation of alternate signaling pathways, and/or progression of brain metastases (because of poor distribution of crizotinib into the CSF) limits long-term therapeutic potential of several ALK inhibitors (e.g., alectinib, ceritinib, crizotinib). Lorlatinib is a brain-penetrant ALK inhibitor; responses to lorlatinib in patients with disease progression while receiving other ALK inhibitors (e.g., alectinib, ceritinib, crizotinib) have included CNS responses.
Lorlatinib Dosage and Administration
General
Pretreatment Screening
-
Confirm presence of ALK-positivity in tumor specimens in patients with metastatic NSCLC.
-
Verify pregnancy status in females of reproductive potential prior to initiating therapy.
-
Assess serum cholesterol and triglyceride concentrations prior to initiating therapy; initiate or optimize antilipemic therapy as clinically indicated.
-
Perform ECG prior to initiating therapy.
-
Assess blood pressure prior to initiating therapy; blood pressure must be controlled prior to initiation of the drug.
-
Assess fasting serum glucose concentrations prior to initiation of the drug.
-
Assess concomitant therapy, including prescription drug, OTC drugs, and dietary or herbal supplements. Concomitant use of lorlatinib with potent inducers of CYP3A is contraindicated
Patient Monitoring
-
Monitor blood pressure after 2 weeks of therapy and then at least monthly during therapy.
-
Monitor serum cholesterol and triglyceride concentrations 1 and 2 months after initiating therapy, and then periodically thereafter. Initiate or optimize antilipemic therapy as clinically indicated.
-
Monitor ECG periodically during therapy.
-
Monitor fasting serum glucose concentration periodically during therapy.
Administration
Oral Administration
Administer once daily at the same time each day without regard to food. Swallow tablets whole; do not crush, chew, or split tablets. Do not take tablets if they are broken, cracked, or otherwise not intact.
If a dose is missed, take the dose as soon as it is remembered unless the next dose is due in ≤4 hours. Do not take 2 doses at the same time to make up for a missed dose. If vomiting occurs after taking a dose, take the next dose at the regularly scheduled time; do not take an additional dose.
Dosage
Adults
NSCLC
Oral
100 mg once daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Dosage Modification for Toxicity
Oral
In the CROWN study, treatment interruption or dosage reduction because of adverse reactions was necessary in approximately 49 or 21%, respectively, of patients receiving lorlatinib at the recommended dosage (most commonly for edema, peripheral neuropathy, cognitive effects, pneumonia, hypercholesterolemia, hypertriglyceridemia, or mood effects). Among previously treated patients, 48% required dosage interruption and 24% required at least one dosage reduction for similar adverse effects.
If dosage reduction is necessary, initially reduce dosage to 75 mg once daily. If further dosage reduction is necessary, reduce dosage to 50 mg once daily. If a dosage of 50 mg once daily is not tolerated, permanently discontinue the drug.
CNS Effects
OralIf grade 1 adverse CNS effects occur, may continue therapy at same dosage or interrupt therapy until recovery to baseline; may resume therapy at same dosage or at next lower dosage.
If grade 2 or 3 adverse CNS effects occur, interrupt therapy until recovery to grade 0 or 1; may resume therapy at next lower dosage.
If grade 4 adverse CNS effects occur, permanently discontinue lorlatinib.
Hyperlipidemia
OralIf grade 4 hypercholesterolemia and/or hypertriglyceridemia (serum cholesterol concentration >500 mg/dL or serum triglyceride concentration >1000 mg/dL) occurs, interrupt therapy and initiate appropriate antilipemic therapy, increase dosage of existing antilipemic therapy, or switch to a new antilipemic therapy. May resume therapy at same dosage upon recovery to grade 2 or less.
If severe hypercholesterolemia and/or hypertriglyceridemia recurs despite optimal antilipemic therapy, resume therapy at next lower dosage.
AV Block
OralIf second-degree AV block occurs, interrupt therapy until PR interval <200 msec; may then resume therapy at the next lower dosage.
If complete AV block occurs, interrupt therapy until a pacemaker is placed or PR interval <200 msec. If a pacemaker is placed, may resume therapy at same dosage. If a pacemaker is not placed, resume therapy at the next lower dosage.
If complete AV block recurs, place a pacemaker or permanently discontinue lorlatinib.
Interstitial Lung Disease/Pneumonitis
OralIf treatment-related interstitial lung disease (ILD)/pneumonitis of any grade occurs, permanently discontinue drug.
