Chronic Pain
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is chronic pain?
Chronic pain is pain that does not get better for 3 months or longer. Chronic pain may hurt all the time, or come and go.
How is chronic pain diagnosed?
Your healthcare provider will ask where your pain is, what it feels like, and when it started. Your provider will ask how your pain is affecting your daily life, your mood, and your sleep. Tell your provider if anything helps your pain or makes it worse. You may need any of the following:
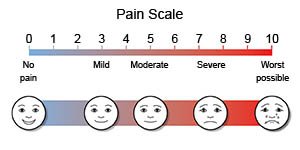
- Pain scales use numbers or faces to help you describe how bad your pain is. Your healthcare provider may ask you to rate your pain on a scale of 0 to 10.
- An x-ray, ultrasound, CT, or MRI may show the cause of your chronic pain. You may be given contrast liquid to help the area show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- Stimulation tests may help to find which nerves or muscles are affected by pain. These tests may include nerve conduction or muscle function studies.
How is chronic pain treated?
- Medicines:
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine called narcotics or opioids may be given for certain types of chronic pain. Ask your healthcare provider how to take this medicine safely.
- Anesthetics can be rubbed on your skin or injected into a nerve or muscle to numb an area.
- Other medicines may reduce pain, anxiety, muscle tension, or swelling.
- Transcutaneous electrical nerve stimulation (TENS) gives you mild, safe electrical signals through a small device attached to your skin.
- Surgery may be done to implant a device that releases pain medicine into your body. Other devices stimulate your nerves with safe electrical signals.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What else can I do to manage chronic pain?
- Apply heat on the area in pain for 20 to 30 minutes every 2 hours for as many days as directed. Heat helps decrease pain and muscle spasms.
- Apply ice on the part of your body that hurts for 15 to 20 minutes every hour or as directed. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel. Ice decreases pain and swelling, and helps prevent tissue damage.
- Go to physical therapy as directed. A physical therapist teaches you exercises to help improve movement and strength, and to decrease pain.
- Exercise for 30 minutes, 3 times a week. Regular physical activity can help decrease pain and improve your quality of life. Ask your healthcare provider about the best exercise plan for your type of pain.
- Get enough sleep. Create a relaxing bedtime routine. Go to sleep and wake up at the same time every day. Avoid caffeine in the afternoon.
- Talk with a counselor or therapist. A type of counseling called cognitive behavioral therapy (CBT) can help your chronic pain by changing the way you think about it. CBT can also improve your mood, sleep, and ability to move.
What do I need to know if I take prescription pain medicine?
- You may need to take a bowel movement softener. The most common side effect of prescription pain medicine is constipation. Bowel movement softeners are available over the counter.
- Do not mix prescription pain medicines. This can cause an overdose of medicine, which can become life-threatening. Read labels. Make sure you know the ingredients in all of your medicines.
- Do not drink alcohol when you take prescription pain medicine. It is not safe to mix narcotics or opioids with alcohol or illegal drugs.
- Prescription pain medicine may impair your ability to drive or work safely. They may also cause dizziness and increase your risk for falling.
- Store prescription pain medicine in a safe location at home. Keep your medicine away from children and other people. Never share your medicine with anyone.
Call your local emergency number, or have someone else call (911 in the US) if:
- You are breathing slower than normal, or you have trouble breathing.
- You cannot be awakened.
- You have a seizure.
When should I call my doctor?
- Your heart feels like it is jumping or fluttering.
- You cannot think clearly.
- You have side effects from prescription pain medicine, such as itching, nausea, or vomiting.
- You have trouble sleeping.
- Your pain gets worse, even after you take medicine.
- You don't think the medicine is working.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Chronic Pain
- Pain Management: Types of Pain and Treatment Options
- Top 9 Things You Must Know About Naproxen
- Tramadol - Top 8 Things You Need to Know
- What are the risks of mixing pain medications and alcohol?
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