Hypertension
OralIf grade 3 hypertension (SBP ≥160 mm Hg or DBP ≥100 mm Hg; elevation requiring medical intervention, >1 antihypertensive drug, or more intensive therapy than previously indicated) occurs, withhold therapy; when hypertension improves to grade 1 or less (SBP <140 mm Hg and DBP <90 mm Hg), may then resume at the same dosage.
If grade 3 hypertension recurs, withhold lorlatinib therapy until hypertension improves to grade 1 or less, and then resume at a reduced dosage. If adequate control of hypertension cannot be achieved with optimal medical management, permanently discontinue drug.
If grade 4 (life-threatening or requires urgent intervention) hypertension occurs, withhold lorlatinib; when hypertension improves to grade 1 or less, may then resume at a reduced dosage or permanently discontinue drug.
If grade 4 hypertension recurs, permanently discontinue drug.
Hyperglycemia
OralIf grade 3 hyperglycemia (serum glucose concentration >250 mg/dL) occurs despite optimal antihyperglycemic therapy occurs, withhold therapy until adequate glycemic control is achieved; may then resume at next lower dosage.
If grade 4 hyperglycemia occurs, withhold therapy until adequate glycemic control is achieved; may then resume at next lower dosage.
Permanently discontinue drug if glycemic control cannot be achieved.
Other Toxicity
OralIf other grade 1 or 2 adverse reaction occurs, may continue therapy at same dosage or the next lower dosage.
If other grade 3 or 4 adverse reaction occurs, interrupt therapy until recovery to grade 2 or less or to baseline; may then resume therapy at the next lower dosage.
Concomitant Use with Drugs Affecting Hepatic Microsomal Enzymes
Oral
Concomitant use of lorlatinib with potent inducers of CYP3A is contraindicated.
Avoid concomitant use with moderate inducers of CYP3A. If concomitant use of a moderate CYP3A inducer cannot be avoided, increase lorlatinib dosage to 125 mg once daily.
Avoid concomitant use with potent inhibitors of CYP3A. If concomitant use of a potent CYP3A inhibitor cannot be avoided, reduce lorlatinib dosage from 100 mg to 75 mg once daily or from 75 mg to 50 mg once daily.
Concomitant use of lorlatinib with fluconazole should be avoided. If concomitant use with fluconazole cannot be avoided, reduce initial dosage of lorlatinib from 100 mg once daily to 75 mg once daily.
Special Populations
Hepatic Impairment
Mild hepatic impairment (total bilirubin not exceeding ULN with AST exceeding ULN, or total bilirubin >1 to 1.5 times ULN with any AST): No dosage adjustment needed.
Moderate or severe hepatic impairment: Recommended dosage not established.
Renal Impairment
Mild or moderate renal impairment (Clcr 30–89 mL/minute): No dosage adjustment needed.
Severe renal impairment (Clcr 15 to <30 mL/minute): Reduce dosage from 100 mg once daily to 75 mg once daily.
Geriatric Patients
No specific dosage recommendations.
Cautions for Lorlatinib
Contraindications
-
Concurrent use of potent CYP3A inducers.
Warnings/Precautions
Serious Hepatotoxicity with Concurrent Use of Potent CYP3A Inducers
Severe hepatotoxicity occurred in most healthy individuals receiving a single dose of lorlatinib with multiple doses of rifampin, a potent CYP3A inducer, during a drug interaction study. Grade 3 or 4 elevations in ALT or AST concentrations occurred in 83% and grade 2 elevations occurred in 8% of individuals who received the drugs concurrently during the study. ALT or AST elevations occurred within 3 days of concomitant administration and returned to within normal limits after a median of 15 days (range: 7–34 days). The median time to recovery was 18 days following grade 3 or 4 elevations and 7 days following grade 2 elevations.
Concomitant use with potent CYP3A inducers is contraindicated. Discontinue potent CYP3A inducers and allow 3 plasma half-lives of the potent CYP3A inducer to elapse prior to initiation of lorlatinib.
Avoid concomitant use with moderate CYP3A inducers.
CNS Effects
A wide variety of adverse CNS effects, including seizures, psychotic effects, and changes in cognitive function (including memory impairment, cognitive disorder, and amnesia), mood (including suicidal ideation/suicidality, irritability, anxiety, depression, and labile affect), speech, mental status, and sleep reported. Median time to first onset of any adverse CNS effect was 1.4 months (range: 1 day to 3.4 years). CNS effects are generally mild and intermittent and improve or resolve upon dosage modification.
Treatment interruption, dosage reduction, or drug discontinuance may be required depending on severity.
Hyperlipidemia
Hypercholesterolemia or hypertriglyceridemia occurred in ≥90% of patients receiving the recommended dosage of lorlatinib in clinical trials; median time to onset was 15 days. Antilipemic therapy was initiated in 83% of patients after a median of 17 days on lorlatinib therapy.
Assess serum cholesterol and triglycerides prior to initiating therapy, 1 and 2 months after initiating therapy, and periodically thereafter. Initiate antilipemic therapy or increase dosage of existing antilipemic therapy in patients with hyperlipidemia. Temporary interruption followed by resumption of lorlatinib therapy at the same or a reduced dosage may be necessary, depending on severity.
AV Block
PR-interval prolongation and AV block may occur. In clinical trials, AV block occurred in 1.9% of lorlatinib-treated patients; 0.2% of these patients experienced grade 3 AV block and underwent pacemaker placement.
Monitor ECG prior to initiating lorlatinib and periodically during therapy. If AV block occurs, interrupt therapy; dosage reduction or placement of a pacemaker may be necessary. If complete AV block recurs in patients without a pacemaker, permanently discontinue lorlatinib.
Interstitial Lung Disease/Pneumonitis
Severe or life-threatening ILD/pneumonitis may occur. In clinical trials, ILD or pneumonitis occurred in 1.9% of patients receiving lorlatinib at a dosage of 100 mg once daily, and grade 3 or 4 ILD or pneumonitis occurred in 0.6% of patients receiving the drug.
Promptly evaluate patients who present with worsening respiratory symptoms indicative of ILD or pneumonitis (e.g., dyspnea, cough, fever). In patients with suspected ILD/pneumonitis, immediately interrupt therapy. Permanently discontinue lorlatinib in patients with treatment-related ILD or pneumonitis of any severity.
Hypertension
Hypertension reported in patients receiving lorlatinib. Median time to onset of hypertension is 6.4 months.
Monitor blood pressure after 2 weeks of treatment and at least monthly thereafter. Control blood pressure prior to initiation of therapy.
Hyperglycemia
Hyperglycemia reported in patients receiving lorlatinib. Median time to onset of hyperglycemia is 4.8 months.
Assess fasting serum glucose prior to initiation of lorlatinib and periodically thereafter. If hyperglycemia occurs, temporary interruption of therapy, dosage reduction, or permanent discontinuance of therapy may be necessary based on severity of hyperglycemia.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; malformations, increased post-implantation loss, and abortion observed in animals.
Avoid pregnancy during therapy. Confirmation of pregnancy status recommended prior to initiation of therapy in females of reproductive potential. Females of reproductive potential should use effective nonhormonal methods of contraception during therapy and for ≥6 months after drug discontinuance. Apprise pregnant females and females of reproductive potential of potential fetal hazard.
Males with female partners of reproductive potential should use effective methods of contraception during therapy and for ≥3 months after drug discontinuance.
Specific Populations
Pregnancy
May cause fetal harm.
Lactation
Not known whether lorlatinib or its metabolites are distributed into milk or if drug has any effect on milk production or the nursing infant. Females should not breast-feed during therapy and for 7 days after drug discontinuance.
Females and Males of Reproductive Potential
Females of reproductive potential should use effective nonhormonal methods of contraception during therapy and for ≥6 months after drug discontinuance.
Males with female partners of reproductive potential should use effective methods of contraception during therapy and for ≥3 months after drug discontinuance.
Based on animal studies, may transiently impair male fertility.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
In clinical trials, 18–40% of patients receiving therapy were ≥65 years of age; no clinically important differences in safety or efficacy observed between geriatric patients and younger adults.
Hepatic Impairment
Mild hepatic impairment (total bilirubin not exceeding ULN with AST exceeding ULN, or total bilirubin >1 to 1.5 times ULN with any AST): Pharmacokinetics not substantially altered; no dosage adjustment needed.
Moderate or severe hepatic impairment: Pharmacokinetics not studied.
Renal Impairment
Mild or moderate renal impairment (Clcr 30–89 mL/minute): Pharmacokinetics not substantially altered; no dosage adjustment needed.
Severe renal impairment (Clcr 15 to <30 mL/minute): Pharmacokinetics not studied. Reduce dosage of lorlatinib to 75 mg once daily.
Common Adverse Effects
Adverse effects (≥20%): Edema, peripheral neuropathy, weight gain, cognitive effects, fatigue, dyspnea, arthralgia, diarrhea, mood effects, cough.
Laboratory abnormalities (≥20%): Hypercholesterolemia, hypertriglyceridemia, hyperglycemia, increased AST or ALT concentrations, hypoalbuminemia, anemia, thrombocytopenia, lymphopenia, increased lipase or amylase concentrations, increased alkaline phosphatase concentrations, hypophosphatemia, hyperkalemia, hypomagnesemia.
Drug Interactions
Metabolized principally by CYP3A4 and UGT 1A4, with minor contributions by CYP isoenzymes 2C8, 2C19, and 3A5 and UGT1A3.
In vitro, inhibits (in a time-dependent manner) and induces CYP3A and activates pregnane X receptor (PXR); net effect is induction in vivo. Induces CYP2B6 and activates the human constitutive androstane receptor (CAR).
Inhibits P-glycoprotein (P-gp), organic cation transporter (OCT) 1, organic anion transporter (OAT) 3, multidrug and toxin extrusion (MATE) 1, and intestinal breast cancer resistance protein (BCRP).
Lorlatinib and its major metabolite M8 do not inhibit CYP isoenzymes 1A2, 2B6, 2C8, 2C9, 2C19, or 2D6 nor UGT isoenzymes 1A1, 1A4, 1A6, 1A9, 2B7, or 2B15. M8 does not inhibit CYP3A nor induce CYP isoenzymes 1A2, 2B6, and CYP3A.
Lorlatinib does not inhibit organic anion transporting polypeptide (OATP) 1B1, OATP1B3, OAT1, OCT2, MATE2K, and systemic BCRP. M8 does not inhibit P-gp, BCRP, OATP1B1, OATP1B3, OAT1, OAT3, OCT1, OCT2, MATE1, and MATE2K.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP3A inducers: Risk of severe hepatotoxicity. Concomitant use contraindicated. In addition, possible decreased peak plasma concentration and exposure of lorlatinib. Discontinue potent CYP3A inducers and allow 3 plasma half-lives of the potent CYP3A inducer to elapse prior to initiation of lorlatinib.
Moderate CYP3A inducers: Risk of hepatotoxicity not known. Avoid concomitant use. If concomitant use cannot be avoided, increase dosage of lorlatinib to 125 mg once daily.
Potent CYP3A inhibitors: Possible increased plasma concentrations of lorlatinib, which may increase incidence and severity of adverse effects. Avoid concomitant use. If concomitant use cannot be avoided, reduce dosage of lorlatinib from 100 mg to 75 mg once daily or from 75 mg to 50 mg once daily. If the potent CYP3A inhibitor is discontinued, allow 3 plasma half-lives of the potent CYP3A inhibitor to elapse, then resume the lorlatinib dosage that was tolerated prior to initiation of the potent CYP3A inhibitor.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP3A: Possible decreased plasma concentrations and reduced efficacy of the CYP3A substrate.
Avoid concomitant use with CYP3A substrates where minimal concentration changes may result in serious therapeutic failure. If concomitant use cannot be avoided, the CYP3A substrate may require dosage adjustment; consult specific product labeling of the CYP3A substrate.
Drugs Affected by Transport Systems
Substrates of P-gp or UGT1A: Possible decreased plasma concentrations and reduced efficacy of the P-gp or UGT1A substrate.
Avoid concomitant use of lorlatinib and P-gp substrates with a narrow therapeutic index. If concomitant use cannot be avoided, consult manufacturer's labeling of the P-gp substrate for dosage recommendations.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
Decreased AUC and peak plasma concentration of acetaminophen (a UGT1A substrate) |
|
|
Bupropion |
Decreased AUC and peak plasma concentration of bupropion (a CYP2B6 substrate) |
|
|
Contraceptives, hormonal |
Possible reduced efficacy |
Use effective nonhormonal contraception during and for ≥6 months after discontinuing lorlatinib therapy |
|
Fexofenadine |
Decreased AUC and peak plasma concentrations of fexofenadine (a P-gp substrate) |
|
|
Fluconazole |
Increased plasma concentrations of lorlatinib |
Avoid concomitant use; if concomitant use cannot be avoided, decrease lorlatinib dosage from 100 mg once daily to 75 mg once daily |
|
Itraconazole |
Increased peak plasma concentrations and AUC of lorlatinib |
Avoid concomitant use; if concomitant use cannot be avoided, reduce dosage of lorlatinib from 100 mg to 75 mg once daily or from 75 mg to 50 mg once daily If itraconazole is discontinued, allow 3 plasma half-lives of itraconazole to elapse, then resume the lorlatinib dosage that was tolerated prior to initiation of itraconazole |
|
Midazolam |
Decreased peak plasma concentration and AUC of orally administered midazolam (a CYP3A substrate) |
Avoid concomitant use with CYP3A substrates where minimal concentration changes may result in serious therapeutic failure If concomitant use cannot be avoided, the CYP3A substrate may require dosage adjustment; consult specific product labeling of the CYP3A substrate |
|
Rabeprazole |
No clinically important effect on pharmacokinetics of lorlatinib |
|
|
Rifampin |
Possible hepatotoxicity; grade 3 or 4 elevations in serum ALT and/or AST concentrations occurred within 3 days of concomitant administration Decreased peak plasma concentration and AUC of lorlatinib |
Concomitant use contraindicated Discontinue rifampin and allow 3 plasma half-lives of rifampin to elapse prior to initiation of lorlatinib therapy |
|
Tolbutamide |
Decreased AUC and peak plasma concentrations of tolbutamide (a CYP2C9 substrate) |
Lorlatinib Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations attained at a median of 1.2 hours (range: 0.5–4 hours) following single-dose oral administration and 2 hours (range: 0.5–23 hours) following multiple-dose oral administration at steady state.
Mean absolute bioavailability is 81%.
Steady-state peak plasma concentration is dose proportional and systemic exposure is slightly less than dose proportional over an oral dosage range of 10–200 mg once daily.
Food
High-fat, high-calorie meal does not substantially affect pharmacokinetics of lorlatinib.
Special Populations
Mild hepatic impairment does not substantially affect pharmacokinetics of lorlatinib.
Moderate or severe hepatic impairment: Effect on pharmacokinetics not known.
Mild or moderate renal impairment does not substantially affect pharmacokinetics of lorlatinib.
Severe renal impairment: AUC increased by 42% in patients with Clcr 15 to <30 mL/minute compared with those with normal renal function (Clcr ≥90 mL/minute).
End-stage renal disease or those receiving dialysis: Effects on pharmacokinetics not known.
Age (19–85 years), sex, race/ethnicity, body weight, and CYP3A5 or CYP2C19 metabolizer phenotype do not substantially affect lorlatinib pharmacokinetics.
Distribution
Extent
Distributed into CSF at a CSF-to-plasma ratio of 0.75.
Not known whether lorlatinib or its metabolites distribute into human milk.
Plasma Protein Binding
66%.
Elimination
Metabolism
Metabolized principally by CYP3A4 and UGT1A4, with minor contributions by CYP 2C8, 2C19, and 3A5, and UGT1A3.
Major metabolite, M8, is pharmacologically inactive.
Oral clearance of lorlatinib is higher at steady state than following a single dose, suggesting autoinduction occurs.
Elimination Route
Eliminated in urine (48%; <1% as unchanged drug) and feces (41%; about 9% as unchanged drug).
Half-life
24 hours.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).
Actions
-
Inhibits multiple tyrosine kinases, including ALK and ROS-1 as well as TYK1, FER, FPS, TRKA, TRKB, TRKC, FAK, FAK2, and ACK.
-
Inhibits phosphorylation of ALK and ALK-mediated signal transduction, specifically, STAT3, AKT, ERK, and S6.
-
Activating mutations or translocations of the ALK gene identified in several malignancies and can result in the expression of oncogenic fusion proteins (e.g., echinoderm microtubule-associated protein-like 4 [EML4]-ALK). Formation of ALK fusion proteins results in activation and dysregulation of the gene's expression and signaling, which can contribute to increased cell proliferation and survival in tumors expressing these proteins.
-
ALK rearrangements identified in approximately 3–7% of patients with NSCLC.
-
Clinical resistance to crizotinib attributed to several mechanisms, including acquired resistance mutations of ALK, amplification of gene expression, and activation of alternate signaling pathways. More potent ALK inhibitors (e.g., alectinib, ceritinib) were developed to overcome resistance to crizotinib; however, resistance to these drugs also develops over time.
-
CNS is a common site of disease progression in crizotinib-treated patients because of poor distribution of the drug into CSF.
-
Lorlatinib demonstrates greater potency than alectinib, ceritinib, and crizotinib in its activity against wild-type ALK in vitro and is active against cell lines expressing ALK mutations that confer resistance to crizotinib, including G1202R (which also confers resistance to alectinib and ceritinib), G1269A, and L1196M.
-
Exhibits dose-dependent antitumor activity in mice bearing NSCLC tumor xenografts expressing EML4-ALK fusions with ALK variant 1 or ALK mutations, including G1202R and I1171T mutations that were detected in tumors of patients at the time of disease progression during therapy with other ALK inhibitors.
-
Demonstrates antitumor activity and prolonged survival in mice bearing intracranial EML4-ALK-positive tumor xenografts. Demonstrated antitumor activity in patients with CNS metastases who had received prior treatment with ALK inhibitors (e.g., alectinib, ceritinib, crizotinib).
Advice to Patients
-
Importance of reading the manufacturer's patient information.
-
Importance of advising patients to take lorlatinib exactly as prescribed and of not altering the dosage or discontinuing therapy unless advised to do so by their clinician. Importance of advising patients to swallow lorlatinib tablets whole without regard to food and not to crush, chew, or split the tablets. If a dose is missed, the missed dose should be taken as soon as possible unless it is within 4 hours of the next dose, in which case the missed dose should not be taken. Inform patients to not take 2 doses at the same time to make up for a missed dose. If vomiting occurs after taking a dose, the next dose should be taken at the regularly scheduled time; an additional dose should not be taken.
-
Risk of severe hepatotoxicity when used concomitantly with potent CYP3A inducers.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription drugs (e.g., antilipemic agents, rifampin, oral contraceptives), OTC drugs, and dietary or herbal supplements (e.g., St. John's wort), as well as any concomitant illnesses (e.g., history of depression or other mood disorders, hyperlipidemia, cardiac arrhythmias, pulmonary disease).
-
Risk of adverse CNS effects. Patients should notify their clinician if they experience new or worsening CNS symptoms such as changes in cognitive function or mood, suicidal ideation, hallucinations, or seizures.
-
Risk of hyperlipidemia. Importance of informing patients about the need for monitoring serum cholesterol and triglyceride concentrations during therapy. Advise patients that initiation of antilipemic therapy or an increase in the dosage of existing antilipemic agents may be required.
-
Risk of AV block. Importance of patients immediately contacting their clinician if they experience new or worsening cardiac symptoms such as dizziness, faintness, or arrhythmia during therapy.
-
Risk of severe or life-threatening ILD/pneumonitis. Importance of advising patients that symptoms may be similar to those of lung cancer and to contact their clinician immediately if they experience any new or worsening respiratory symptoms (e.g., dyspnea or shortness of breath, cough, fever).
-
Risk of hypertension. Importance of advising patients to monitor blood pressure regularly. Advise patients that initiation or optimization of blood pressure medications may be necessary during lorlatinib therapy. Importance of immediately informing clinician if signs or symptoms of hypertension, including headaches, dizziness, blurred vision, chest pain, or shortness of breath occur.
-
Risk of hyperglycemia. Importance of advising patients that regular monitoring of blood glucose may be needed prior to and during treatment with lorlatinib. Patients should be advised of the possible need to change or start medications for hyperglycemia. Importance of informing clinician of new or worsening signs and symptoms of hyperglycemia, including increased thirst, increased need to urinate,increased hunger, nausea, weakness or tiredness, or confusion.
-
Risk of fetal harm. Necessity of advising females of reproductive potential that they should use effective, nonhormonal methods of contraception while receiving lorlatinib and for ≥6 months after discontinuance of therapy and of also advising such females that oral contraceptives and other hormonal forms of contraception may not be effective during lorlatinib therapy. Importance of advising males with female partners of reproductive potential to use effective methods of contraception while receiving the drug and for ≥3 months after the drug is discontinued. Importance of also advising males of reproductive potential that lorlatinib may transiently impair fertility and to discuss any concerns about fertility with their clinician.
-
Importance of females informing their clinicians if they are or plan to become pregnant. Advise of potential fetal risk.
-
Importance of advising females to avoid breast-feeding while receiving lorlatinib and for 7 days after discontinuance of therapy.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Lorlatinib is available through specialty pharmacies. Clinicians may consult the Lorbrena website for specific information regarding distribution of the drug.
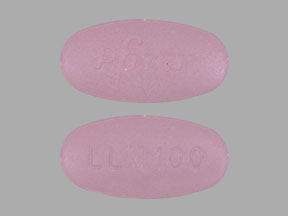
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
25 mg |
Lorbrena |
Pfizer |
|
100 mg |
Lorbrena |
Pfizer |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 29, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about lorlatinib
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: multikinase inhibitors
- Breastfeeding
- En español